Translate this page into:
The link between serum vitamin D levels and bronchial asthma: A case control study
*Corresponding author: Dr. Pavan N Kumar, Department of Respiratory Medicine, Kempegowda Institute of Medical Sciences and Research Centre VV Puram, Bangalore, India. pkreddy24297@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar PN, Amirullah A, Kumar D. The link between serum vitamin D levels and bronchial asthma: A case control study. Ann Natl Acad Med Sci (India). 2025;61:118-21. doi: 10.25259/ANAMS_206_2024
Abstract
Objectives
Asthma is a common long-term respiratory condition that considerably increases morbidity worldwide. Because of its immunomodulatory properties, vitamin D may have an impact on the severity of asthma. This case control study explores the relationship between serum vitamin D levels and bronchial asthma.
Material and Methods
There were 70 participants in all, 35 of whom were matched controls and 35 of whom were asthma patients. Measurements of IgE and serum vitamin D were made to look for associations with asthma.
Results
Patients with asthma had higher IgE levels, suggesting heightened allergic reaction and substantially less vitamin D in their blood (13.83 ± 9.34 ng/mL) than control (27.34 ± 8.19 ng/mL) (p < 0.001).
Conclusion
This study highlights that individuals with bronchial asthma tend to have lower serum vitamin D levels and higher IgE levels, suggesting a link between vitamin D deficiency and asthma severity. Addressing vitamin D deficiency may offer a supportive role in asthma management, though further studies are needed to confirm these findings.
Keywords
Bronchial Asthma
IgE levels
Vitamin D levels
INTRODUCTION
Millions of people worldwide have bronchial asthma, a chronic condition marked by symptoms like dyspnea, tightness in the chest, wheezing, and fluctuating airflow blockage.1,2 With more than 300 million individuals impacted globally and over 30 million in India alone, it is especially pervasive.3,4 Variables like hypercapnia and hypoxia frequently signal the severity of asthma. A positive atopic status, allergen exposure, and a family history of allergy disorders are risk factors. In addition to being necessary for the regulation of calcium and phosphate, vitamin D is important for immunological modulation or cell differentiation.5,6 An increasing amount of data points to a global epidemic of vitamin D deficiency, which has been linked to the exacerbation of asthma symptoms. Poor nutrition, insufficient sun exposure, prolonged breastfeeding sans supplementation, or maternal deficiency are some of the factors that contribute to this deficiency.7 The purpose of this study was to investigate the potential link between vitamin D levels in the serum on asthma, specifically looking at how a deficiency may exacerbate the condition.
MATERIAL AND METHODS
We enrolled 35 patients having bronchial asthma and 35 sex-, age-, and BMI-matched control subjects, ranging in age from 20 to 67, in our first case-control research. Participants were drawn from the medicine ambulatory department; those in the control group were people who were there for unrelated, minor medical conditions but did not exhibit symptoms of asthma. Asthma patients were confirmed based on eosinophilia in blood smears, where control participants were evaluated through clinical examination to rule out asthma. Type 1 diabetes, malnutrition based on protein-energy intake, or recent consumption of drugs or supplements influencing vitamin D levels were among the exclusion criteria. Furthermore, the study excluded those with long-term liver, kidney, lung, and neurological conditions.
Venous blood samples of about 5 mL were taken from the patients and the controls. As soon as the nonfasting serum samples were collected, routine biochemical parameters were examined for both groups. In addition, aliquots of all the samples were kept at −20°C in order to test for IgE or 25-hydroxyvitamin D levels.
To assess the levels of IgE or 25-hydroxyvitamin D, commercial immunoassay enzyme linked immunosorbent assay kits were used. Student’s t-test was used to do statistical analysis on the various biochemical parameters. The standard deviation, or mean ± SD, was used to express the results. The Mann–Whitney U test was used to assess nonparametric data, while the Student’s unattached two-tailed t-test was used to compare means of two distributed sample groups. With SPSS software, every statistical test was carried out. It was deemed significant when p<0.05.
RESULTS
Our study compares the metabolic profiles and participant characteristics in the bronchial asthma unit (n = 35) with the control group (n = 35). There were 15 men and 20 women in the placebo group and 17 men and 18 women in the asthma group, respectively, according to sex distribution. The control group had an average age of 39.64 ± 13.1 years, while the asthma group had an average age of 38.94 ± 12.69 years. The asthma group had an upper body mass index (BMI) of 24.96 ± 2.29 kg/m2, which was marginally higher than the control group’s BMI of 23.27 ± 1.46 kg/m2 [Table 1].
| Control (n=35) means ± SD | Bronchial Asthma (n=35) means ± SD | |
|---|---|---|
| Sex | ||
| Male | 15 | 17 |
| Female | 20 | 18 |
| Age (in years) | 39.64 ± 13.1 | 38.94 ± 12.69 |
| BMI (kg/m2) | 23.27 ± 1.46 | 24.96 ± 2.29 |
| Serum IgE (IU/L) | 141.8 ± 71.06 | 665.2 ± 245.3* |
| RBS (mg/dl) | 85.13 ± 10.42 | 80.7 ± 12.28 |
RBS: Random blood sugar. Age, BMI, and serum levels of biochemical parameters were expressed as the means ± SD. Statistically significant, *p<0.05 vs. Control. SD: Standard deviation, BMI: Body mass index.
The asthma group had significantly greater serum IgE levels (665.2 ± 245.3 IU/L) than the control sample (141.8 ± 71.06 IU/L), which is a measure of allergic reaction. Nonetheless, there was no noteworthy distinction in the random blood sugar readings between the asthma unit (80.7 ± 12.28 mg/dL) and the control group (85.13 ± 10.42 mg/dL). In patients with bronchial asthma, plasma 25-hydroxyvitamin D levels were considerably lower than in controls (13.83 ± 9.34 ng/mL vs. 27.34 ± 8.19 ng/mL; p < 0.001) [Figure 1].
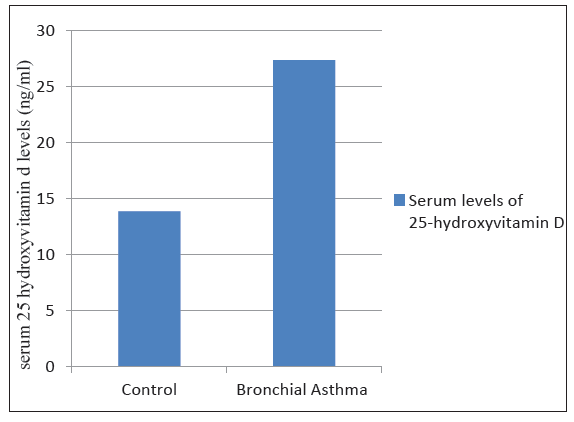
- Serum 25-hydroxy vitamin D levels were significantly lower in bronchial asthma patients compared to controls (p<0.001).
These results show that blood IgE levels are higher in people with bronchial asthma than in nonasthmatics, suggesting that asthma patients have a more sensitive allergic reaction. While both groups’ BMIs were within normal levels, the asthma group’s BMI was marginally higher.
DISCUSSION
It is important to consider that seasonal variations affect vitamin D synthesis due to differing sunlight exposure across seasons, which may impact serum vitamin D levels and influence asthma outcomes. Future studies should account for these variations to provide a more accurate assessment.8
Vitamin D’s role in asthma may be linked to its immunomodulatory effects. It can influence immune cells like monocytes, macrophages, and lymphocytes, potentially reducing airway inflammation and controlling immune responses in asthma. This immunomodulation may help alleviate asthma symptoms and improve patient outcomes.9
A number of causes, including increasing indoor activity, poor food, restricted sun exposure, sunscreen use, and biological characteristics like skin melanin content, that decrease the skin’s capacity to synthesize vitamin D3, have contributed to the rise in vitamin D deficiency as a major global health concern. This shortage affects people of all ages in India.10 A correlation has been shown in studies involving vitamin D deficiency or an increased risk of allergic reactions and asthma. Asthma and high blood IgE levels have even been linked to vitamin D insufficiency in some studies, and vitamin D deficiency in families may be a risk factor for asthma.3
In our investigation, we observed higher IgE levels and a significant decrease in the amount of serum vitamin D among individuals with bronchial asthma when compared with the control group. The significance of vitamin D in the development of asthma is explained by several theories. Vitamin D has the capacity to alter immune cell activity, such as that of monocytes, macrophages, lymphocytes, and even epithelial cells. This could exacerbate asthma symptoms. This shows that inadequate vitamin D may exacerbate immunological dysregulation and asthma-related inflammation or immune responses.11
Our results are consistent with a research by Li et al. (2011) that involved 435 adults with asthma (268 women and 167 men), and they showed lower levels of 25(OH)D.12 Similar to our findings, Shaaban and Hashem’s study involving 75 persons without asthma and 75 normal controls revealed vitamin D deficiency.13 This correlation may be explained by decreased serum vitamin D levels increasing the expression of tumor necrosis factor-alpha (TNF-α), indicating that increased proinflammatory cytokine TNF-α may exacerbate asthma symptoms.14
A different study with 280 adult asthmatics found that people with bronchial asthma had reduced 25(OH)D concentrations. They came to the conclusion that there may be a hormonal influence on asthmatic inflammatory activity or vice versa given the substantial link between the severity of asthma and 25(OH)D concentrations. When respiratory infections occur, airway epithelia, which have large concentrations of the enzyme that changes circulating 25-OH-vitamin D3 into the active form of 1,25-OH-vitamin D3, may respond locally, thereby reducing inflammation.15
In addition, a study found a correlation among serum 25(OH)D levels as well as the likelihood of an asthma-related ER visit or hospital stay, indicating that vitamin D deficiency could be the most reliable predictor of asthma, surpassing even serum IgE levels and family history of asthma.3
Also, we discovered that people with bronchial asthma had higher blood IgE levels. Our findings align with Sandeep et al. (2010), who reported a correlation between total IgE levels and asthma, independent of allergen sensitization.16
According to these findings, bronchial asthma is linked to low vitamin D levels in both industrialized and developing nations. There is a correlation between the seriousness of bronchial asthma and the shortage of vitamin D. Vitamin d may help improve glucocorticoid responsiveness in severe asthmatics by upregulating CD4+ T cell production of the anti - inflammatory cytokine interleukin-10, regardless of total IgE levels, atopy type or corticosteroid use. Therefore, in bronchial asthma patients who are resistant to steroids, vitamin D may help regulatory T cells secrete interleukin-10 in response to these drugs.
Limitation
It is important to note that our study has certain limitations. Due to the small sample size and the use of topical corticosteroids and antihistamines by some patients, serum vitamin D levels may have been impacted.
CONCLUSION
This study indicates that individuals with bronchial asthma are more likely to have lower serum vitamin D levels and higher IgE levels, suggesting a potential role for vitamin D supplementation in asthma management. Treating vitamin D deficiency could be a beneficial strategy in improving asthma outcomes. Larger longitudinal studies are needed to validate these findings and further explore the mechanisms involved.
Authors’ contributions
PNK: Study design, data collection, manuscript writing; AA: Statistical analysis, literature review, manuscript editing; DKR: Patient recruitment, manuscript review.
Ethical approval
Institutional Review Board approval was exempted, as it is a observational, non interventional study utilizing de-identified, routinely collected clinical data with minimal risk to participants.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
REFERENCES
- The global burden of asthma: Executive summary of the GINA dissemination committee report. Allergy. 2004;59:469-78.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between serum total IgE and disease severity in patients with allergic asthma in Spain. J Investig Allergol Clin Immunol. 2015;25:120-7.
- [PubMed] [Google Scholar]
- Prevalence and risk factors for wheezing in children from rural areas of north India. Allergy Asthma Proc. 2007;28:647-53.
- [CrossRef] [PubMed] [Google Scholar]
- Is vitamin D deficiency to blame for the asthma epidemic? J Allergy Clin Immunol. 2007;120:1031-5.
- [CrossRef] [PubMed] [Google Scholar]
- Growth patterns of Qatari school children and adolescents aged 6-18 years. J Health Popul Nutr. 2005;23:250-8.
- [PubMed] [Google Scholar]
- Vitamin D insufficiency linked to asthma severity. Am J Respir Crit Care Med. 2009;179:739-742.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373-8.
- [CrossRef] [PubMed] [Google Scholar]
- Respiratory epithelial cells convert inactive vitamin D to its active form: Potential effects on host defense. J Immunol. 2008;181:7090-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of vitamin D in asthma. Ann Allergy Asthma Immunol. 2010;105:191-9. quiz 200-2, 217
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of vitamin D deficiency among inner-city African American youth with asthma in Washington, DC. J Pediatr. 2010;156:948-952.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vitamin D deficiency is associated with decreased lung function in Chinese adults with asthma. Respiration. 2011;81:469-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Serum 25 hydroxy vitamin D levels in adult asthmatic patients. Egypt J Hosp Med. 2012;49:946-952.
- [CrossRef] [Google Scholar]
- Vitamin effects on the immune system: Vitamins A and D take centre stage. Nat Rev Immunol. 2008;8:685-98.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Respiratory epithelial cells convert inactive vitamin D to its active form: Potential effects on host defense. J Immunol. 2008;181:7090-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evaluation of serum immunoglobulin E levels in bronchial asthma. Lung India. 2010;27:138-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





