Translate this page into:
A five-year review of in-hospital neonatal mortality: Trends and implications for care
* Corresponding author: Dr. Priyanka Gupta, Department of Pediatrics, ESIC Medical College and Hospital, Faridabad, Haryana, India. drpriyankaguptakapil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta P, Garg D. A five-year review of in-hospital neonatal mortality: Trends and implications for care. Ann Natl Acad Med Sci (India). 2025;61:122-6. doi: 10.25259/ANAMS_2_2024
Abstract
Objectives
The objectives of this study were to estimate the in-hospital mortality/survival outcomes at discharge and to determine the risk factors for in-hospital neonatal mortality.
Material and Methods
This study was a secondary data analysis (review) of the existing hospital records during the first five years of operationalization of the neonatal intensive care unit (NICU) in a tertiary care hospital at Haryana, India.
Results
There were 126 in-hospital mortality rates among a total of 2725 admissions (i.e., in-hospital neonatal mortality of 4.62 per 100). The in-hospital mortality among male and female neonates were comparable (4.52 vs 4.26%; P value 0.788). However, the in-hospital mortality among extramural births (5.52%) was significantly higher than the mortality among intramural births (4.26%; P = 0.010). Neonates with the lowest birth weight had the highest in-hospital mortality (P value < 0.00001). There was an exponential increase in the risk of in-hospital mortality among neonates with birth weight < 1500 g and < 1000 g, that is, 11.6% and 48.6%, respectively.
Conclusion
Information about in-hospital neonatal mortality and survival outcomes from NICU is an important indicator of quality of care. The in-hospital mortality in this study was comparable to other Indian studies, with poorer survival outcomes among neonates < 1500 g birth weight. Extramural births had higher mortality than intramural births, reminding us of the importance of in-utero fetus transfer among high-risk and preterm labor.
Keywords
Birth weight
Extramural
Gender
Intramural
Neonatal mortality
Survival outcome
INTRODUCTION
Although there has been an overall improvement in the survival of very low birth weight (VLBW) and extremely low birth weight (ELBW) neonates in recent years, it varies significantly between countries and regions, depending on the facilities and quality of medical care. Low- and middle-income countries are disproportionately affected due to their lack of healthcare technology and shortage of trained health personnel. The mortality rates among overall admissions to the neonatal intensive care units (NICUs) have been noted to vary from 3% to 29%, figures varying from 20% to 46% among ELBW, and from 5% to 12% among VLBW neonates.1 A recent systematic review and meta-analysis by Ramaswamy et al.2 (2021) included 192 studies, enrolling 22,278 ELBW neonates. In this review, the survival of ELBW babies in low-income, lower-middle-income, and upper-middle-income countries was found to be 18% (11–28%), 28% (21–35%), and 39% (36–42%), respectively.
Information about individual in-hospital neonatal mortality and survival outcomes is an indicator of quality of care, which helps clinicians to counsel the families appropriately and also guides administrators in allocating limited NICU resources. In this study, we estimated the in-hospital mortality/neonatal survival rates (till discharge) in a recent operational NICU of a tertiary care hospital at Haryana, India; secondary objectives were to determine risk factors for in-hospital neonatal mortality with the limited records.
MATERIAL AND METHODS
This study was a secondary analysis of the existing hospital records (review) at the NICU of a tertiary care hospital in Haryana, India. The data from June 5, 2018, till June 4, 2023, that is, the initial five years of its inception and operationalization, were reviewed. This facility provides services to both intramural and extramural births covered under a social security scheme. An approval from the Institutional Ethics Committee was granted. This being a review of existing records, a waiver of consent from parents was provided by the Ethics Committee.
The data included all neonates admitted to the NICU irrespective of any other factor(s), as also both intramural and extramural NICU admissions > 23 weeks and > 400 g in birth weight. The in-hospital mortality rate was calculated as the number of deceased neonates divided by the total number of neonatal admissions multiplied by 100. Neonates with birth weight 1000–1499 g were defined as VLBW and < 1000 g as ELBW.
The anonymized data was analyzed with SPSS version 25.0. Frequencies and percentages were used to summarize categorical variables. Pearson Chi-square test was applied to study the association of in-hospital mortality with gender, mural status (intramural or extramural), and the birth weight category. P value < 0.05 was considered significant.
RESULTS
In total, 2725 neonates were admitted to the NICU during the five years of the study period. This included both intramural and extramural births. The calendar year-wise admissions and in-hospital mortality data are described in Table 1 and Table 2, respectively. There was a steady increase in the number of admissions per year, and the absolute number of in-hospital deaths also increased proportionately [Figure 1]. Overall, there were 126 in-hospital mortality rates among a total of 2725 admissions (i.e., in-hospital neonatal mortality rate of 4.62/100); this also seemed to increase every year which could be explained by many variables like the rising proportion of lower birth weight and extramural admissions [Tables 1–3].
| Calendar year/number of neonatal admissions | Total admissions (N = 2725) |
Male N (%) |
Female N (%) |
Intramural births N (%) |
Extramural births N (%) |
Birth weight < 1000 g N (%) |
Birth weight ≥ 1000–1500 g N (%) |
Birth weight ≥ 1500–2000 g N (%) |
Birth weight ≥ 2000–2500 g N (%) |
Birth weight ≥ 2500 g N (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 2018 (June 5 to December) | 236 | 112 (47.46) | 124 (52.54) | 208 (88.14) | 28 (11.86) | 4 (1.69) | 26 (11.02) | 43 (18.22) | 63 (26.69) | 100 (42.37) |
| 2019 (January to December) | 186 | 104 (55.91) | 82 (44.09) | 137 (73.66) | 49 (26.34) | 5 (2.69) | 27 (14.52) | 33 (17.74) | 40 (21.51) | 81 (43.55) |
| 2020 (January to December) | 288 | 145 (50.35) | 143 (49.65) | 172 (59.72) | 116 (40.28) | 5 (1.74) | 18 (6.25) | 45 (15.63) | 105 (30.46) | 115 (39.93) |
| 2021 (January to December) | 574 | 295 (51.39) | 279 (48.61) | 411 (71.60) | 163 (28.40) | 8 (1.39) | 51 (8.89) | 107 (18.64) | 164 (28.57) | 244 (42.51) |
| 2022 (January to December) | 971 | 493 (50.77) | 478 (49.23) | 709 (73.02) | 262 (26.98) | 36 (3.71) | 79 (8.14) | 176 (18.13) | 265 (27.29) | 415 (42.74) |
| 2023 (January to June 4) | 470 | 267 (56.81) | 203 (43.19) | 309 (65.74) | 161 (34.26) | 16 (3.40) | 57 (12.13) | 75 (15.96) | 108 (22.98) | 214 (45.53) |
| Total admissions (N = 2725) | 2725 | 1416 (51.96) | 1309 (48.04) | 1946 (71.41) | 779 (28.59) | 74 (2.71) | 258 (9.47) | 479 (17.58) | 745 (27.34) | 1169 (42.90) |
| Calendar year/number of in-hospital neonatal deaths | Total deaths (N = 126) |
Male N (%) |
Female N (%) | Intramural births N (%) | Extramural births N (%) |
Birth weight < 1000 g N (%) |
Birth weight ≥ 1000–1500 g N (%) |
Birth weight ≥ 1500–2000 g N (%) |
Birth weight ≥ 2000–2500 g N (%) |
Birth weight ≥ 2500 g N (%) |
|---|---|---|---|---|---|---|---|---|---|---|
|
2018 (June 5 to December) |
1 | 1 (100.00) | 0 (0.00) | 1 (100.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (100.00) |
| 2019 (January to December) | 13 | 6 (46.15) | 7 (53.85) | 9 (69.23) | 4 (30.77) | 2 (15.38) | 7 (53.85) | 3 (23.08) | 0 (0.00) | 1 (7.69) |
| 2020 (January to December) | 7 | 4 (57.14) | 3 (42.86) | 5 (71.43) | 2 (28.57) | 1 (14.28) | 1 (14.28) | 1 (14.28) | 2 (28.57) | 2 (28.57) |
| 2021 (January to December) | 19 | 9 (47.37) | 10 (52.63) | 14 (73.68) | 5 (26.32) | 3 (15.79) | 6 (31.58) | 5 (26.32) | 3 (15.79) | 2 (10.53) |
| 2022 (January to December) | 54 | 26 (48.15) | 28 (51.85) | 32 (59.26) | 22 (40.74) | 20 (37.04) | 9 (16.67) | 5 (9.26) | 11 (20.37) | 9 (16.67) |
| 2023 (January to June 4) | 32 | 18 (56.25) | 14 (43.75) | 22 (68.75) | 10 (31.25) | 10 (31.25) | 7 (21.87) | 3 (9.37) | 5 (15.62) | 7 (21.87) |
| Total deaths (N = 126) | 126 |
64 (50.79) |
62 (49.21) |
83 (65.87) |
43 (34.13) |
36 (28.57) |
30 (23.81) |
17 (13.49) |
21 (16.67) |
22 (17.46) |
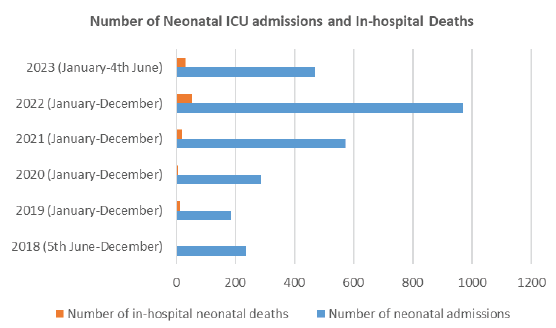
- Number of admissions and in-hospital neonatal deaths.
| Calendar year/ In-hospital mortality (per 100) | In-hospital mortality (per 100) | Males | Females | Intramural births | Extramural births | Birth weight < 1000 g | Birth weight ≥ 1000–1500 g | Birth weight ≥ 1500–2000 g | Birth weight ≥ 2000–2500 g |
Birth weight ≥ 2500 g |
|---|---|---|---|---|---|---|---|---|---|---|
| 2018 (June 5 to December) | 0.42 | 0.89 | 0.00 | 0.48 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 2019 (January to December) | 6.99 | 7.70 | 8.54 | 6.57 | 8.16 | 40.00 | 25.92 | 9.10 | 0.00 | 1.23 |
| 2020 (January to December) | 2.43 | 2.76 | 2.10 | 2.91 | 1.72 | 20.00 | 5.55 | 2.22 | 1.90 | 1.73 |
| 2021 (January to December) | 3.31 | 3.05 | 3.58 | 3.41 | 3.07 | 37.50 | 11.76 | 4.67 | 1.83 | 0.82 |
| 2022 (January to December) | 5.56 | 5.27 | 5.86 | 4.51 | 8.40 | 55.55 | 11.40 | 2.84 | 4.15 | 2.17 |
| 2023 (January to June 4) | 6.81 | 6.74 | 6.90 | 7.12 | 6.21 | 62.50 | 12.28 | 4.00 | 4.63 | 3.27 |
| Overall, in-hospital mortality | 4.62 | 4.52* | 4.74* | 4.26# | 5.52# | 48.65^ | 11.63^ | 3.55^ | 2.82^ | 1.88^ |
*P value 0.788: Chi-square test, #P value 0.010: Chi-square test, ^P value < 0.00001: Chi-square test
Table 3 describes the in-hospital mortality rate separately for each gender, intramural and extramural births, and birth weight category. The in-hospital mortality rates among male and female neonates were comparable (4.52% vs 4.26%; P value 0.788; Chi-square test). However, the in-hospital mortality among extramural births (5.52%) was significantly higher than among intramural births (4.26%; P = 0.010). The risk of in-hospital mortality (per 100) among neonates with birth weight < 1000 g was 48.6 in contrast to this risk of 1.88 among neonates with birth weight ≥ 2500 g. Neonates with the lowest birth weight had the highest in-hospital mortality (P value < 0.00001) [Table 3]. Figure 2 depicts an exponential rise of in-hospital mortality among neonates with birth weight < 1500 g and < 1000 g [Figure 2].
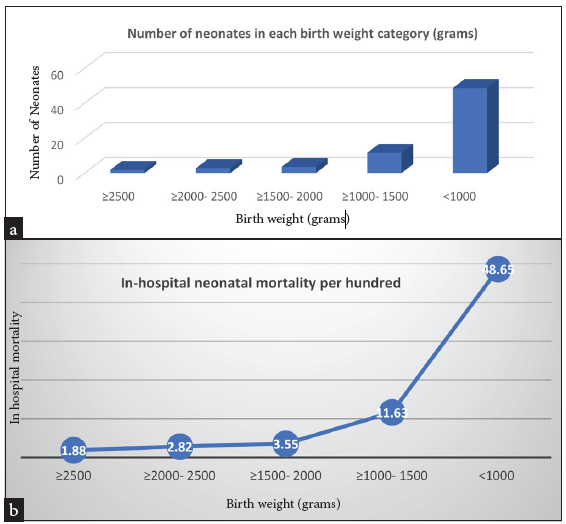
- (a) Birth weight characteristics and (b) risk of in-hospital mortality per 100.
DISCUSSION
The overall in-hospital mortality rate has been reported to vary widely from 3.1% to 3.8% in South Africa during 2007–2008,3 4% in Canada during 1996–1997,4 5.7% in Portugal during 2004–2008,5 6.5% in Qatar during 2002–2006,6 8.1% in England during 2008–2010,7 9.2% in Australia during 1995–2006,8 14.2% in Nigeria during 2012–2013,9 and 26–29% in Uganda in 2012.10
The association between LBW and poor survival outcomes is well established. Among VLBW neonates, the overall in-hospital mortality rate was reported to be 5% in New Zealand during 2009,11 6.5% in Korea during 2009,12 and 12.9% in the United States during 2007–2008.13 Neonatal mortality rates among ELBW were 34% in the United States during 2006–2009,14 46% in Australia during 2005–2010 ,15 30% in New Zealand during 2009,11 44.8% in Korea during 2009,12 and 45.9% in India during 2006–2008.16 This is also due to the variable study definitions of ELBW neonates. For instance, Alleman et al.14 (2013) defined ELBW as 401–1,000 g and Keir et al.15 (2014) defined ELBW as ≤ 500 g in their study.
National Neonatal-Perinatal Database report 2002–2003 recorded 55% mortality among ELBW neonates.17 In a prospective study at the level III neonatal unit of a teaching hospital in Northern India during 2009–2011, only 78 out of 149 ELBW admissions (52%) were discharged alive.18 Among other birth cohorts from India, VLBW mortality has been reported to vary from 14.8% to 40.9%.19–21 A multicentric study by Murki et al.20 (2015) evaluated the mortality of VLBW neonates (weighing 1500 g or less at birth) in 11 different neonatal units in India. Four centers admitted only intramural neonates and seven centers admitted both intra and extramural neonates. The study enrolled 1345 neonates, from which 199 (14.8%) died before discharge from the hospital.
Tripathy et al.22 (2019), from Odissa, India, enrolled all 212 neonates < 1500 g born in a single hospital during 2011–2013. Mortality of ELBW babies was 61.11% and that of VLBW babies was 26.41%. The death rate in babies with a weight range of 500–749 g, 750–999 g, 1000–1249 g, and 1250–1499 g was 87.50%, 53.57%, 30.76%, and 20.97%, respectively. Another recent descriptive study at a level III NICU of a tertiary care teaching hospital in South India during January to December 2017 included 239 VLBW neonates. The mortality among VLBW and ELBW was 20.5% and 69.3%, respectively.23
CONCLUSION
Although this study had some limitations due to the use of historical data in which only limited variables could be studied for association with mortality, it still provides valuable local reference information. The in-hospital mortality rate and survival outcomes at discharge were comparable to other Indian studies. Neonates born elsewhere and transported to the study site for management had higher mortality than intramural births. This reminds us of the importance of timely in-utero fetus transfer among high-risk births. To keep improving neonatal care and outcomes, such audits should be done regularly to monitor progress and address any new challenges.
Authors’ contributions
PG: developed the concept, design and disposition for the study; PG and DG: both were involved in collection of data and review of literature; PG prepared the initial draft of manuscript. The manuscript has been approved by both authors.
Ethical approval
The research/study approved by the Institutional Review Board at ESIC Medical College and Hospital, Faridabad, Haryana, number 134X/11/13/2023- IEC/DHR/118, dated 01st November 2023.
Declaration of patient consent
The study involved secondary analysis of anonytmized pre-existing hospital records and did not directly involve interaction with patients or their families. The requirement for obtaining informed consent was waived by the Institutional Review Board..
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- A selected review of the mortality rates of neonatal intensive care units. Front Public Health. 2015;3:225.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ELBW and ELGAN outcomes in developing nations: Systematic review and meta-analysis. PLoS One. 2021;16:e0255352.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Predicting mortality and length-of-stay for neonatal admissions to private hospital neonatal intensive care units: A Southern African retrospective study. Afr Health Sci. 2012;12:166-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Variations in mortality rates among Canadian neonatal intensive care units. CMAJ. 2002;166:173-8.
- [PubMed] [PubMed Central] [Google Scholar]
- Diagnosis and cause of death in a neonatal intensive care unit—how important is autopsy? J Matern Fetal Neonatal Med. 2011;24:760-3.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of 28+1 to 32+0 weeks gestation babies in the state of Qatar: Finding facility-based cost effective options for improving the survival of preterm neonates in low income countries. Int J Environ Res Public Health. 2010;7:2526-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Population-based estimates of in-unit survival for very preterm infants. Pediatrics. 2013;131:e425-32.
- [CrossRef] [PubMed] [Google Scholar]
- Causes of death in infants admitted to Australian neonatal intensive care units between 1995 and 2006. Acta Paediatr. 2013;102:e17-23.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of morbidity and mortality of newborns admitted into the sick and special care baby unit of Enugu State University Teaching Hospital, Enugu state. Niger J Clin Pract. 2014;17:346-51.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and risk factors for early neonatal mortality in newborns with severe perinatal morbidity in Uganda. Int J Gynaecol Obstet. 2014;127:201-5.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement in mortality of very low birthweight infants and the changing pattern of neonatal mortality: The 50-year experience of one perinatal centre. J Paediatr Child Health. 2012;48:596-9.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of neonatal care resources on regional variation in neonatal mortality among very low birthweight infants in Korea. Paediatr Perinat Epidemiol. 2013;27:216-25.
- [CrossRef] [PubMed] [Google Scholar]
- Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307:1709-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Individual and center-level factors affecting mortality among extremely low birth weight infants. Pediatrics. 2013;132:e175-84.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Beyond the borderline: Outcomes for inborn infants born at ≤500 grams. J Paediatr Child Health. 2014;50:146-52.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality and morbidity in extremely low birth weight (ELBW) infants in a neonatal intensive care unit. Indian J Pediatr. 2013;80:16-20.
- [CrossRef] [PubMed] [Google Scholar]
- National Neonatal-Perinatal Database Report 2002–2003. Indian Council of Medical Research. New Delhi. Available at: https://www.newbornwhocc.org/pdf/HRRC-Report_2002-03.pdf [Last accessed 2023 Sept 30].
- Predictors of mortality and major morbidities in extremely low birth weight neonates. Indian Pediatr. 2013;50:1119-23.
- [CrossRef] [PubMed] [Google Scholar]
- Early predictors of mortality in very low birth weight neonates. Indian Pediatr. 2001;38:596-602.
- [PubMed] [Google Scholar]
- Variability in survival of very low birth weight neonates in hospitals of India. Indian J Pediatr. 2015;82:565-7.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing the age at discharge of very low birth weight preterm neonates from a neonatal intensive care unit in Eastern India: A cohort study. Cureus. 2020;12:e11889.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mortality and morbidity of very low birth weight and extremely low birth weight babies in neonatal period. Int J Contemp Pediatr. 2019;6:645-9.
- [CrossRef] [Google Scholar]
- Short term outcome and predictors of mortality among very low birth weight infants – A descriptive study. Indian J Pediatr. 2021;88:351-7.
- [CrossRef] [PubMed] [Google Scholar]





