Translate this page into:
An insight into the heatstroke in Northern India: Clinico-pathological observation and outcomes from a tertiary care center
* Corresponding author: Ashish Gautam, Department of Medicine, S.N. Medical College, Agra, India. dr_ashishgautam@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Pursnani N, Yadav SK, Doneria JK, Agrawal P, Gautam A. An insight into the heatstroke in Northern India: Clinico-pathological observation and outcomes from a tertiary care center. Ann Natl Acad Med Sci (India). 2024;60:178-84. doi: 10.25259/ANAMS-2023-9-11-(1037)
Abstract
Objectives
To observe the clinical presentation, pathological changes, and outcomes of heatstroke at a tertiary care center.
Material and Methods
Patients presented with an axillary temperature above 104°F to the casualty during summers in the months of April and May 2022 were screened. After excluding the other causes of fever and based on history, patients were diagnosed as suffering from heatstroke. After taking valid consent, treatment was initiated, and all observations were taken. Clinical presentation, demographic data, vitals, and investigations (hemogram, renal function, liver function, CPK, IL6, CRP, and random glucose levels) were recorded, diagnosed, and enrolled for observation. Chi-Square test for 2 x 2 contingency table used to identify the association between CPK and muscle cramps. The T-test for 2 Independent Means and the Pearson Correlation Coefficient test were used for analyzing other data.
Results
For the study, 112 patients were enrolled and classified as per severity: 80 were pre heatstroke, 22 were mild heatstroke, and 10 were severe heatstroke. Age above 50 years is associated with severe forms of disease and poor outcomes. Out of 112, 28 (25%) participants were 50 years or above age. Nine (32.1%) out of these 28 developed pre-heatstroke, and 19 (67.8%) developed mild to severe heatstroke. Creatinine kinase was raised in 17 out of 112 (15.1%) participants, but the proportion of participants having raised CPK does not differ by the presence of myalgia. IL6 was also found to be elevated and related directly to the severity of the disease in this study.
Conclusion
Heatstroke is a common disease that occurs due to working on farms during the summer. Old age is more prone to severe disease and poor outcomes. Raised IL6 also correlates directly with disease severity.
Keywords
Heat cramps
Heat exhaustion
Heat injury
Heat stress
Heatstroke
Summer sickness
INTRODUCTION
Heatstroke is a condition of abnormal thermoregulation characterized by a fatal rise in core body temperature of more than 40°C or 104°F in addition to central nervous system abnormalities like altered consciousness, seizures, and sometimes coma along with,heatstroke can also cause multi-organ failure and death. It is a common disease that usually occurs in states with tropical climate conditions. Bundelkhand region of central India is geographically located at a place where most landscapes consist of irregular uplands with outcrops of rocks intermingling with lowlands rocky hills, and the climate is semi-arid during summers. Every year since 2010, more than 1000 deaths have been reported from various parts of India, with a maximum of 2040 deaths in 2015 and 1111 in 2016. Most of these are from Uttar Pradesh, Bihar, Maharashtra, Orissa, and Andhra Pradesh. From 2006 to 2010, more than 3332 deaths were attributed to heat-related illness.1 Death records due to heatstroke from South Asian countries in April 2023 were 179 (India), 22 (Pakistan), 2 (Malaysia), and 2 (Thailand).
Several other infectious diseases prevalent in tropical areas of India often share common symptoms like high-grade fever, altered sensorium, and seizures. The presence of acute renal failure, rhabdomyolysis, cardiac arrhythmias, and seizures determines the high mortality rate and fatal outcomes. Effective cooling of the body and reducing core body temperature to normal without landing to hypothermia is the gold standard for the management of heatstroke. Management of hyperpyrexia or hyperthermia in the initial 24 hours of presentation to the hospital is often rewarding in cases of heatstroke. That’s why an early diagnosis and management are very important to prevent mortality and morbidities. Management of comorbidities like shock, acute renal failure, rhabdomyolysis, seizures, and multi-organ dysfunction (MODS) is done on the usual lines of treatment.
The rapid increase in the environmental temperature in the months of April and May has increased the number of cases of casualty in our Institute. In this study, we hereby present the clinical, biochemical, and treatment outcomes of the cases presented.
Significance
Bundelkhand is one of the hottest regions in India and is primarily composed of farmlands. This study contributes clinical and pathological data among field workers. Thus, results from this study help further derive better treatment guidelines for the management of heatstroke among this group of patients.
MATERIAL AND METHODS
Study design and settings
The study was conducted in the Department of Medicine at Rani Durgawati Government Medical College, district Banda, Uttar Pradesh, India and S N Medical College, district Agra, Uttar Pradesh, India. The study was conducted during the months of April and May 2022. Participants enrolled were those presented to the casualty department seeking treatment. Participants presented to casualty with fever having an axillary temperature of ≥104°F, signs of dehydration, hypotension or low pulse pressure, muscle cramps and tenderness, altered behavior, and classical clinical background were screened for inclusion. The diagnosis was made after the exclusion of all other infectious causes of presenting clinical features by sepsis screening.
Data collection and classification
Enrolled participants were interviewed for onset, duration and progression of symptoms, duration and type of exposure to heat, any aggravating factor for present symptoms, and treatment taken before presentation to casualty. Every possible symptom pertaining to heat-related illness described in the literature search was enlisted in the data record sheet. Vitals, including BP, pulse, respiration and temperature, and random blood glucose, were recorded. Systemic examination with special details of the neurological system was done and recorded. Based on presenting symptoms and vitals, participants were graded for severity and grouped into (1) pre heatstroke, (2) mild heatstroke, and (3) severe heatstroke. Severe heatstroke is further graded to heat cramps, heat exhaustion, and classical heatstroke.
Ethical approval
Ethical clearance of this observational study was received from Ethical committee of S N Medical College, Agra (Letter No: SNMC/ IEC/2021/52, Dated: 05-Apr-2022). Written informed consent was obtained from all enrolled subjects.
Methodology
Participants diagnosed with heatstroke were investigated, including complete blood picture, renal, liver, thyroid functions tests, arterial blood gas analysis, random blood glucose, creatinine phosphokinase, C reactive protein, and complete urinalysis. Treatment to reduce core temperature included ice sponging, chilled saline infusions, and oral rehydration solutions. Treatment guidelines for complications were adopted from updated standard evidence-based recommendations. Death due to heatstroke is defined as any mortality during treatment in hospitalization duration or one week after the discharge due to any complication arising out of the primary condition, including deep vein thrombosis (DVT), acute renal failure (ARF), liver failure, brain death, any cardiac problem, etc.
Statistical analysis
The website https://www.socscistatistics.com was used to do all statistical calculations. Various statistical tools like the Chi-Square test for a 2 x 2 Contingency Table, T-test for 2 Independent Means, and Pearson Correlation Coefficient test were used for analyzing the data. The one-way, or one-factor Analysis of Variance (ANOVA) test for independent measures is used to compare the means of all investigations in three groups.
RESULTS
Demography
A total of 267 patients admitted with axillary temperature ≥104°F were screened for heatstroke. After exclusion and removing who lost follow up, a total of 112 patients were enrolled for the study. Two participants with severe grades expired due to multi-organ failure. The remaining r 110 participants completed the study with no long-term morbidity.
Age is an important factor in disease severity. Figure 1 illustrates the age distribution in different severity groups. Older age is often associated with poor outcomes of acute diseases. Eighty-four (75%) participants were less than 50 years of age, out of which 71 (84.5%) developed preheatstroke, whereas 13 (15.5%) had mild to severe heatstroke. On the other hand, 28 (25%) participants were 50 years or above age, out of which nine (32.1%) developed preheatstroke and 19 (67.8%) developed mild to severe heatstroke. A chi-square test of independence showed that there was a significant association between age above 50 years and disease severity, X2 (1, N = 112) = 28.2, p = 0.00001.
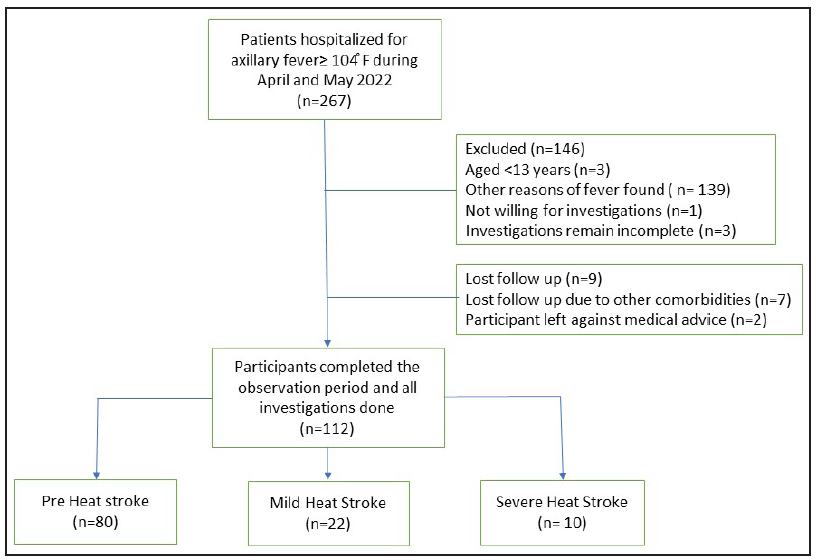
- Flow chart of the case selection process.
Clinical presentation
Oliguria due to dehydration was the first symptom complained by 30.5% of participants. Three participants were also presented with anuria. Myalgia, which occurs due to intermittent contraction of muscles due to electrolyte imbalance, was the second most prominent symptom present in 25% of participants. Creatinine kinase (CK) is raised (normal value 10 to 120 mcg/L) in 17 out of 112 (15.1%) participants. The proportion of participants having raised CK did not differ by the presence of myalgia, X2 (1, N = 112) = 1.8, p > 0.17. The result is not significant at p < 0.05. Myalgia and CK are not associated with heatstroke.
Pathological findings
All demographic, clinical, and pathological characteristics and outcomes are summarized in Table 1. A significant difference is found in three groups at the parameters of hematocrit, serum creatinine, and Blood urea Nitrogen (BUN). Figure 2 illustrates all the pathological findings among different severity groups and their frequencies.
| Sl. No. | Characteristics | n | SD |
|---|---|---|---|
| 1 | Age | 38.7 years | 14.2 |
| 2 | Sex | ||
| Male | 72 | ||
| Female | 40 | ||
| 3 | Duration of symptoms onset | 23.2 hours | 14.1 |
| 4 | Received first aid | ||
| Yes | 91 | ||
| No | 21 | ||
| 5 | Disease severity | ||
| Pre heatstroke | 80 | ||
| Mild heatstroke | 22 | ||
| Severe heatstroke | 10 | ||
| • Subtype heat cramps | 2 | ||
| • Subtype heat exhaustion | 4 | ||
| • Subtype classical heatstroke | 4 | ||
| 6 | Axillary temperature °F (Avg.) | 103 | 1.5 |
| 7 | Pulse rate per min | 139 | 15.9 |
| 8 | Systolic BP mmHg | 118 | 25.8 |
| 9 | Diastolic BP mmHg | 73.3 | 15.7 |
| 10 | Respiratory rate per min | 24 | 11.3 |
| 11 | Clinical features n (%) | ||
| Myalgia | 28 (25.0) | ||
| Diarrhea | 13 (11.6) | ||
| Oliguria | 34 (30.5) | ||
| Respiratory distress | 9 (8.0) | ||
| Confusion | 20 (17.8) | ||
| Delirium | 3 (2.6) | ||
| Hallucination | 1 (0.8) | ||
| Decerebrate | 1 (0.8) | ||
| Seizures | 1 (0.8) | ||
| Coma | 1(0.8) | ||
| 12 | Pathological findings | ||
| Hemoglobin g/dL (12–18 g%) | 11.3 | 2.1 | |
| Hematocrit % (36%–50%) | 48.9 | 3.1 | |
| Platelets count in lakh (1.5-4.5 lakh/µL) | 1.3 | 0.4 | |
| CRP mg/L (<0.3 mg/dL) | 6.5 | 2.1 | |
| IL6 pg/mL (<7 pg/mL) | 24 | 8.6 | |
| Creatinine mg/dL (0.7–1.3 mg/dL) | 0.8 | 0.5 | |
| BUN mg/dL (7–20 mg/dL) | 24.7 | 20.4 | |
| SGPT IL/L (19–33 IU/L) | 37.9 | 22.6 | |
| CPK mcg/L (10–120 mcg/L) | 86.1 | 32.7 | |
| RBG mg/dL (<140 mg/dl) | 102.2 | 51.8 | |
| 13 | Outcome | ||
| Survived | 110 | ||
| Expired | 2 | ||
CRP: C reactive protein, IL6: Interleukin 6, BUN: Blood urea nitrogen, SGPT: Serum glutamic pyruvic transaminase, CPK: Creatine phosphokinase, RBG: Random blood glucose, SD: Standard deviation.
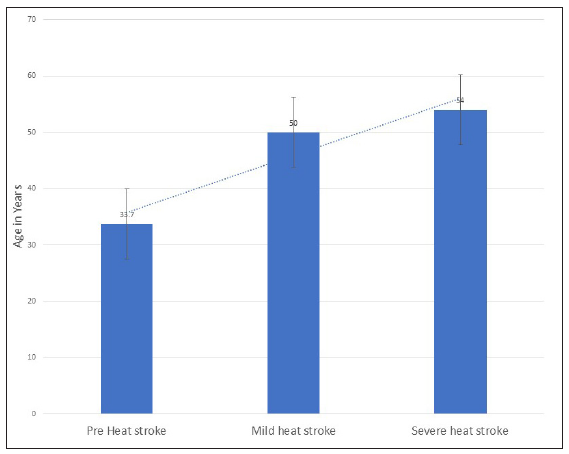
- Age distribution and disease severity.
DISCUSSION
Heatstroke remains one of the leading causes of morbidity and mortality in summers in tropical regions in India. This study contributes several important inputs for various clinical and pathological characteristics of heatstrokes. Patients’ age always remains the most important factor for disease occurrence and disease outcomes.2 In our study, out of 112 participants, 28 (25%) were ≥50 years of age. 61 ± 13.5 years was the mean age of 27 study participants in a study by Ninan et al.3 Old age is associated with less adaptive mechanisms towards heatstroke. Classical heatstroke occurs in young and old age people due to extreme heat waves during summers without preceding exertion, whereas exertional heatstroke occurs due to athletic activity or strenuous exertion during variably warm or hot weather or while wearing heat-retaining clothing.4 Poor sudomotor, cardiovascular, and immune function, along with defective behavioral thermoregulation, are the important factors why geriatric age is at high risk for heatstroke.5
Measuring rectal temperature is the best way to access the exact core body temperature during heatstroke. We lacked this in our study as we measured the axillary temperature. Axillary temperature was 103 ± 1.5°F in this study. In a study by Deshwal et al. among paratroopers suffering from exertional heat exhaustion in the Agra district of India, the average rectal temperature was 104.74°F.6 This is equivalent to our study considering the difference between rectal and axillary temperature, where the former remains 0.5 to 1.0°F higher than the latter.7 Oliguria, followed by myalgia, was the most frequent manifestation in our study. Dehydration and oliguria are present in 29% of sufferers of heatstroke.8 Inability to maintain hydration due to lack of water and unawareness towards heat while engaged in farm work were the common reasons due to which our study participants land up into heat-related illnesses, especially dehydration and oliguria.
Myalgia was the prominent manifestation of heatstroke presented in 28 (25%) participants. Hyponatremia and dehydration, hypokalemia, increased lactic acid levels, and exertional muscle injuries are the prominent causes of myalgia and fatigue among patients.9 Judicious selection of fluids, correction of electrolytes, and cold sponging are effective methods to reduce myalgia.10 The presence of confusion, mental obtundation, and restlessness are prominent features of mild and severe heatstroke.6 Hyponatremia, hypercalcemia, cortical vein thrombosis, lactic acidosis, and metabolic alkalosis are defined as etiological factors behind CNS manifestations of heatstroke. Further, sepsis and MODS could lead to metabolic encephalopathy and seizure.11 Symptomatic management, effective cooling, and rehydration during golden hours in critical care units are always rewarding, with minimal residual CNS deformities.12 Delirium, hallucinations, and decerebrate rigidity are also rarely reported CNS manifestations of heatstroke.13–15 Renal dysfunction like pre-renal ARF secondary to dehydration or intrinsic renal failure due to prolonged dehydration, myoglobinuria, or sepsis syndrome is also recognized complications of heatstroke.16,17 The average S creatinine levels in our study in the severe heatstroke group was 1.8 mg% whereas it was 0.8 mg% in pre heatstroke group. In 13 out of 112 (11.6%), S creatinine and 34 out of 112 (30.3%), BUN were more than 13 mg% and 24 mg%, respectively. The raised values of S creatinine and BUN responded to rehydration in all participants. All participants who received institutional first aid elsewhere before visiting our institute had normal renal functions clearly explains its importance. Values of other relevant investigation like Hematocrit, Platelet count, C Reactive protein, Interleukin 6, Blood urea Nitrogen, serum glutamic pyruvic transaminase (SGPT), Creatine phosphokinase and Random Blood Glucose in different severity groups are illustrated in Figure 3. Management and outcomes of participants requiring dialysis for ARF due to heatstroke are not different than the cases with other causes.18 Severe acute liver injury has also been reported due to heatstroke.19 Recognition of common pathological changes and their clinical correlation helps in management. In a study by Gharibi et al., hematocrit is raised in 87.1% of participants admitted for heatstroke.20 In another study by Deshwal et al., no changes in hematocrit levels were observed during heatstroke.6 In our study, the significant difference in hematocrit between pre heatstroke group and the combined mild and severe group was found (t-value is –6.97367; p-value is <0.00001. The result is significant at p < 0.05). This suggests that raised hematocrit could be a predictor of poor prognosis and outcomes in heatstroke. Elevated CRP levels (152±40 mg/L) were reported by Bouchama et al. in 72% out of 28 hajj pilgrims who suffered heatstroke.21 IL6 was also found to be elevated and related directly to the severity of the disease in this study. In another study by Kuo-Cheng Lu et al., among participants with exertional heatstroke, proinflammatory cytokines IL-1beta, tumor necrosis factor-alpha, IL-6; T helper 1 cytokines INF-gamma and IL-2 receptor; and chemokines IL-8, monocyte chemoattractant protein 1, and Regulated upon Activation, normal T cell Expressed and Secreted (RANTES) were found to be elevated.22 CRP and IL6 levels were also elevated in this study and correlated directly with the disease severity.
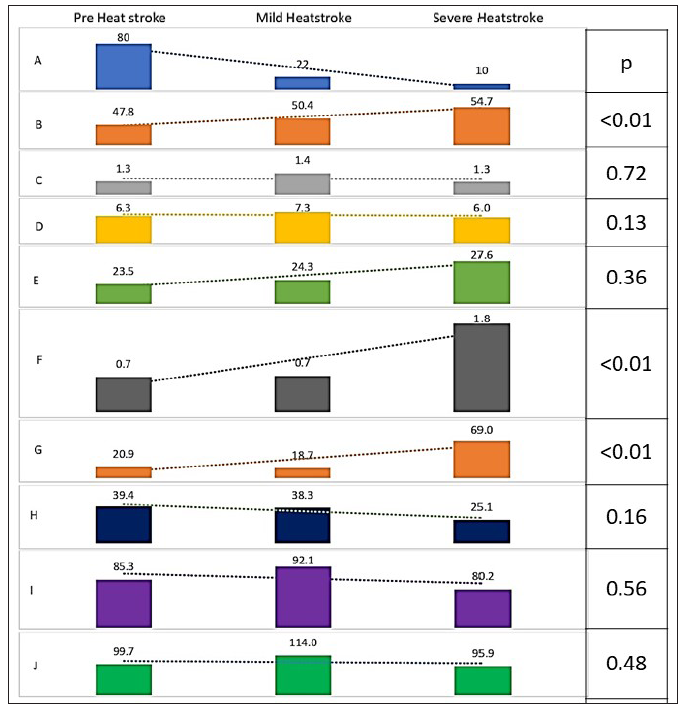
- Changes in pathological findings in different stages of heatstroke. (A) subject count; (B) Hematocrit; (C) Platelet count in lakh; (D) CRP; (E) IL6; (F) S. Creatinine; (G) BUN; (H) SGPT; (I) CPK; (J) RBG. Trendline denotes changes as per severity. CRP: C reactive Protein, IL6: Interleukin 6, BUN: Blood Urea Nitrogen, SGPT: Serum Glutamic Pyruvic transaminase, CPK: Creatine Phosphokinase, RBG: Random Blood Glucose.
The biggest strength of this study is that it is the first- study done in the Bundelkhand region of India, which experiences extremes of temperature during summers and winters. The study incorporated participants suffering due to their working conditions, thus may help to add data for developing basic and advanced treatment lines for them. After searching all databases, we found that this study contributes all relevant information from the maximum number of participants ever reported from Indian studies. There are certain limitations of this study that need to be considered. First, measuring axillary temperature is not a standard method as done in this study. However, measuring oral or rectal temperature in an agitated and altered patient was not feasible. Second, a few subjects were referred to our institute after getting basic treatment. Thus, the exact clinical presentation and investigation may differ from the actual. Finally, as most of the participants were laborers working in farms and fields, thus, exactly defining the type of stroke as classical or exertional among participants was not possible.
CONCLUSION
Exposure to hot environmental temperatures can cause heatstroke with variable presentations. The outcome of heatstroke could be benign or fatal. Results from this study suggest an early and basic treatment can improve the prognosis and outcome of heatstroke. Raised hematocrit, S creatinine, and BUN suggest poor prognosis and should be managed intensively. Besides other pathological investigations, inflammatory markers like IL6 and CRP could determine prognosis in case of heatstroke. Further detailed investigatory studies are needed in critical heatstroke subjects to substantiate the observations found so far.
Ethical approval
The research/study approved by the Ethical committee at S N Medical College, Agra, number SNMC/ IEC/2021/52, dated 05th April 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Heat-related illness – Clinical profile and predictors of outcome from a healthcare center in South India. J Family Med Prim Care. 2020;9:4210-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thermoregulatory disorders and illness related to heat and cold stress. Autonomic Neurosci. 2016;196:91-104.
- [CrossRef] [PubMed] [Google Scholar]
- Impairments to thermoregulation in the elderly during heat exposure events. Gerontol Geriatr Med. 2020;6:2333721420932432.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and biochemical characteristics of exertional heat stroke among paratroopers in Agra, India. J Assoc Physicians India. 2017;65:57-61.
- [PubMed] [Google Scholar]
- Normal oral, rectal, tympanic and axillary body temperature in adult men and women: A systematic literature review. Scand J Caring Sci. 2002;16:122-8.
- [CrossRef] [PubMed] [Google Scholar]
- Heatstroke: Be ready for summer. Patient Care. 1993;27:52. Available from: https://link.gale.com/apps/doc/A13869115/AONE?u =anon∼2e7b8242& sid=googleScholar&xid=3cfc1b99
- [Google Scholar]
- Evaluation and treatment of heat-related illnesses. Am Fam Physician. 2002;65:2307-14.
- [PubMed] [Google Scholar]
- Exertional heat stroke: Pathophysiology and risk factors. BMJ Medicine. 2022;1:e000239.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exertional heat stroke - Golden hour is the key to success: A report from Peripheral Military Hospital of Northern India. J Assoc Physicians India. 2019;67:100.
- [PubMed] [Google Scholar]
- It’s getting hot in here: A rare case of heat stroke in a young male. Cureus. 2018;10:e3724.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thermal injury of the nervous system. In: Dobbs MR, ed. Clinical neurotoxicology. Philadelphia: W.B. Saunders; 2009. p. :569-76.
- [Google Scholar]
- P. L. A. P. C. of C. C. M. Expert group of heat stroke prevention and treatment of the people’s liberation army. Expert consensus on the diagnosis and treatment of heat stroke in China. Mil Med Res. 2020;7:1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute kidney injury due to rhabdomyolysis and renal replacement therapy: A critical review. Crit Care. 2014;18:224.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Characteristics of heat illness during hajj: A cross-sectional study. Biomed Res Int. 2018;2018:5629474.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35:349-55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Severe acute liver injury related to heat stroke. Eur J Case Rep Intern Med. 2020;7:001382.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effect of heat stress on hematological parameters and oxidative stress among bakery workers. Toxicol Ind Health. 2020;36:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Elevated pyrogenic cytokines in heatstroke. Chest. 1993;104:1498-502.
- [CrossRef] [PubMed] [Google Scholar]
- Role of circulating cytokines and chemokines in exertional heatstroke. Crit Care Med. 2004;32:399-403.
- [CrossRef] [PubMed] [Google Scholar]





