Translate this page into:
Atypical progress of tuberculosis in the peripartum period: Report of a paradoxical reaction
*Corresponding author: Jyotsna Sharma, Obstetrics and Gynecology, Jawaharlal Institute of Post Graduate Medical Education and Research, Puducherry, India. jyotsnaa.sharma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma J, Dorairajan G. Atypical progress of tuberculosis in the peripartum period: Report of a paradoxical reaction. Ann Natl Acad Med Sci (India). 2024;60:228-30. doi: 10.25259/ANAMS-2023-5-3-(921)
Abstract
Central nervous system involvement is noted in approximately 1% of all Tuberculosis (TB) cases. Worsening of pre-existing tubercular lesions following antitubercular treatment in the absence of disease relapse or any other diagnosis is called a paradoxical reaction. We detail an atypical evolution of TB in a pregnant woman. We report the case of a woman admitted with respiratory symptoms at 35 weeks of Pregnancy. She had a spontaneous onset of labor within 48 hours and delivered a 1.6 kg live baby. Investigations confirmed pulmonary TB. She was started on antituberculosis treatment. Post-partum, she developed persistent headaches, and the imaging confirmed tuberculoma in the left inferior frontal gyrus with leptomeningeal enhancement. She was started on steroids. She was readmitted after two weeks due to a new onset holocranial headache, and MRI detected a new large tuberculoma in the temporal region hence, a diagnosis of Pleuropulmonary with Extrapulmonary tuberculosis with a Paradoxical reaction was made. Anti-edema measures were added, and the patient was managed in hospital for another 2 weeks. The case details and the possibility of flare due to puerperium and steroids are discussed. In pregnant women with active TB disease, complications of perinatal death, preterm birth, acute fetal distress, and low birth weight are increased. The risks of untreated active disease in a pregnant woman are higher than the risks of its treatment. A high index of suspicion, avoiding overcrowding, proper nutrition, timely and appropriate initiation of treatment may have a favorable pregnancy outcome.
Keywords
Paradoxical reaction
Pregnancy and puerperium
Tuberculosis
INTRODUCTION
Worsening of preexisting lesions following antitubercular treatment (ATT) in the absence of disease relapse or any other diagnosis is called a paradoxical reaction.1,2 Increased incidence of paradoxical reaction has been reported in patients with autoimmune disease on immunomodulators like monoclonal antibodies, lymph node tuberculosis, and human immunodeficiency virus (HIV) co-infected population.1,3–5 It is more likely to flare up in the postpartum period once the immunological changes of Pregnancy start reverting to normal. It is important to be aware of this entity while treating patients with Tuberculosis as it can be confusing with possible wrong diagnosis or treatment failure due to drug resistance. We discuss a case with atypical progress of TB from lungs to brain and postpartum brain spread despite appropriate treatment.
CASE REPORT
A 20-year-old G2P0L0A1 (Second gravida with no living children and history of previous abortion) was referred to us at 35 weeks of gestation from a nearby district with complaints of occasional cough with minimal expectoration for 6 months, shortness of breath, intermittent low-grade fever, and loss of appetite for 1 week duration. She had a positive history of contact with TB with her father, who was on ATT. General physical examination showed a poor nutrition status, tachycardia, low-grade fever, and pallor. There was no generalized lymphadenopathy; she was mildly dyspneic with a respiratory rate of 28 per minute, and the oxygen saturation was 93% in room air. Auscultation revealed normal cardiac sounds, decreased breath sounds, and bronchial breathing on the right lower lung field. Obstetric examination suggested a clinically growth-restricted fetus, further confirmed by ultrasonogram, and the admission cardiotocograph (CTG) was normal. She was immediately admitted to the intensive care unit (ICU), propped up and positioned with oxygen on flow, and management was planned with a multidisciplinary team of obstetricians, anesthetists, respiratory physicians, general physicians, and neonatologists. Her hemoglobin was 8.2g%, total leukocyte count (TLC) was 2430/µL, and platelets were 3.06 lakh/µL. Renal and liver function tests were within normal limits. Chest X-ray showed a right lower zone opacity with pleural effusion [Figure 1]. She was kept under vigilant vital monitoring and started on round-the-clock antipyretics, hydration, and optimum calories. Sputum was sent for culture sensitivity, gram stain, Acid Fast Bacillus (AFB) stain, and Gene Xpert. COVID-19 testing was negative. Post-admission, she spontaneously went into preterm labor and delivered a 1.6 kg female baby uneventfully. The baby was shifted to the neonatal ICU for observation. Subsequently, her Gene Xpert was reported positive for Mycobacterium tuberculosis (MTB) with sensitivity to Rifampicin and was started on Category I ATT comprising fixed-dose combination of isoniazid, rifampicin, pyrazinamide, and ethambutol, three tablets a day based on her weight band. On postnatal day 4, she complained of severe unremitting generalized headache, and prolonged period of lethargy and drowsiness. There was no history or record of febrile spikes, convulsions, urinary tract infection, breast engorgement, leg pain, chest pain, breathlessness, or foul-smelling lochia. A general physical examination revealed tachycardia and pallor. Neurological examination showed a confused patient with a slow response but otherwise normal higher mental functions. Muscle bulk, tone, power, and sensory system were normal, and plantar reflex was extensor. There was no evidence of any facial nerve palsy and no positive signs suggestive of meningitis, papilledema, or tubercles on fundus examination. The liver function tests were normal. Magnetic resonance imaging (MRI) of the brain was done, which showed a sub-centimetric well-defined ring enhancing T2 hypointense lesion with subtle perilesional edema in the left inferior frontal gyrus suggestive of tuberculoma along with leptomeningeal enhancement [Figure 2]. The diagnosis was expanded to extrapulmonary Tuberculosis with tubercular meningitis and tuberculoma. Analgesics and oral dexamethasone 6 mg at a frequency of twice a day for 2 weeks followed by weekly tapering doses over 5 weeks, were added to the preexisting treatment. Her headache and drowsiness improved after the addition of steroids and analgesics. She tolerated drugs well, liver function tests were normal, and she was discharged home 20 days later, with directly observed treatment short-course (DOTS) registration and Isoniazid prophylaxis for the neonate. After 2 weeks of discharge, she reported back to the hospital with a recurrence of severe holo cranial, yet predominantly left-sided headache and vomiting. She was taking 4 mg oral Dexamethasone twice a day when she developed the recurrence of headache. There were no seizure episodes, fever, neck pain, limb weakness, or visual disturbance. A repeat chest X-ray showed a reduction in pleural effusion than the previous one. Fundus examination showed signs of early papilledema, and repeat MRI showed new, large tuberculoma and exaggerated leptomeningeal enhancement in the left temporal region [Figure 3] hence, a diagnosis of pleuropulmonary with extrapulmonary tuberculosis with a paradoxical reaction was made. She was under observation and along with ATT, oral steroids were replaced with an injection of Dexamethasone 4 mg intravenous eighth hourly, and oral Acetazolamide 125 mg twice a day was added as the anti-edema measure. Her headache improved and she was discharged home after ensuring compliance. In the follow-up visits, she was declared cured at the completion of treatment.
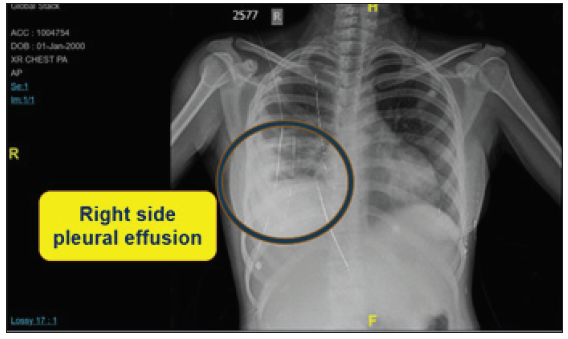
- Chest X-Ray showing right lower zone opacity with pleural effusion.
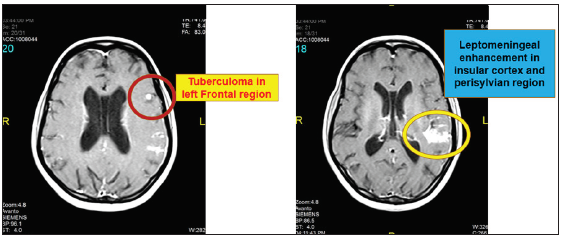
- Post-contrast magnetic resonance imaging (MRI) brain showing tuberculoma in left inferior frontal gyrus with leptomeningeal enhancement.
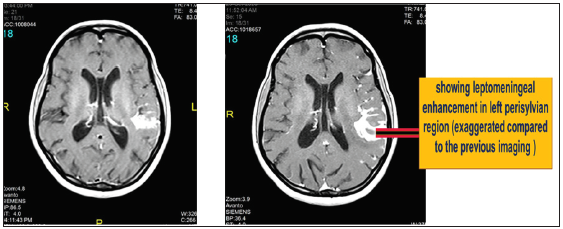
- Follow-up MRI showed new tuberculoma and exaggerated leptomeningeal enhancement in the left temporal region.
DISCUSSION
The principles for the treatment of Tuberculosis in a pregnant woman with presumed drug-sensitive disease are the same as in the nonpregnant state. In pregnancies in women with active TB disease, there is an increased risk of perinatal death, preterm birth, acute fetal distress, and low birth weight.6 A state of vague ill health may be present for 2 to 8 weeks prior to the development of meningeal irritation,7,8 which may often be confused with the nonspecific complaints in Pregnancy. Moreover, the weight gain during Pregnancy can mask the weight loss accompanying tuberculosis, thereby giving a false sense of reassurance.6 A review9 of 29 cases published in 2003 documented that tuberculosis developed a median of 10 days after delivery, with 76% of the patients experiencing symptoms within 10 days postpartum. About 93% of the patients with tuberculosis during the postpartum period had extrapulmonary involvement, and of these patients, 69% had central nervous system (CNS) infection. Nevertheless, the progress of the disease to newer lesions, even after the commencement of ATT is rare. A recent case report10 from Central America described a young postpartum woman who succumbed to the reactivation of undiagnosed prepartum latent Tuberculosis. Pregnancy is a relatively immunocompromised state due to the maternal immune tolerance to prevent fetal rejection; however, the immune reconstitution in the postpartum period can lead to the flare-up of the disease.
In our case, there was fetal growth restriction and she had pulmonary symptoms. She had a spontaneous preterm delivery. The postpartum flare-up involved the nervous system. Maybe she already had disseminated tuberculosis at the time of presentation. The neurological symptoms manifested once the lung symptoms subsided. It is also possible that addition of steroids for the neurological disease would have further spread the TB to form yet another tuberculoma. Such a flare has not been reported. Poor nutrition, poor socioeconomic status, postpartum immune-modulation, and heavy tubercle bacilli load could have resulted in this atypical flare.
CONCLUSION
The risks of untreated active tuberculosis in Pregnancy outweigh the risks of the treatment of the disease. A high index for suspicion of flare-ups despite treatment, timely and appropriate initiation of and compliance with treatment may have a favorable pregnancy outcome and complete recovery in women with TB in the peripartum period.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Paradoxical reaction in tuberculous meningitis: presentation, predictors and impact on prognosis. BMC Infect Dis. 2016;16:306.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Determinants of treatment-related paradoxical reactions during anti-tuberculosis therapy: A case control study. BMC Infect Dis. 2016;16:479.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Paradoxical Response to Antituberculous Therapy in Infliximab-Treated Patients with Disseminated Tuberculosis. Clin Infect Dis. 2005;40:756-9.
- [CrossRef] [PubMed] [Google Scholar]
- Immune reconstitution inflammatory syndrome in non-HIV immunocompromised patients. Curr Opin Infect Dis. 2009;22:394-402.
- [CrossRef] [PubMed] [Google Scholar]
- Paradoxical reaction in the form of new pulmonary mass during anti-tuberculosis treatment: A case series and literature review. Infect Drug Resist. 2019;12:3677-85.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A rare case of CNS tuberculosis with Pregnancy. Int J Reprod Contracept Obstet Gynecol. 2015;4:911-4.
- [Google Scholar]
- Central nervous system tuberculosis. Afr Health Sci. 2011;11:116-27.
- [PubMed] [PubMed Central] [Google Scholar]
- M. Loto, Ibraheem Awowole. Tuberculosis in Pregnancy. J Pregnancy. 2012;2012:379271.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Peripartum Tuberculosis as a form of immune restitution disease. Eur J Clin Microbiol Infect Dis. 2003;22:313-7.
- [CrossRef] [PubMed] [Google Scholar]
- An Unfortunate Case of Reactivation of Tuberculosis in a Postpartum Female. Cureus. 2020;12:e11775.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





