Translate this page into:
Favorable Pregnancy Outcome in a Patient with Uncorrected Uni-ventricular Heart - A Case Report and Review of Literature
Correspondence : Dr. Charu Sharma, Assistant Professor, Department of Obstetrics & Gynecology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. Mob. : 7063956215. Email: sharma.charu651@gmail.com.
Abstract
Univentricular heart or a heart with a double inlet ventricle is a rare congenital cardiac anomaly that poses a great challenge for the clinicians owing to increased maternal and fetal complications. It may even lead to maternal mortality. We here describe a case that was managed efficiently and successfully in a low resource setting.
Keywords
Univentricular heart
pulmonary stenosis
aortic stenosis
low resource setting.
Introduction
Of the seven per 1000 live infants born with congenital heart disease, over 85% now survive into adult life (1). Single ventricle represents a rare abnormality found in 3.2% of patients with congenital heart disease (CHD), often discovered during childhood (2). Pregnancy with this rare complex congenital heart disease poses a great challenge to the obstetrician. We, here report a case of successful outcome in a pregnancy with double inlet ventricle and pulmonary stenosis and discuss the literature review.
Case Report
A 23 years old primi-gravida at 32 weeks gestation with complex congenital heart disease was admitted in our maternity ward with threatened preterm labor. Her past medical history revealed that she was diagnosed to have a double inlet ventricle with severe aortic and pulmonary stenosis, one and a half years back when she was being evaluated for dyspnoea and palpitation with her pre-existing diagnosis of rheumatic heart disease (RHD) with severe aortic stenosis at some other centre. Considering the complexity of surgical procedure (Fontan operation) with subaortic outflow resection and uncertainty of long term outcome with surgery, the patient had refused for surgical correction and opted for medical follow-up.
Her first visit to our antenatal clinic was at 8 weeks of gestation for a routine check-up. She had no complaints except for dyspnoea (NYHA class II). Physical examination revealed clubbing of fingers (Figure 1) and cyanosed lips, nose and tongue. Her oxygen saturation (SpO2) was 84% and heart rate was 64 beats/minute. On auscultation S1 was normal S2 single; ejection systolic murmur of grade 3/6 was heard at left 2nd intercostal space. Her baseline echocardiography showed a double inlet single ventricle with intermediate morphology, malposed great vessels both arising from the rightward aspect of single ventricle, large ventricular septal defect (VSD), severe subvalvular aortic stenosis and severe valvular pulmonary stenosis with peak gradient of 10 mmHg. The systolic performance of a single ventricle was conserved (ejection fraction= 60%). Rest all investigations were within normal limits. A fresh Echocardiography was repeated that showed the similar findings and there was no deterioration in ejection fraction or development of pulmonary hypertension. The family was counseled about the complexity of the condition and associated poor prognosis, but they decided to continue the pregnancy. Ultrasonography confirmed a single live intrauterine pregnancy of 8.3 weeks. Following this, she had regular antenatal visits along with cardiological assessment. Despite the severity of her disease, she had an uneventful antenatal period. Anomaly scan at 20 weeks showed no gross anomaly in fetus. Fetal echo at 28 weeks was normal but there was evidence of asymmetric intra uterine growth restriction (IUGR) with normal Doppler.

- Arrow showing the distorted angle of nail bed.
On admission at 32 weeks for threatened preterm labor she was managed conservatively & steroids were given for pulmonary maturity. Her hemoglobin was 11.3 gm% and haematocrit of 41%. An electrocardiogram showed a sinus bradycardia with sinus rhythm, ST changes in lead V1, V2, V3; left axis deviation with intraventricular conduction defects (Fig. 2). Repeat sonography revealed high resistance flow in umbilical arteries and moderate oligohydramnios. She was taken up for an elective caesarean section at 33.4 weeks period of gestation under antibiotic coverage & epidural anaesthesia & delivered an alive male baby of weight 1.7kg & APGAR 8/10 at 1 min. Intra operative period was uneventful. The estimated blood loss was 600ml. Pain relief was achieved with epidural top ups followed by paracetamol infusion. She had atonic PPH one hour after the caesarean which was managed conservatively and one unit packed cell volume was transfused. In the post operative period, her oxygen saturation remained between 74% - 80% in room air. She was given intermittent humidified oxygen to maintain her saturation. Anti-coagulation with low molecular weight heparin was started eight hours after surgery for prophylaxis against deep vein thrombosis and replaced by oral anticoagulants from the fourth day.
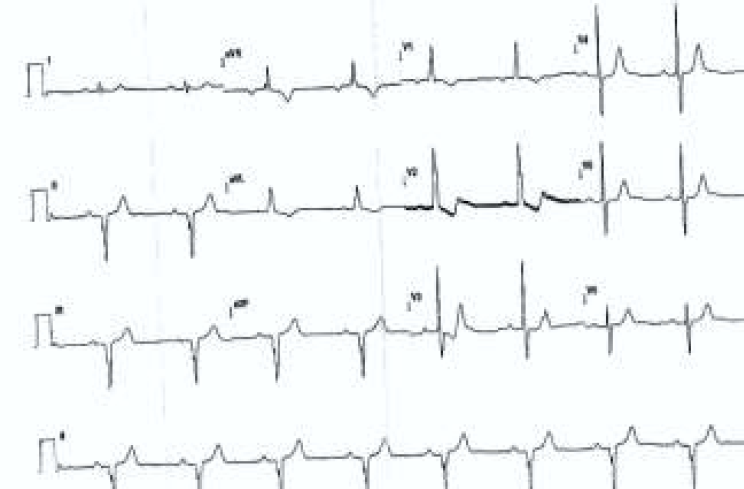
- Electrocardiogram.
Echocardiography of the newborn was normal. She was discharged on 10th post operative day in satisfactory condition. She has been under regular follow-up for last one year and is in good condition.
Discussion
Cardiac diseases in pregnant women are now increasingly encountered in our clinical practice. With recent advances in the field of pediatric cardiac surgery and improved childhood survival, there is a rising trend in the population of reproductive age women with congenital heart diseases. Most of these women, especially those with lesions of moderate or severe complexity, have sequelae that increase their risk of cardiovascular complications during pregnancy (3).
Univentricular heart or double inlet ventricle is a rare congenital cardiac anomaly, characterized by a large dominant ventricle, most commonly, a morphologic left ventricle while the other ventricle is a small rudimentary chamber. Patients with a functionally single morphological left ventricle with a well balanced circulation i.e. some degree of pulmonic stenosis to avoid excessive pulmonary blood flow, may achieve late survival with good ventricular function, exercise capacity and minimal symptoms (4). Our patient had severe pulmonary stenosis which was good for her as it prevented the development of pulmonary hypertension. Unoperated cases of univentricular hearts have poor prognosis with a median survival of 14 years (death rate of 4.8% per year) and with majority of patients presenting with cyanosis and decreased exercise tolerance (3). Pregnant women with cyanotic CHD are at increased risk for maternal and neonatal complications. Fortunately, as long as their ventricular function is normal they tolerate pregnancy well. Maternal heart failure, pregnancy induced hypertension, pulmonary oedema, endocarditis, arrhythmias, embolism, stroke, hemorrhage, thrombosis, and maternal death are the risks encountered in these pregnancies (5). In uncorrected pregnant patients with cyanotic CHD the usual pregnancy associated fall in systemic vascular resistance and rise in cardiac output exacerbate right to left shunting leading to increased maternal hypoxemia and cyanosis (6). Fetal complications such as premature births, small for gestational age, low birthweight and respiratory distress syndrome are often associated with univentricular heart disease (5). Our patient also presented with preterm labor and the baby had IUGR.
Since such patients are prone to maternal and fetal complications, they should ideally be managed in a tertiary care centre with a fully equipped cardiac care unit (CCU) and round the clock availability of a cardiologist, anaesthetist and obstetrician. Our hospital was the only tertiary care hospital in the Andaman & Nicobar group of Islands where people used to come from far off places & remote islands either by ships or by helicopters. The hospital had a good medical and surgical intensive care unit with almost all the facilities but unfortunately there was no CCU and cardiologist at that time. Patient was therefore advised referral to the mainland but she refused to go. However she could be well managed by the combined efforts of physician, anaesthetist and the obstetricians. The favorable outcome reported in our patient was probably due to the absence of pulmonary hypertension.
A study by Presbitero et al. examining the outcomes of 96 pregnancies in 44 women with a variety of cyanotic CHD reported a high rate of maternal cardiac events (32%), including one mortality, prematurity (37%), and a low live birth rate (43%) (7). The main determinants of live birth were the arterial oxygen concentration at rest (>85%). They concluded from the study that women with cyanotic CHD can go through pregnancy with a low risk to themselves, with frequent treatable complications, but there is a high incidence of miscarriage, premature births, and low birth weights (7).
Favorable outcomes have been reported following vaginal delivery or caesarean section in women with univentricular heart (8-10). Epidural anaesthesia provides excellent analgesia in the immediate post operative period. All patients must receive antibiotic cover and thromboprophylaxis during their hospital stay or until they achieve full mobilization (10). Moreover preconception counseling should be emphasized so as to allow women to make informed pregnancy decisions and risk stratification tool can be helpful to predict pregnancy risk.
Conclusion
Pregnancy is often well tolerated in a single ventricle patient with good NYHA functional class, good ventricular function and an oxygen saturation > 85%. The risk of paradoxical emboli in these patients is high and meticulous attention should be paid to avoid deep venous thrombosis in these patients.
Declarations
Authors declare no conflict of interest.
References
- Congenital heart disease in pregnancy-Review. Postgrad Med J. 2005;81:292-298. doi: 10.1136/pgmj.2004.026625
- [CrossRef] [PubMed] [Google Scholar]
- Heart disease in pregnancy. In:. In: de Swiet M, ed. Medical Disorders in Obstetric Practice (4th). Oxford: Blackwell; 2002. p. :1125. PMID: 17134063
- [CrossRef] [Google Scholar]
- The ROPAC registry: a multicentre collaboration on pregnancy outcomes in women with heart disease. European Heart Journal. 2013;34(9):634-635. doi: 10.1093/eurheartj/ehs335
- [CrossRef] [PubMed] [Google Scholar]
- CCS Consensus Conference 2001 update: Recommendations for the Management of Adults with Congenital Heart Disease SECTION XIV - Single Ventricles. http//www.achd-library.com
- [Google Scholar]
- Williams Obstetrics. In: Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, eds. Cardiovascular disease (23rd). United States of America: McGraw-Hill Companies; 2010. p. :958-82.
- [Google Scholar]
- Pregnancy in cyanotic congenital heart disease. Outcome of mother and fetus. Circulation. 1994;89:2673-6. [PubMed]
- [CrossRef] [PubMed] [Google Scholar]
- Successful Pregnancy in a Patient with Univentricular Heart and Pulmonary Stenosis Heart Views : The Official Journal of the Gulf Heart Association. . 2012;13(2):71.
- [CrossRef] [PubMed] [Google Scholar]
- Successful pregnancy and delivery in a woman with a single ventricle and Eisenmenger syndrome. J Saudi Heart Assoc. 2013;25(4):261-264. doi: 10.1016/j.jsha.2013.05.001 PMCID: PMC3818635
- [CrossRef] [PubMed] [Google Scholar]
- Successful pregnancy and caesarean section delivery in a patient with single ventricle and transposition of the great arteries. J Obstet Gynaecol. 2005;25:69-70. doi: 10.1080/01443610400025911
- [CrossRef] [PubMed] [Google Scholar]





