Translate this page into:
Labrune syndrome: A unique entity
* Corresponding author: Dr. Dushyant Kumar Varshney, MD, DNB, Department of Radiology, Rama Medical College, Kanpur, Uttar Pradesh, India. dushyantvarshney657@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varshney DK, Labrune syndrome: A unique entity. Ann Natl Acad Med Sci (India). doi: 10.25259/ANAMS_13_2024
Abstract
A 23-year-old female was presented with complaints of seizures and progressive neurological deficit. contrast-enhanced computed tomography scan of the brain was performed which revealed extensive intracranial calcifications, intracranial cysts, and diffuse white matter hypodensity. Based on the imaging findings, diagnosis of Labrune syndrome was made.
Keywords
Cerebral calcifications
Cysts
Leukoencephalopathy
INTRODUCTION
Labrune syndrome is extremely rare association of extensive cerebral calcifications, Leukoencephalopathy, and cysts which was first labelled as entity by Labrune et al.1 In this case report we describe a rare case of Labrune syndrome, its clinical features, classic radiological findings and approach to its differential diagnosis.
CASE REPORT
A 23-year-old female with a rural background and low socioeconomic status presented in our hospital with complaints of multiple seizures episodes since the past five years. She also had a history of gradually progressive weakness in the right upper and lower limb since the past ten months. Recent episode of seizure was three days back—generalized tonic-clonic seizure—lasting for a few minutes. The episode was associated with the involuntary passage of urine and stools. There was postictal confusion also. She was taking antiepileptic treatment for the past five years; she was on valproate therapy, but not taking treatment regularly. She was born full term with normal vaginal delivery and no history of birth asphyxia or hospitalization; also no history of similar disorder among antecedents. There was no history of recent trauma and no abnormality was found on general physical, ophthalmologic examinations. On neurological examination, the Glasgow Coma Scale E4V5M6 indicated that she was conscious and cooperative, and revealed mild to moderate cognitive decline and subnormal intelligence. Cranial nerve examination was unremarkable. On examination of the motor system, tone was increased and bulk was decreased with the power of 2/5 across all joints on the right side. Deep tendon reflexes were exaggerated. The sensitivity for touch and pain was decreased on the right side. She had bilateral cerebellar signs, including incoordination, finger-nose ataxia, dysdiadochokinesia, and gait ataxia, with tremors and slurring of speech. Various laboratory tests were done to rule out etiology. Complete blood count, erythrocyte sedimentation rate, liver and renal function test, thyroid and parathyroid profile, serum calcium, phosphate, lactate, and alkaline phosphatase levels were within normal limits. Serological evaluation for cytomegalovirus, toxoplasma gondii, hydatid cyst, and human immunodeficiency virus (HIV)-1 and 2 were negative. electroencephalogram showed an epileptic focus originating from the right frontal region. Contrast enhanced computed tomography scan of the brain was performed revealing an extensive coarse bilateral basal ganglia, cerebral, and dentate calcifications. Multiple non enhancing intracranial cysts and diffuse white matter hypodensities [Figure 1] and no significant mass effects were also noted. Based on the clinical scenario and imaging background, patient treatment plan was changed to Levetiracetam and advised biopsy as well as further genetic testing. Patient refused further genetic testing as well as procedure due to reluctance as well as financial constraints.
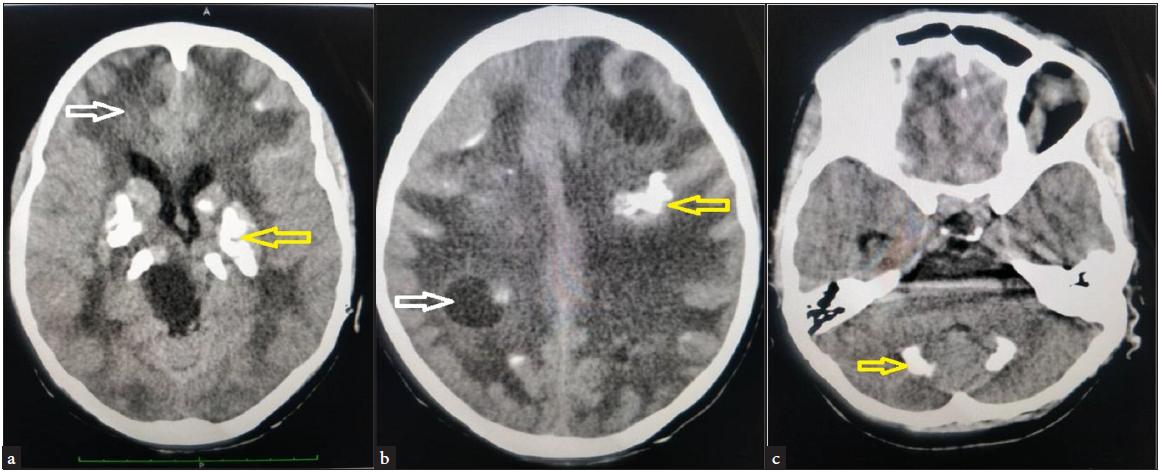
- (a) Demonstrating the diffuse white matter hypodensities (white arrow) and coarse bilateral basal ganglia calcifications (yellow arrow). (b) Demonstrating intracranial cyst (white arrow) and white matter calcifications (yellow arrow). (c) Demonstrating cerebellar calcifications (yellow arrow).
DISCUSSION
Labrune et al. (1996) were the first to describe the extremely rare association of extensive cerebral calcification and white matter changes/leukoencephalopathy with calcifications and cysts (LCC) as an entity.1 The main pathological feature of Labrune syndrome is cerebral microangiopathy, coexisting with microhemorrhages, gliosis, and intracranial calcifications. Various theories of cyst formations have been described previously in the literature. A few of them suggested that cyst formation is due to obliterative microangiopathy leading to necrosis. The type of calcification seen in Labrune syndrome is dystrophic.2 Jenkinson et al. (2016) identified the SNORD118 mutation is the leading cause of Labrune syndrome.3 Stable ribonucleic acid (RNA)-protein complexes, such as SNORD118, with uridine-rich RNA components, are called small nuclear ribonucleoproteins (snRNPs).These snRNPs may have a role in the pre-mRNA splicing.3 The onset of Labrune syndrome may occur from early infancy to adolescence, with signs including cognitive decline, convulsions, pyramidal, extrapyramidal, and/ or cerebellar signs. Visual field defects may also be seen sometimes. Clinically, various diseases present with seizures and progressive neurological deficit, but the classical radiological features of the triad points toward the diagnosis of LCC.4
The differential diagnosis of similar imaging features includes metabolic diseases and parasitic infections. Parasitic diseases include neurocysticercosis, cystic echinococcosis and cryptococcosis. Multiple cystic lesions with variable parenchymal calcification are seen in neurocysticercosis.5 Gelatinous pseudocyst and parenchymal calcification are reported in HIV patients with cryptococcosis.6 Serological tests can help in ruling out parasitic infestations. Also, leukoencephalopathy is not a characteristic feature of these parasitic diseases. Other metabolic diseases which show extensive basal ganglia and dentate calcification, like Fahr’s disease do not have other features such as leukoencephalopathy and cystic lesions. Coats disease may present with leukoencephalopathy, cysts, and calcification, named as Coats plus.7 It was ruled out, as our patient had normal ophthalmological findings.
CONCLUSION
Although, many diseases presents with imaging findings of intracranial calcifications, cysts & leukoencephalopathy this classical radiological triad of cerebral calcifications, cysts & leukoencephalopathy is usually diagnostic of this rare entity Labrune syndrome. Further, definitive diagnosis of Labrune syndrome can be achieved by genetic analysis of SNORD118. Treatment is primarily symptomatic, involving surgery to reduce mass effect and medical management to control seizures and mental status changes. Currently, there is no curative treatment available for the disease.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Extensive brain calcifications, leukodystrophy, and formation of parenchymal cysts: A new progressive disorder due to diffuse cerebral microangiopathy. Neurology. 1996;46:1297-301.
- [CrossRef] [PubMed] [Google Scholar]
- Leukoencephalopathy with intracranial calcifications and cysts in an adult: Case report and review of literature. Ann Indian Acad Neurol. 2010;13:299-301.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mutations in SNORD118 cause the cerebral microangiopathy leukoencephalopathy with calcifications and cysts. Nat Genet. 2016;48:1185-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leukoencephalopathy, cerebral calcifications, and cysts: New observations. Neurology. 2004;62:1206-9.
- [CrossRef] [PubMed] [Google Scholar]
- [Clinical and diagnostic approaches to neurocysticercosis] Med Pregl. 2001;54:353-6.
- [PubMed] [Google Scholar]
- Central nervous system cryptococcosis: Parenchymal calcification and large gelatinous pseudocysts. AJNR Am J Neuroradiol. 1997;18:107-9.
- [PubMed] [PubMed Central] [Google Scholar]
- Cerebroretinal microangiopathy with calcifications and cysts (CRMCC) Am J Med Genet A. 2008;146A:182-90.
- [CrossRef] [PubMed] [Google Scholar]





