Translate this page into:
Loss of lateral femoral condyle following sepsis of knee region in infancy: The hypothesis of vascular pathogenesis and clinical course
*Corresponding author: Anil Agarwal, Department of Pediatric Orthopedics, Chacha Nehru Bal Chikitsalaya, Delhi, India. rachna_anila@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Agarwal A, Jethwa R. Loss of lateral femoral condyle following sepsis of knee region in infancy: The hypothesis of vascular pathogenesis and clinical course. Ann Natl Acad Med Sci (India). 2024;60:231-5. doi: 10.25259/ANAMS-2022-8-10-(714)
Abstract
Complete loss of lateral femoral condyle of the femur following sepsis of the knee region in infancy is a well-recognized entity. The etiopathogenesis of the sequelae is poorly understood with synovial plicae and post-septic growth disturbance postulated as possible causes. Two illustrative cases are presented to elucidate the clinical effects of condylar loss in the pediatric age group.There is a typical pattern of unicondylar damage, loss of adjacent metaphysis, and metaphyseal spur in involved cases. Abnormal loading of the knee, ligament laxity, and the presence of a physeal bar contribute additionally to deformity. The deformity progression can be as rapid as 2.8 degrees per month. The lesion is most often treated by balancing the knee mechanics using osteotomies and growth modulations. The lesion progresses downhill due to the absence of lateral support of the knee joint configuration. The anatomical region supplied by the superior lateral genicular vessels closely matches with the lateral unicondylar femoral loss seen post-sepsis. A vascular etiology is therefore hypothesized for the lesion.
Keywords
Infection
Lateral femoral condyle
Loss
Sepsis
Introduction
Complete loss of one femoral condyle of the femur is recognized as one of the most devastating complications of osteoarticular infection of the knee region in infancy.1–7 Loss of lateral condyle of femur post sepsis is the more frequently recognized entity.2-4 What follows is a course of progressive angular deformity, joint instability, and limb length discrepancy. The described interventions for the pathology either require several repetitions or, at best are salvage procedures aimed at reducing disability.2,7
The anatomical description of this entity is strikingly similar in various series.2-4 Following infection in infancy, an area of destruction appears in the epiphysis and adjacent metaphysis in a few days.2 With the settling of soft tissue swelling, a well-circumscribed defect involving epiphysis and metaphysis manifests a few weeks later. The margins of the defect are well-defined almost resembling the loss of one-half of the distal end femur, including the epiphysis and adjacent metaphysis [Figure 1]. The proximal margins of the bony defect may spread out a bit in the form of a “metaphyseal” spur.2 This appearance persists for several years post-infection.
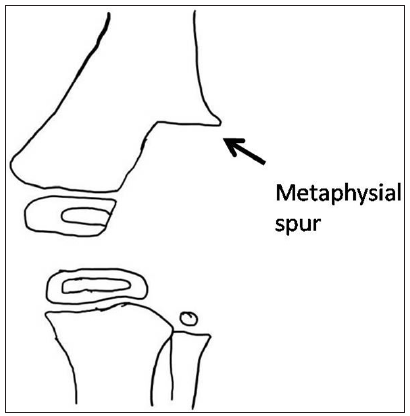
- The typical sequelae observed following infection of the knee region in infancy: There is a loss of one-half of the distal end femur including the epiphysis and adjacent metaphysis. The proximal margins of the bony defect may spread out a bit in the form of a “metaphyseal” spur.
The etiopathogenesis of the above sequelae remains ill-understood. It is variably described as a consequence of osteomyelitis or septic arthritis of the knee region.2-7 Strong et al. put forward the concept of metaphyseal infection spreading to the epiphysis through transphyseal blood vessels.8 However, the above theory could not explain the sparing of the medial femoral articular cartilage while the whole joint was infected. To explain the “unicondylar” involvement, Tercier et al. postulated the synovial septum hypothesis wherein the opposite condyle was shielded from the proteolytic effect of bacteria.7 The trans-synovial septae could however be demonstrated only in about 15% of knees. The “loculation” hypothesis again could not explain the unicondylar damage as once the infection spreads into epiphysis and metaphysis, there are no absolute barriers to the spread of infection.
Lately, there have been extensive studies on the vascular supply of the distal femur with osteochondral flaps and genicular artery embolization for knee osteoarthritis.9–12 The present manuscript aims to revisit the etiopathogenesis of post-infective lateral unicondylar femoral loss with a vascular origin hypothesis. Two representative cases are presented to illustrate the clinical course following such lesions.
CASE REPORTS
Case 1
A 1.5-year-old girl presented with complaints of progressive valgus deformity of the right knee [Figure 2]. Her previous records revealed management for septic arthritis of the right knee joint at 10 days of life. The joint was decompressed by arthrotomy under the cover of intravenous antibiotics. The cultures isolated Staphylococcus aureus. The infection settled by 6 weeks. Serial radiographs showed partial loss of lateral femoral epiphysis by 6 months of age. The typical pattern of unicondylar damage, loss of adjacent metaphysis, and metaphyseal spur were obvious by 12 months. Computed tomography and MRI imaging reaffirmed the plain radiological findings. At the time of presentation to our institution, the lateral distal femoral angle (LDFA) had worsened to 30 degrees. The approximate rate of deformity progression was 2.8 degrees per month since the septic event. She underwent a distal medial closing wedge femoral osteotomy supplemented with growth modulation to prevent an early recurrence. She has also been advised to a hinged long knee brace post-operatively. The tension band plate was removed when the limb was aligned to neutral at 18 months post-surgery. At follow-up of 31 months, the deformity had already partially recurred (LDFA 74 degrees). The child continues to use the brace and is in regular follow-up.

- Illustrative case 1: (a) Anteroposterior view of right knee joint at age 10 days when septic arthritis of the joint was diagnosed. (b). Partial loss of epiphysis visible by 6 months. (c) Typical unicondylar loss of distal femur and adjacent metaphysis on lateral side at 12 months. Metaphyseial spur could also be appreciated (white arrow). (d) Computed tomography (e) MRI images of the lesion. (f,g) Clinical deformity and knee range of movement at 1.5 years. (h) Combined procedure distal medial closing wedge femoral osteotomy and tension band plating of medial side. (i,j,k) Follow- up 31 months – clinical and radiological findings of recurrent deformity.
Case 2
A 2.5–year-old girl was seen with severe valgus deformity of the right knee region [Figure 3]. The parents reported the onset of deformity soon after the child initiated walking. This child had a history of severe neonatal sepsis (Organism: Streptococcus) at age 15 days of life with multifocal involvement of the left shoulder, left elbow, and right knee joint. The interventions involved multiple aspirations of the joints and intravenous antibiotics. The loss of the right lateral femoral condyle was obvious as early as 2 months in this child. At the time of presentation to our institution, the LDFA was 56.4 degrees. At age 3 years, the child underwent a distal medial closing wedge femoral osteotomy. Deformity at this time was 80 degrees. At 6 years, with the onset of recurrent deformity, an eccentric physeal bar was detected. The bar was excised and growth modulation of the medial femoral side was added. The limb length discrepancy at this time had progressed to 5 cm and therefore, concomitant left distal femoral complete epiphysiodesis was also performed. At the last follow-up, when the child had achieved skeletal maturity (at age 14 years), the right knee movements were relatively preserved, but there was a residual valgus of 12.4 degrees. The limb length discrepancy was 4 cm at this time. The patient is being planned for deformity correction and limb length equalization surgery.

- Illustrative case 2: (a,b) severe neonatal sepsis with multifocal joint involvement. Radiographs at 2 months. Lesions are obvious in the right knee and lateral metaphysis, left shoulder, and elbow region. (c,d) Child at 2.5 years of age. Clinical deformity and radiological appearance. (e,f) Medial closing wedge osteotomy of the distal femur was performed at age 3 years. Healed osteotomy and corrected limb alignment at this stage. (g,h,i) Child at 6 years. The deformity had recurred. Partial regeneration of the lateral condyle is obvious. There was evidence of an eccentric physeal bar in the distal femur which was excised and a medial side tension band plating was added. (j,k) Follow up at skeletal maturity at age 14 years. Residual valgus at knee and limb length discrepancy. Knee range of movements fairly preserved. (l,m) Scanogram of the limb and the fate of other affected joints at the same follow-up.
Discussion
The pathogenesis of loss of lateral femoral condyle following sepsis of the knee joint in children is debated. The primary site of infection – metaphysis or joint space; the presence of synovial plicae and loculation or post-septic growth disturbance all have been postulated.1–7 None could, however, fully explain the characteristic appearance of the lesion.
Singson et al. hypothesized a possible ischemic cause as the destructive changes typically seen due to proteolytic activity were not evident in the epiphysis and adjacent metaphysis.6 Additionally, the partial regrowth of the affected region demonstrated over time in a few cases supported the ischemic etiology. Newer insights into the vascular anatomy of the distal femur may provide an answer to the occurrence of typical destruction patterns noticed in the said pathology.9–12 The superior lateral genicular artery (SLGA) is the main vascular supply to the lateral femoral condyle9,13,14 [Figure 4]. As a consistent branch from the popliteal artery, it originates approximately 4 cm proximal to the knee joint line. It runs laterally on the posterior aspect of the femur to reach the lateral intermuscular septum. Posterior to the septum, it gives out a superficial branch and a deep branch. The superficial branch travels anteriorly, giving off skin perforators, and ends at the superolateral patella. The deep branch pierces the intermuscular septum to travel anteriorly on the lateral surface of the femur, giving branches to the vastus lateralis, the lateral head of the gastrocnemius muscle, the biceps femoris muscle, periosteum of the femur and ends by terminal end branches supplying the lateral femoral condyle. Overall the area supplied by SLGA extends approximately 12 cm above the lateral femur condyle in adult dissections. This very anatomy of SLGA forms the basis of vascularized lateral condylar graft used for reconstruction of non-union and defects of the hand, tibia, mandible, etc.
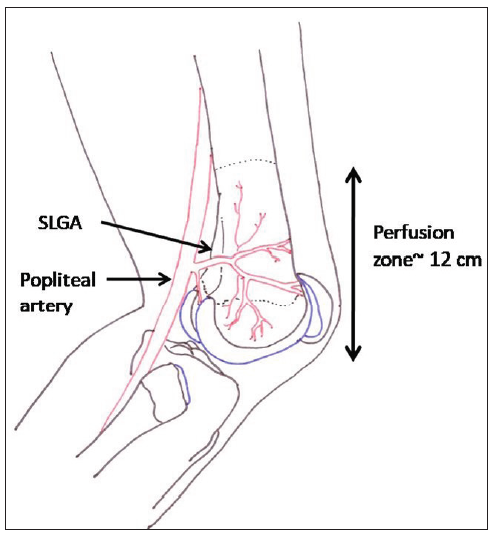
- The area supplied by superior lateral genicular artery (SLGA). It is branch of popliteal artery and arises on the posterior aspect of knee. Approximately 12 cm of lateral half of distal femur is completely supplied by this vessel.
The lateral condyle of the distal femur is shown to be far more vascular than its medial counterpart in experimental studies.15 This may predispose lodgement of infection in the lateral region. The SLGA vessel has a much larger bore of 1.5 mm compared to a medial vessel of size 1.2 mm. Thus, the lateral condyle grabs the larger share of the blood supply of the distal femur. Studies have shown that the application of a lateral locking plate over the distal femur resulted in a mean 21% total reduction in distal femoral arterial contribution.15 When an additional medial plate was applied, it reduced the blood supply of the distal femur further by only 4%.
The chief mechanisms through which osteoarticular infection damages tissues are ischemia (vasculitis/thrombus/pressure tamponade), lysis by bacterial and inflammatory toxins and in some cases by host immune response. The lateral distal femoral supply is dedicated yet precarious. The anatomical area supplied by SLGA closely matches the loss of articular cartilage and the metaphyseal region associated with sepsis of the knee region in children. It is, therefore justified to hypothesize that an ischemic phenomenon occludes the SLGA early in infection. The occlusion of the vessel prevents further invasion by bacterial and host responses and, therefore the resultant clear demarcation of the involved region. Partial regeneration as noticed in several series, is theoretically possible with the dissolution of the thrombus, regeneration of newer vessels, or formation of collaterals from the surrounding vasculature.
Clinically, post-infective damage of the femoral condyle is associated with loss of lateral support of the knee joint configuration. What follows is a downhill course with progressive angular deformity and joint instability, as shown in the illustrated cases. The deformity progression can be as rapid as 2.8 degrees per month (Case 1). Abnormal loading of the knee, ligament laxity, and the presence of a physeal bar contribute additionally to deformity. The lesion is most often treated by balancing the knee mechanics using osteotomies and growth modulations.2 The ongoing growth soon overcomes the correction achieved and in most patients, and throughout the disease, multiple osteotomies may be required. Langenskiöld documented that up to six osteotomies may be needed before skeletal maturity in these children.4 In illustrated case 1, an early removal of tension band plating resulted in partial recurrence of deformity as early as 13 months post removal. In the second case, the child’s benefits of the first osteotomy were lost within 3 years. The use of contralateral growth modulation in concurrence with osteotomy may lessen the number of osteotomy procedures but add to the existing limb length discrepancy. In most cases, the regeneration of the lost part is delayed and its extent is unpredictable. Anticipating the unpredictable regeneration of lost femoral condyle, Tercier et al. advocated reconstruction of a lost articular surface using patella and osteoarticular graft from proximal fibula.7 Either way, the outcome is never optimal or satisfactory.
The main technique through which the vascular territories have been commonly mapped is dye studies in cadavers followed by surgical dissection or high-resolution imaging. The infantile nature of post-infective vascular insult may preclude the determination of the exact sequence of events at that time and the lesion manifests only several weeks later. Either way, post-infective loss of lateral femoral condyle qualifies as one of the most disastrous sequelae of knee sepsis. The vascular hypothesis may pave the way for preventive interventions in the form of adequate hydration, anticoagulant medications, and decompressions if the site of vascular occlusion can be localized.
Conclusion
The superior lateral genicular artery-based vascular insult explains the typical anatomical pattern of post-sepsis lateral femoral condylar loss to a large extent. Advances in science may delineate the precise site in the future. This sequelae of knee sepsis results in recurrent angular deformities and is difficult to treat.
Ethical approval
The research/study approved by the Institutional Ethics Committee at Chacha Nehru Bal Chkitsalaya Delhi, number F.1/IEC/CNBC/18/01/2022/Protocol no. 104/265, dated 08th April 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Regeneration of the lower femoral epiphysis: Report of a case. J Bone Joint Surg Br. 1954;36:116-17.
- [CrossRef] [PubMed] [Google Scholar]
- Suppurative arthritis of infancy. Some observations upon prognosis and management. J Bone Joint Surg Br. 1960;42:706-20.
- [CrossRef] [PubMed] [Google Scholar]
- Disturbed epiphysial growth at the knee after osteomyelitis in infancy. J Bone Joint Surg Br. 1970;52:692-703.
- [PubMed] [Google Scholar]
- Growth disturbance after osteomyelitis of femoral condyles in infants. Acta Orthop Scand. 1984;55:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Partial destruction of the distal femoral epiphysis as a consequence of osteomyelitis: Regeneration after transplantation of a bone graft. J Pediatr Orthop. 1985;5:731-3.
- [CrossRef] [PubMed] [Google Scholar]
- “Missing” femoral condyle: An unusual sequela to neonatal osteomyelitis and septic arthritis. Radiology. 1986;161:359-61.
- [CrossRef] [PubMed] [Google Scholar]
- Loss of a condyle of the femur or tibia following septic arthritis in infancy: Problems of management and testing of a hypothesis of pathogenesis. J Child Orthop. 2012;6:319-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sequelae from septic arthritis of the knee during the first two years of life. J Pediatr Orthop. 1994;14:745-51.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic and high-resolution computed tomographic angiography study of the lateral femoral condyle flap: Implications for surgical dissection. J Plast Reconstr Aesthet Surg. 2018;71:33-43.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral femoral condyle flap: An alternative source of vascularized bone from the distal femur. J Hand Surg Am. 2015;40:1972-80.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the vascularized lateral femoral condyle flap. Plast Reconstr Surg. 2016;137:1024e-1032e.
- [CrossRef] [PubMed] [Google Scholar]
- Cadaveric and angiographic anatomical considerations in the genicular arterial system: Implications for genicular artery embolisation in patients with knee osteoarthritis. Cardiovasc Intervent Radiol. 2022;45:80-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Blood supply of the knee joint. A microangiographic study in children and adults. Clin Orthop Relat Res. 1986;208:119-25.
- [PubMed] [Google Scholar]
- Mapping the genicular arteries to provide a caution zone during knee surgery. Clin Anat. 2020;33:1049-55.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of dual plating on the vascularity of the distal femur. Bone Joint J. 2020;102:530-8.
- [CrossRef] [PubMed] [Google Scholar]





