Translate this page into:
Management of Patent Vitellointestinal Duct in Infants
Address for correspondence Rajendra K. Ghritlaharey, MS, MCh, FAIS, MAMS, DLitt, Department of Paediatric Surgery, Gandhi Medical College and Associated Kamla Nehru and Hamidia Hospitals, Bhopal 462001, Madhya Pradesh, India (e-mail: drrajendrak1@rediffmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives
This study was undertaken to investigate and review the clinical presentation, surgical procedures executed, and the final outcome of infants managed for the patent vitellointestinal duct.
Materials and Methods
This is a single-institution, retrospective study and included infants who were operated for the patent vitellointestinal duct. This study was conducted at author's Department of Paediatric Surgery during the last 20 years; from January 1, 2000 to December 31, 2019.
Results
A total of 24 infants were operated for the patent vitellointestinal duct during the study period and comprised 20 (83.3%) boys and 4 (16.6%) girls. The age of infants ranged from 7 days to 10 months, with a mean of 88.41 ± 64.9 days. Twenty-three (95.8%) infants were operated within 6 months of the age, 17 (70.8%) of them were operated within 3 months of the age. Only one (4.1%) infant was operated at the age of 10 months. Among 24 infants, 13 (54.1%) were presented with features suggestive of acute intestinal obstruction and remaining 11 (45.8%) were presented with fecal discharges through the umbilicus without intestinal obstruction. Among 13 infants who presented with acute intestinal obstruction, 12 had prolapsed bowel and 6 of them also had gangrenous bowel. Operative procedures were executed (n = 24) in the following order of frequency: (1) resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair (n = 13, 54.1%); (2) resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis (n = 9, 37.5%); and (3) resection of patent vitellointestinal duct, segment of ileum, and an ileostomy (n = 2, 8.33%). Postoperatively, two (8.3%) infants developed anastomotic leak and peritonitis one each, later on, both of them died.
Conclusion
Patent vitellointestinal duct not only present with fecal discharges through the umbilicus but half of the infants presented with prolapsed bowel and with features of acute small bowel obstruction. Delay in seeking treatment for such cases was associated with considerable morbidity and mortality and therefore the patent vitellointestinal duct should be excised at the earliest.
Keywords
infants
intestinal obstruction
omphalomesenteric duct
patent vitelline duct
patent vitellointestinal duct
vitelline duct
vitellointestinal duct
Introduction
Persistent or patent vitellointestinal duct occurred due to the complete failure of the regression of the vitellointestinal duct and reported in about 15% of all the vitellointestinal duct anomalies.1,2,3 Meckel's diverticulum is the commonest among the vitellointestinal duct anomalies and also a most common congenital malformation of the gastrointestinal tract.4,5 Most of the cases of patent vitellointestinal duct clinically present during the infancy but also reported after infancy and in older children.6,7,8 Patent vitellointestinal ducts is extremely rare in adults but have been reported in literature.9 Diagnosis is obvious in most of the cases due to the presence of omphaloenteric fistula/patent vitellointestinal duct and fecal discharges through the umbilicus. Standard therapy for the patent vitellointestinal duct is surgical resection of the patent duct with or without resection of adjacent small segment of ileum.6,7,8,10 Present study comprised of the 24 infants who were operated for the patent vitellointestinal duct, with a brief review of the literature. To the best of author's knowledge, this is the largest series on the management of the patent vitellointestinal duct, exclusively in infants.
Materials and Methods
This is a single-institution, retrospective study and included infants who were operated for the patent vitellointestinal duct. This study was conducted as author's department of pediatric surgery during the last 20 years from January 1, 2000 to December 31, 2019. Medical records of all the 24 infants were reviewed for their age, sex, clinical presentation, surgical procedures executed, postoperative major complications, and the final outcome of the infants who were operated for the patent vitellointestinal duct.
Results
Twenty-four infants were operated for the patent vitellointestinal duct during the study period. Demographic details of above 24 infants are provided in ►Table 1. Age distribution of the above infants is provided in ►Fig. 1. The mean age of infants was 88.41 ± 64.9 days, ranged from 7 days to 10 months. Clinically 11 (45.8%) infants presented with fecal discharges through the umbilicus without intestinal obstruction (►Fig. 2A-B) and 13 (54.1%) infants were presented with features suggestive of acute small intestinal obstruction. Prolapsed bowel was observed in 12 of the infants (►Fig. 3A-C). Operative findings of above infants are detailed in ►Fig. 4. Operative procedures executed for above infants are detailed in the ►Fig. 5. Right transverse supraumbilical incision and subumbilical incision were selected in equal number of infants. Postoperatively, two (8.3%) infants developed anastomotic leak and peritonitis, one each. Infant who developed anastomotic leak required reexploration. Later on, both of the above infants died during the course of management.
| Serial no. | Age | Sex | Date of operation | Presentation and clinical examination | Operative procedures executed | Result |
|---|---|---|---|---|---|---|
| 1 | 3 mo | Male | February 24, 2001 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 2 | 3 mo | Male | March 31, 2001 | Intestinal obstruction Bowel prolapse: yes bowel gangrene: yes |
Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 3 | 2 mo | Female | July 19, 2001 | Intestinal obstruction Bowel prolapse: yes bowel gangrene: yes |
Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 4 | 3 mo | Male | September 11, 2003 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 5 | 6 mo | Male | May 25, 2004 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum and ileal repair | Well |
| 6 | 3 mo | Male | September 05, 2004 | Intestinal obstruction Bowel prolapse: yes Bowel gangrene: yes |
(A) Resection of patent vitellointestinal duct, small segment of ileum and ileoileal anastomosis (B) Reexploration for anastomotic leak |
Death |
| 7 | 5 mo | Male | February 19, 2005 | Intestinal obstruction Bowel prolapse: no |
Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 8 | 2 mo | Male | September 01, 2006 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 9 | 3 mo | Female | March 01, 2008 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 10 | 2 mo | Female | June 03, 2010 | Intestinal obstruction Bowel prolapse: yes | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 11 | 4 mo | Male | May 31, 2011 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 12 | 10 mo | Male | August 11, 2011 | Intestinal obstruction Bowel prolapse: yes | Resection of patent vitellointestinal duct, wide wedge resection of ileum and ileal repair | Well |
| 13 | 3 mo | Male | January 07, 2012 | Intestinal obstruction Bowel prolapse: yes | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 14 | 4 mo | Male | January 14, 2012 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 15 | 15 d | Male | August 08, 2012 | Intestinal obstruction Bowel prolapse: yes |
Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Death |
| 16 | 6 mo | Male | January 31, 2013 | Intestinal obstruction Bowel prolapse: yes |
Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 17 | 2 mo | Male | February 20, 2014 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 18 | 4 mo | Male | June 24, 2014 | Intestinal obstruction Bowel prolapse: yes |
Resection of patent vitellointestinal duct, small segment of ileum, and ileoileal anastomosis | Well |
| 19 | 45 d | Male | October 29, 2015 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 20 | 1 mo | Male | November 03, 2015 | Intestinal obstruction Bowel prolapse: yes Bowel gangrene: yes |
Resection of patent vitellointestinal duct, small segment of ileum and ileoileal anastomosis | Well |
| 21 | 1 mo | Female | February 02, 2017 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 22 | 7 d | Male | February 28, 2018 | Intestinal obstruction Bowel prolapse: yes Bowel gangrene: yes |
Resection of patent vitellointestinal duct, segment of ileum, and an ileostomy | Well |
| 23 | 15 d | Male | November 26, 2019 | Fecal discharges through umbilicus | Resection of patent vitellointestinal duct, wide wedge resection of ileum, and ileal repair | Well |
| 24 | 1 mo | Male | December 24, 2019 | Intestinal obstruction Bowel prolapse: yes Bowel gangrene: yes |
Resection of patent vitellointestinal duct, segment of ileum, and an ileostomy | Well |
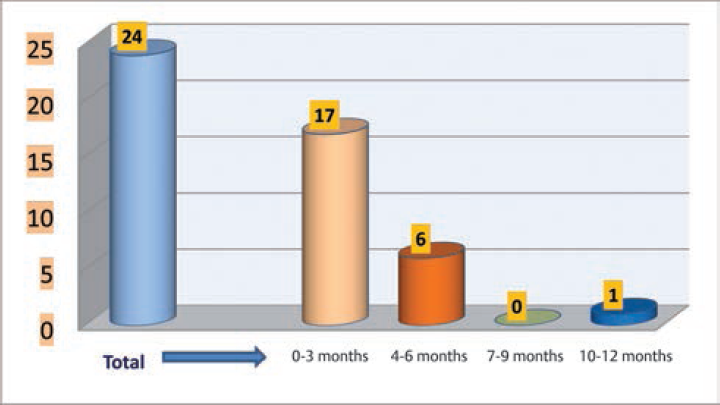
- Age distribution of infants operated for the patent vitellointestinal duct.

- (A) Photograph of an infant showing fecal discharge through the umbilicus without periumbilical redness/skin excoriation. (B) Photograph of an infant showing fecal discharge through the umbilicus with periumbilical redness and skin excoriation.

- (A) Photograph of an infant showing prolapsed of bowel mucosa through the umbilicus. (B) Photograph of an infant showing prolapsed ileum (without gangrene) through the umbilicus. (C) Photograph of an infant showing prolapsed ileum (with gangrene) through the umbilicus.

- Operative findings in infants with the patent vitellointestinal duct.

- Operative procedures executed in infants for the patent vitellointestinal duct.
Discussion
In the early weeks of fetal life the midgut loop has a wide communication with the yolk sac known as vitellointestinal duct. The vitellointestinal duct is also named as vitelline duct, omphaloenteric duct, omphalomesenteric duct, omphaloileal fistula, and umbilicointestinal fistula. It appears at the end of the fourth week, and normally disintegrates at 8 to 10 weeks of intrauterine life.1,2,3 The obliteration process of the vitellointestinal duct begins at the umbilical end of the duct and extends toward the intestine.11 The intestinal end of the vitellointestinal duct persists most frequently in the form of Meckel's diverticulum.3,4,11
Literature relating to the patent vitellointestinal duct are scanty, and the exact incidence is not known. At the Chicago Lying-In Hospital, there were 30,000 births over a period of 10 years (1937–1947). Among above 30,000 births, only two infants had complete patency of the omphalomesenteric duct, accounted for 1:15,000 (0.0066%) hospital births.12 At the St. Luke's Hospital in Cleveland, there were 31,975 births over a period of 21 years, only two babies were born with complete patency of the omphalomesenteric duct, accounted for approximately 1:16,000 (0.0062%) hospital births.12
The patent vitellointestinal ducts occurred more frequently in infants and also documented more in male as compared to females. In a retrospective analysis of 16 symptomatic cases of vitellointestinal duct anomalies, 9 were patent vitellointestinal duct, all of them were infants, and 8 of them were boy.7 In a retrospective review of 18 children of symptomatic vitelline duct anomalies over a period of 22 years, authors recorded 12 cases of patent vitelline duct.8 In another review of 36 neonates with vitelline duct pathologies, there were 11 cases of patent vitelline duct, and authors also observed male preponderance as 10:1.10 In analysis of 73 cases of symptomatic patent vitellointestinal duct anomalies, there were only 5 cases of patent vitellointestinal duct, and all of them were male infants.11 Kittle et al also documented patent vitellointestinal duct 4.4 times more in males than in females.12 In a review of 72 cases relating to the vitelline duct anomalies, there were 6 cases of patent vitellointestinal duct.13 In a series of 66 cases of anomalies relating to the vitelline duct in infants and children, authors found 20 cases of patent vitelline duct, and they also documented the above anomaly more in male.14 Amongst 217 children relating to the vitelline duct anomalies, there were only 4 cases relating to the patent vitelline duct, and all of them were neonates.15 Present study on patent vitellointestinal ducts included only infants. Among 24 infants, 23 (95.8%) were 7 days to 6 months of age, and only one boy was of the age of 10 months. This study documented 20 males, with a male–to-female ration of 5:1, and further support that the above anomaly is more frequent in male.
Clinical presentation varies from the discharges of mucus, flatus, and feces through the umbilicus to the acute small intestinal obstruction.6,7,8 Prolapse of the bowel (ileum) through the umbilicus/patent vitellointestinal duct is the gravest complication relating to the untreated cases, and reported in as many as 50% of the cases.6,11,16,17 Yamada et al in a review of Japanese literature observed that 28 cases had prolapsed bowel amongst 53 cases of patent vitellointestinal duct.6 In Kirtland, in a review of 131 documented cases of patent vitellointestinal duct, 28 of them had prolapsed bowel.11 Present report of patent vitellointestinal ducts also documented that 50% of the infants had prolapsed bowel. Prolapse of the bowel through the umbilicus is probably related to the luminal diameter of the patent vitellointestinal duct. Author strongly believe that the wider the lumen of the patent vitellointestinal duct, the more the chances of the bowel prolapse, but smaller lumen size does not guarantee that there would not be a bowel prolapse.
There are two options for the surgical resection of the patent vitellointestinal duct: (1) resection of the patent vitellointestinal duct along with wide wedge resection of the ileum and ileal repair; and (2) resection of the patent vitellointestinal duct, adjacent small segment of ileum, and ileoileal anastomosis.6,7,8,10,13,17 Above surgical procedures can be accomplished through the subumbilical incision, infraumbilical incision, transumbilical approach, or supraumbilical right transverse abdominal incisions. Surgical procedures done through the umbilicus and subumbilical incision carries the best cosmetic results. Resection of the patent vitellointestinal duct along with wide wedge resection of the ileum and ileal repair is feasible in many of the cases of patent vitellointestinal duct. In this technique, there are chances of ectopic mucosa that may be left behind in native ileum.7 Therefore resection of the patent vitellointestinal duct, small segment of ileum and ileoileal anastomosis is a better option.7 The timing of surgical resection of the patent vitellointestinal duct is very crucial. Most of the authors suggested an early surgical intervention to prevent morbidity in the form of bowel prolapse and intestinal obstruction.
Postoperative complications may occur following the surgical procedures done for the resection of the patent vitellointestinal duct and are anastomotic leak, septicemia, peritonitis, and postoperative intestinal obstruction/adhesion.6,8,11 Mortality has also been reported following the surgical procedures done for the patent vitellointestinal duct and documented more in children who had prolapsed bowel.6,8,11 There were two (8.3%) deaths in present study, and both of the infants had major postoperative complications.
Conclusion
Patent vitellointestinal ducts not only present with fecal discharges through the umbilicus but also present with prolapsed bowel and features of acute small bowel obstruction in as many as 50% of the cases. Patent vitellointestinal duct should be excised at the earliest, as delay in seeking treatment was associated with considerable morbidity and mortality. Surgical resection of the patent vitellointestinal duct along with small segment of ileum and ileoileal anastomosis is preferable over wide-wedge resection of ileum and ileal repair.
Note
This study was presented at Paediatric Surgeons Club in Bhopal on September 21, 2019.
Conflict of Interest
None declared.
References
- Omphalomesenteric duct remnants. In: Puri P, Höllwarth M, eds. Pediatric Surgery: Diagnosis and Management. Berlin, Germany: Springer 2009:491-496.
- [CrossRef] [Google Scholar]
- Meckel's diverticulum and other omphalomesenteric duct remnants. In: Wyllie R, Hyams JS, eds. Pediatric Gastrointestinal and Liver Disease. 4th ed. Philadelphia, PA: Elsevier-Saunders 2011:572-575.
- [CrossRef] [Google Scholar]
- Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99(10):501-505.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018;97(35):e12154.
- [CrossRef] [PubMed] [Google Scholar]
- Patent omphalomesenteric duct: a case report and review of Japanese literature. Asia Oceania J Obstet Gynaecol. 1989;15(03):229-236.
- [CrossRef] [PubMed] [Google Scholar]
- Vitellointestinal duct anomalies in infancy. J Neonatal Surg. 2016;5(03):30.
- [CrossRef] [PubMed] [Google Scholar]
- Patent vitelline duct as a cause of acute abdomen: case report of an adult patient. Turk J Gastroenterol. 2011;22(01):101-103.
- [CrossRef] [PubMed] [Google Scholar]
- Vitelline duct pathologies in neonates. North Clin Istanb. 2018;5(03):211-215.
- [CrossRef] [PubMed] [Google Scholar]
- Remnants of the vitello-intestinal duct; a clinical analysis of 88 cases. Arch Dis Child. 1953;28(137):1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Persistent omphalomesenteric duct; incidence relative to Meckel's diverticulum. Am J Surg. 1952;83(05):680-685.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical study of vitelline duct and vessel remnants. J Korean Assoc Pediatr Surg. 1998;4(01):27-33.
- [CrossRef] [Google Scholar]
- Remnants of vitelline duct: analysis of 66 cases. Acta Paediatr Acad Sci Hung. 1978;19(02):113-123.
- [Google Scholar]
- Vitelline duct anomalies. Experience with 217 childhood cases. Arch Surg. 1987;122(05):542-547.
- [CrossRef] [PubMed] [Google Scholar]
- Patent omphalomesenteric duct and its relation to the diverticulum of Meckel. Arch Surg. 1947;54(01):10-36.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic omphalomesenteric duct remnants in children. Pediatr Int. 2010;52(03):480-484.
- [CrossRef] [PubMed] [Google Scholar]





