Translate this page into:
Radiological imaging of a giant sinonasal ossifying fibroma
* Corresponding author: Adity Prakash, MD Radiodiagnosis, Department of Radiodiagnosis, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India. prakashadity26@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prakash A, Yadav M, Sen KK, Satapathy G. Radiological imaging of a giant sinonasal ossifying fibroma. Ann Natl Acad Med Sci (India). doi: 10.25259/ANAMS_98_2024
Abstract
Ossifying fibroma is a rare benign fibro-osseous tumor that usually involves the maxilla or the mandible. X-ray and computed tomography (CT) is indispensable in characterizing these tumors and determining their extent of involvement. Magnetic resonance imaging (MRI) is useful in assessing orbital and intracranial extension. In this case report, we describe a rare giant juvenile variant of ossifying fibroma of the sinonasal tract in a 17-year-old boy, spanning across the nasal cavity, frontal, ethmoid and maxillary sinuses, and even extended posteriorly through the choana into the nasopharynx.
Keywords
Computed tomography
Fibro osseous tumor
Magnetic resonance imaging
Ossifying fibroma
Sinonasal
INTRODUCTION
Ossifying fibromas are benign tumors and were first described by Montgomery in 1927.1 They belong to the spectrum of fibro-osseous tumors, which include osteomas, fibrous dysplasia, ossifying fibroma, cemento-ossifying dysplasia, and more.2 The etiology of these tumors is hypothesized to be odontogenic in origin, wherein primitive mesenchymal cells in the maxilla, mandible, or occasionally petrous bone differentiate into odontogenic epithelium, which further proliferate to form these tumors. Other authors believe these tumors to be traumatic or developmental in origin.2,3
Ossifying fibromas are most common in the younger age group, that is, 20–30 years of age, and usually involve the maxilla or mandible. They are more common in women than men, with a 2:1 female-to-male ratio. Ossifying fibroma of the sinonasal tract is rare, and only 48 cases have been reported in the literature till date.4 Sinonasal tract involvement by an ossifying fibroma is mostly seen in adults in the third to fourth decade of their life.5 However, in our case, this tumor occurred within the sinonasal tract in a 17-year-old boy, which is very rare. Most reported cases of ossifying fibroma are relatively small, confined to either maxillary or ethmoid sinus. Our case is rare in the sense that the tumor was so large that it spanned across the frontal, ethmoid as well as maxillary sinus and even extended posteriorly through the choana into the nasopharynx.
CASE REPORT
A 17-year-old boy presented to the department of ears, nose, and throat with complaints of headache, left-side nasal obstruction, left frontal swelling, and epistaxis for the past three months. The left frontal swelling was painless and gradually increased over time. There was no history of trauma, loss of consciousness, seizures, or vomiting. There were no associated comorbidities. On the anterior rhinoscopic examination, a polypoidal mass was seen bulging into the left nasal cavity which was completely obliterating the cavity. The nasal septum was deviated to the right side. The mass was also seen in the left frontal region. On palpation, the mass was hard in consistency [Figure 1]. All the laboratory markers were within the normal range. X-ray of the face and paranasal sinus AP (anteroposterior) view showed a giant calcified mass involving the left nasal cavity, left maxillary, ethmoid, and frontal sinuses [Figure 2].

- Clinical picture of the 17-year-old boy with the huge sinonasal mass. Swelling (red arrow) can be seen in the left frontal region, representing the frontal sinus component of the mass. Mass was also seen within the left nasal cavity on rhinoscopy (not shown).
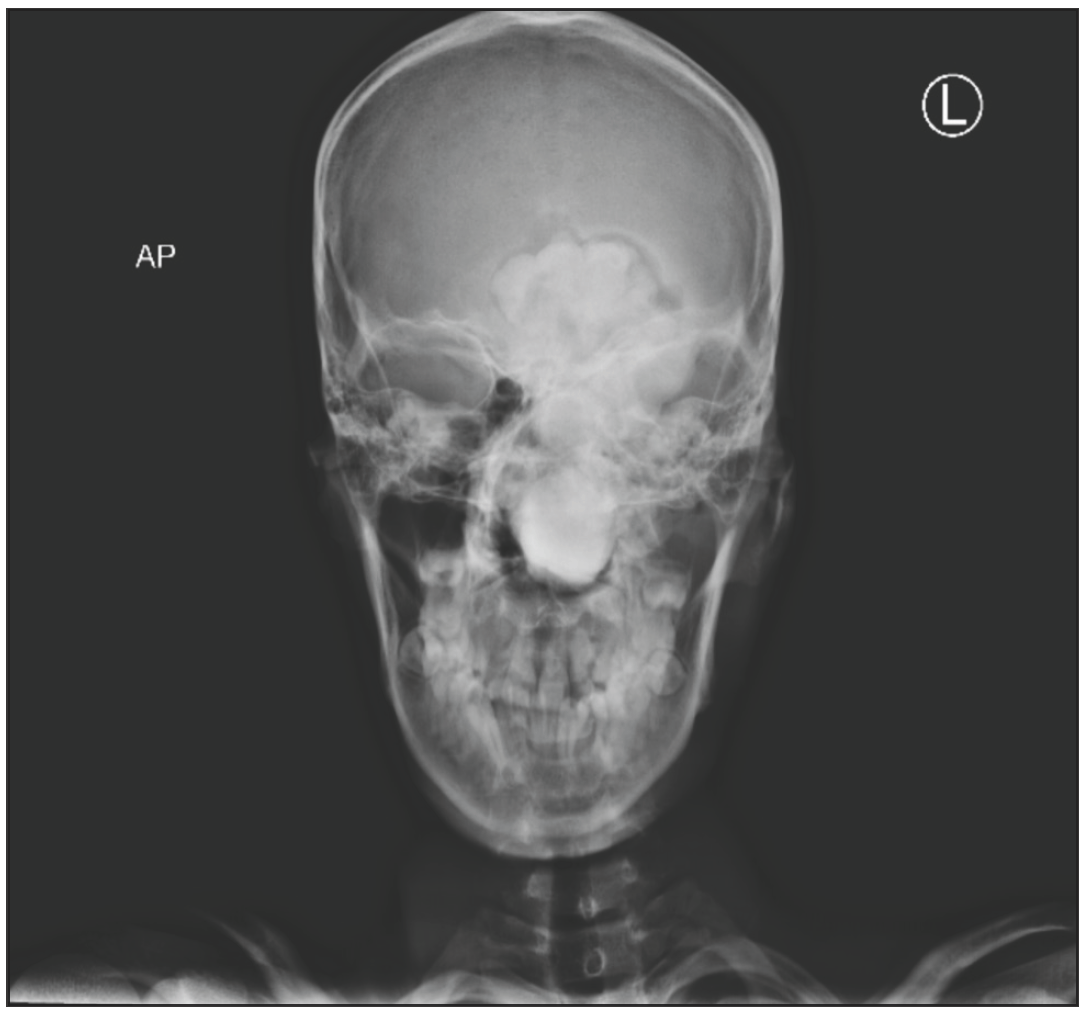
- X-ray face and paranasal sinus; AP view shows a calcified expansile mass, occupying the left nasal cavity, left maxillary sinus, left ethmoid sinus, and the left frontal sinus. AP: Anteroposterior view.
On computed tomography (CT), there was a large expansile mass occupying the entire left nasal cavity. A portion of the mass was grossly calcified. Other portions of the mass showed a ground glass matrix. A small noncalcified soft tissue component was also visible in the periphery of the mass. The mass was extending superiorly into the left ethmoid and the frontal sinus. Laterally, the mass extended through the osteomeatal unit into the medial aspect of the left maxillary sinus. The rest of the maxillary sinus was opacified with secretions due to a blocked drainage pathway. Medially, the mass was displacing the nasal septum toward the right side. Posteriorly, the mass was prolapsing through the left choana into the nasopharynx. The mass was mildly bulging the medial wall of the left orbit. However, no intraorbital extension was seen. A focal area of bony erosion was seen in the posterior wall of the left frontal sinus [Figure 3].
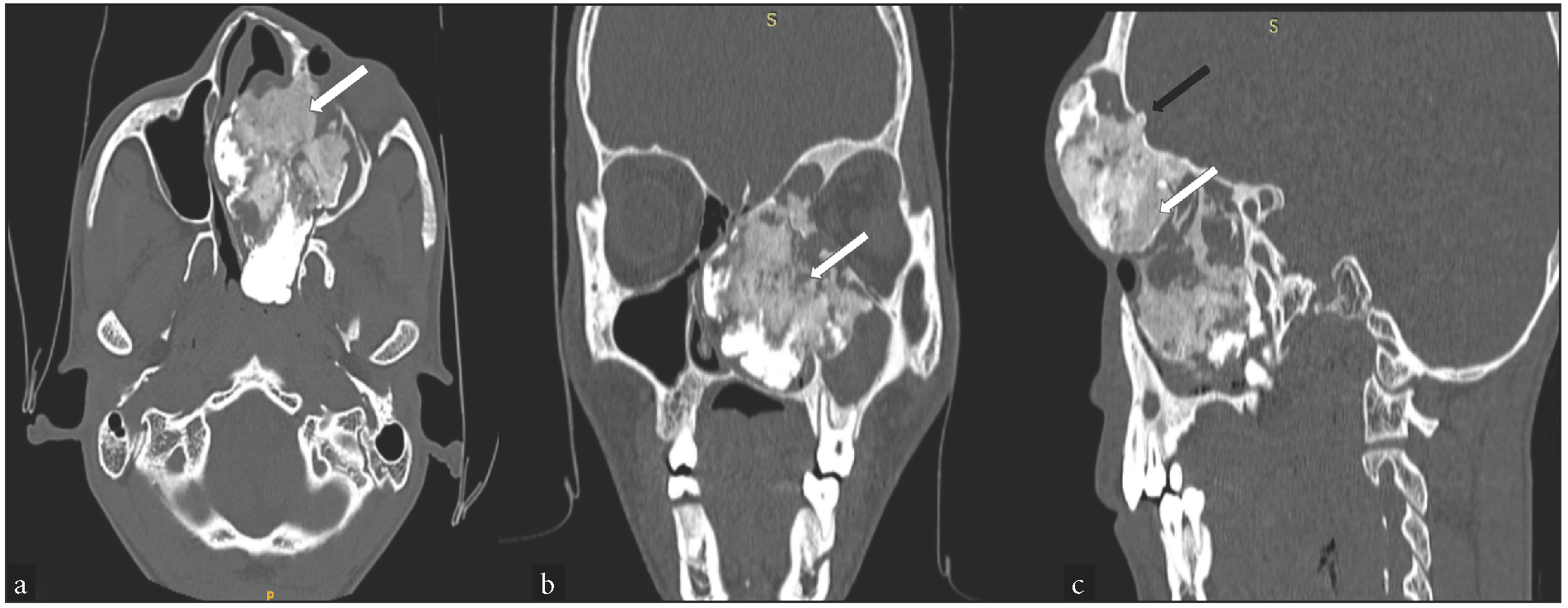
- (a) Axial CT scan shows that the mass (white arrow) contains densely ossified, ground glass and noncalcified components. (b) Coronal CT shows the extent of the mass. Note that the medial wall of left orbit is deviated but no orbital wall erosion is present. (c) Sagittal section shows focal erosion in the posterior wall of the left frontal sinus (black arrow). (b,c): White arrow signifies the mass. CT: Computed tomography.
Magnetic resonance imaging (MRI) was done to look for intraorbital and intracranial extension. On MRI, the heavily calcified portion of the mass was T1 and T2 hypointense, whereas the lesser calcified and soft tissue component of the mass was intermediate and hyperintense, respectively, on T2 weighted sequence. MRI also demonstrated the bony erosion in the posterior wall of the left frontal sinus. However, only extra-axial extension was present, while no intra-axial extension was seen. No obvious involvement of the left orbit was seen [Figure 4].
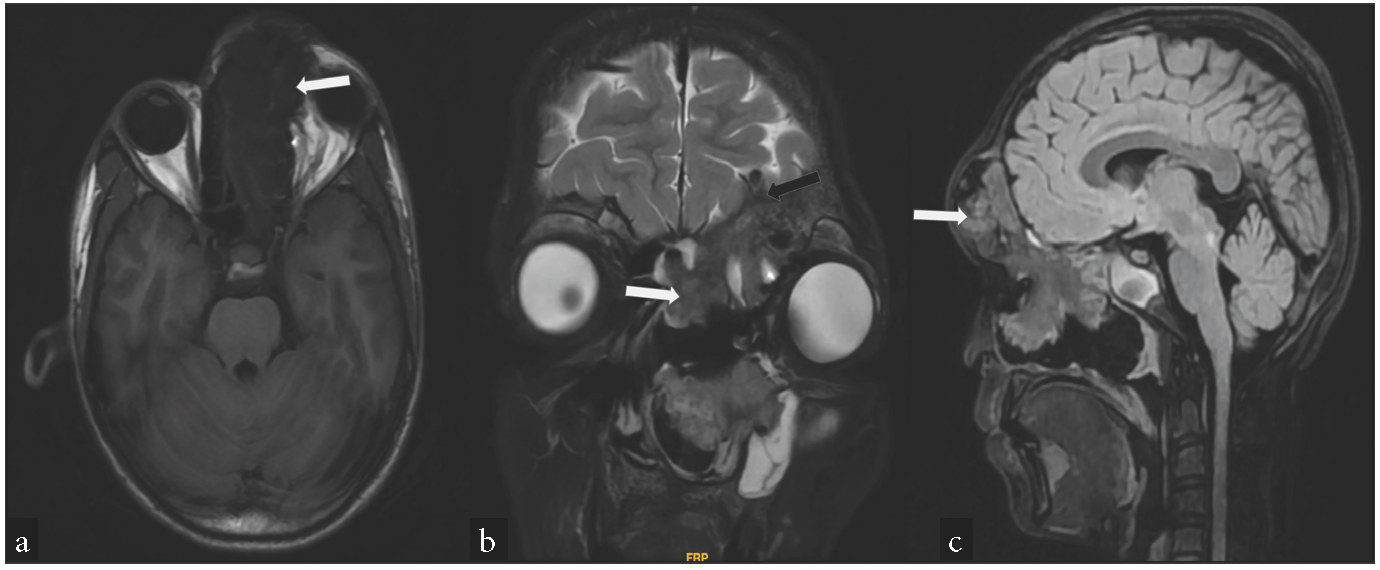
- (a) T1 weighted axial MRI shows a hypointense sinonasal mass (white arrow). (b) Coronal T2 FS image shows mixed signals. Some portions appear T2 hypointense, some are intermediate, while few areas are T2 hyperintense. The orbit is not involved (white arrow). (c) Sagittal FLAIR FS image shows the entire extent of the mass
(white arrow). FLAIR FS: Fluid-attenuated inversion recovery, FS: Fat suppression
A transnasal biopsy of the mass revealed variable sizes of woven and lamellar bone along with fibroblastic proliferation and osteoblastic rimming. There was no atypia or mitosis seen. These features were suggestive of a benign fibro-osseous lesion morphologically consistent with ossifying fibroma [Figure 5]. The patient underwent bifrontal flap incision with excision of the tumor with cranioplasty and duraplasty. The bifrontal flap was elevated, revealing the hard bony tumor extending to the paranasal sinuses. The tumor was nonvascular and non-suckable. Transnasal endoscopic debulking of the mass was performed with due care to avoid injury to the anterior skull base. The postoperative period was uneventful. The patient was advised on a regular follow-up to look for any regrowth.
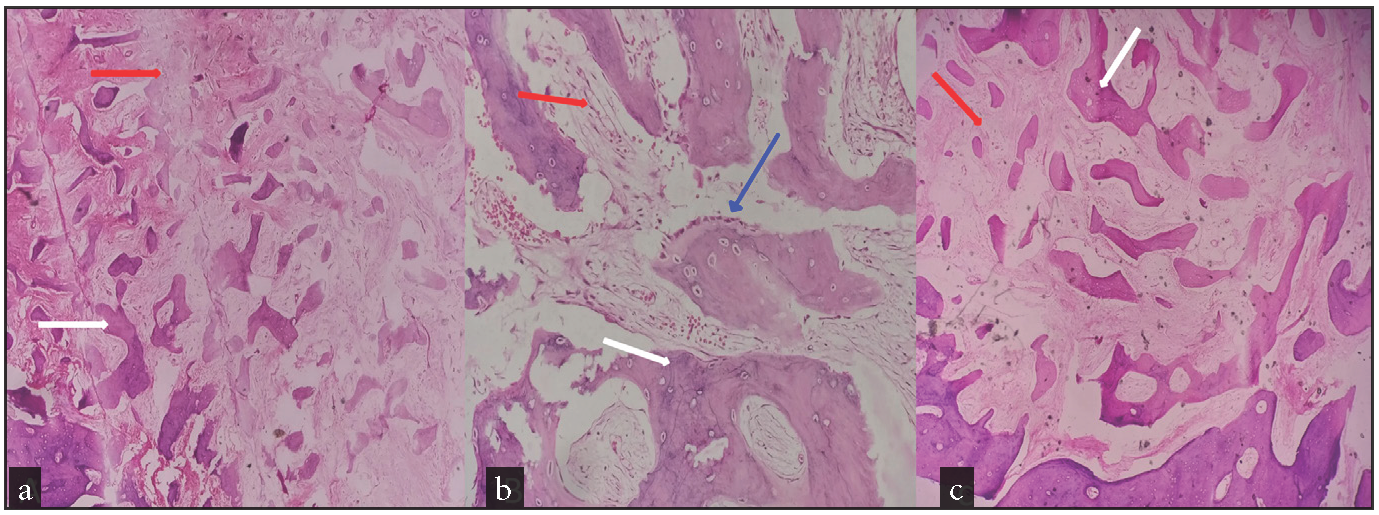
- Histopathology slides of the biopsy specimen. (a) There is proliferation of fibrous tissue containing trabeculae of woven bone, (H&E stain 100x magnification). (b) Multiple anastomotic strands of bony trabeculae are seen and osteoblastic rimming is present, (H&E stain 400x magnification). (c) Variable sizes of woven and lamellar bone with fibrous tissue. Red arrows denote fibrous tissue, white arrows denote mature bony trabeculae, and blue arrows show osteoblastic rimming, (H&E stain 200x magnification). H&E: Hematoxylin and eosin stain.
DISCUSSION
Ossifying fibromas come under the umbrella of fibro-osseous tumors. Other tumors that are included in the spectrum are osteomas and fibrous dysplasia. In the literature, multiple nomenclatures have been used for various fibro-osseous tumors, including osteoma, ossifying fibroma, and cemento-ossifying dysplasia. Some of these names overlap, and thus, there has been confusion among clinicians, radiologists, and pathologists as to the accurate subtyping of these tumors. In general, osteomas contain only the woven bone without any fibrous component, whereas ossifying fibroma has both osseous as well as fibrous components. Fibrous dysplasia is the expansion of the diploic space of bone by fibro-osseous tissue. On biopsy, fibrous dysplasia and ossifying fibroma may look similar. Here, radiology comes to the rescue, as it helps to delineate ossifying fibromas as calcified mass having distinct margins with the adjacent bone, whereas fibrous dysplasia is essentially contained within the diploic space of a normal bone and blends diffusely with the normal bone.6
Involvement of the sinonasal tract by ossifying fibroma is rare, and when it occurs, it is generally reported in the 30–40-year age group.5 However, in our case, the sinonasal ossifying fibroma was found in a 17-year-old young male. It is of note that a particular “juvenile” variant has been reported to be particularly aggressive in behavior and has a tendency to recur after excision.7 In our case also, the mass was found in an adolescent boy and led to bony erosions along the skull base, thus affirming its aggressive behavior. Hence, we believe this to be a juvenile variant of ossifying fibroma.
The symptoms of ossifying fibroma depend on the degree of involvement of the surrounding structures. When confined to the sinonasal cavity, it can present with headache, nasal obstruction, epistaxis, and nasal or facial deformity. In the case of aggressive tumors, the orbit may be involved and proptosis and other ocular abnormalities may be the predominant symptom. They may have intracranial extension through the anterior skull base.8
The diagnosis is primarily based on clinical examination, radiology, and histopathology. On CT, they are seen as calcified masses. CT shows the status of the surrounding bones and the characteristic osseous matrix of these tumors, whereas MRI is excellent in delineating the intraorbital and intracranial extension. MRI also shows the triple signal intensity, that is, hypointensity, isointensity, and hyperintensity, within the mature calcified, partly calcified, and noncalcified portions, respectively. Few case reports have demonstrated fluid-fluid levels within the ossifying fibroma on MRI. Few authors believe this to be due to the secondary aneurysmal bone cyst changes within the tumor.6 Bone scans show them as hot spots with intense uptake owing to the florid osteoblastic activity.
The various differentials which may mimic these tumors on imaging are osteoma, fibrous dysplasia, inverted papilloma, and osteosarcoma. Osteomas consist of only osseous tissues and do not have any soft tissue component, whereas ossifying fibromas have both fibrous as well as ossified regions. In our case, ground glass matrix and noncalcified soft tissue components were noted within the tumor in addition to the calcified portion. As already explained, in fibrous dysplasia, the lesion blends diffusely with the normal bone, whereas ossifying fibromas have distinct margins with the adjacent bone.6 Inverted papillomas arise from the lateral nasal wall and may extend into the sinuses. Although there may be mild calcification within an inverted papilloma at the site of its attachment to the turbinate, such gross calcification does not occur. Osteosarcomas of the sinonasal tract are rare, and by the time they reach such immense size, they would lead to erosion of adjacent bones and extra-compartmental extension.4
Various treatment options are available for ossifying fibromas. Small asymptomatic ossifying fibromas may be followed under a “wait and watch” policy. Symptomatic tumors may be treated either by an open or an endoscopic curettage or resection. With the current advances in endoscopic surgeries and routine use of navigation protocols, endoscopic surgery has become popular and safer nowadays. Subtotal resection may lead to tumor recurrence, especially in case of the juvenile variant of ossifying fibroma. Hence, whenever possible, a complete resection of these tumors must be done in order to avoid recurrence. However, at times, a complete resection may not be possible, especially when the tumor involves the frontal sinuses, as in our case. In such cases, an overenthusiastic attempt to complete resection may lead to injury to the anterior skull base and complications such as cerebrospinal fluid leak. Preoperative embolization of these tumors have been discouraged by a few authors owing to reports of visual loss following embolization, as these tumors often share arterial supply with the ophthalmic arterial network.9,10
CONCLUSION
To conclude, ossifying fibromas are rare benign fibro-osseous tumors that may affect the sinonasal tract. Imaging, including X-ray, CT, and MRI, may help characterize these tumors, show their extent of involvement, and help differentiate them from other tumors of the head and neck region.
Author’s contributions
AP: Prepared the manucript; MY: Collected data related to the case; KKS: Conceptualized the idea and design; GS: Supervised the overall work.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Ossifying fibroma of the middle turbinate: A case report. Am J Otolaryngol. 2004;25:377-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ossifying fibroma of the ethmoid involving the orbit and the skull base. Otolaryngol Head Neck Surg. 2005;133:158-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ossifying fibroma of maxilla in a male child: Report of a case and review of the literature. Natl J Maxillofac Surg. 2011;2:73-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ossifying fibroma of the ethmoid sinus: Report of a rare case and review of literature. J Res Med Sci. 2011;16:841-7.
- [PubMed] [PubMed Central] [Google Scholar]
- Psammomatoid ossifying fibroma of sinonasal tract. Otolaryngol Head Neck Surg. 2006;134:705-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sinonasal ossifying fibroma with fluid-fluid levels on MR images. AJNR Am J Neuroradiol. 2003;24:1639-41.
- [PubMed] [PubMed Central] [Google Scholar]
- Maxillary sinus ossifying fibroma. Am J Otolaryngol. 1997;18:419-24.
- [CrossRef] [PubMed] [Google Scholar]
- Ossifying fibromas of the paranasal sinuses: Diagnosis and management. Acta Otorhinolaryngol Ital. 2015;35:355-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute visual loss after preoperative embolization of an ethmoidal metastasis. Int Ophthalmol. 2012;32:165-9.
- [CrossRef] [PubMed] [Google Scholar]





