Translate this page into:
Review of benign skull vault lytic lesions: A case of desmoplastic fibroma—rare but not to be forgotten
*Corresponding author: Dr. S Shanmuga jayanthan, DNB Radiology, Department of Radiology, Meenakshi Hospital, Nilagiri, Therkku Thottam, Thanjavur, Tamil Nadu, India. jettan.32@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shanmuga Jayanthan S, Arathi N, Nadanasadharam K, Rupesh G. Review of benign skull vault lytic lesions: A case of desmoplastic fibroma—rare but not to be forgotten. Ann Natl Acad Med Sci (India). doi: 10.25259/ANAMS_28_2024
Abstract
A wide variety of benign and malignant tumors affect the skull bone. However, desmoplastic fibroma (DF) is an extremely rare benign tumor with locally aggressive behavior described in the literature. Herein, we report a case of parietal bone DF in a young male patient.
Keywords
Desmoplastic fibroma
Lytic skull lesion
Skull bone lesion
INTRODUCTION
Desmoplastic fibroma (DF) of bone is the osseous counterpart of soft tissue fibromatosis. This benign tumor of the bone is very rare and is often confused for a malignant lesion. Though non metastasizing, it is extremely invasive; thus, mimicking an aggressive bone lesion.
CASE REPORT
A 37-year-old male patient presented with a bony swelling in the left parietal bone of the skull for two years. There was a slow and progressive increase in size of the swelling without any associated pain. There was no history of fever. Patient is a known diabetic for 15 years and hypertensive for two years. He had a past history of right middle cerebral artery infarct, which was managed conservatively. Patient was referred to computed tomography (CT) brain scan.
Plain CT brain scan showed a solitary, well-defined, expansile lytic lesion in the left parietal bone measuring 4.7 × 2.3 cm [Figure 1]. There was no intracranial extension of the lesion. The outer and inner cortices were intact. Further imaging with contrast CT could not be performed as the patient’s renal function test was abnormal. The differential diagnoses in this case include Brown’s tumor (in the background of chronic kidney disease [CKD]), hemangioma, and less likely malignancy.
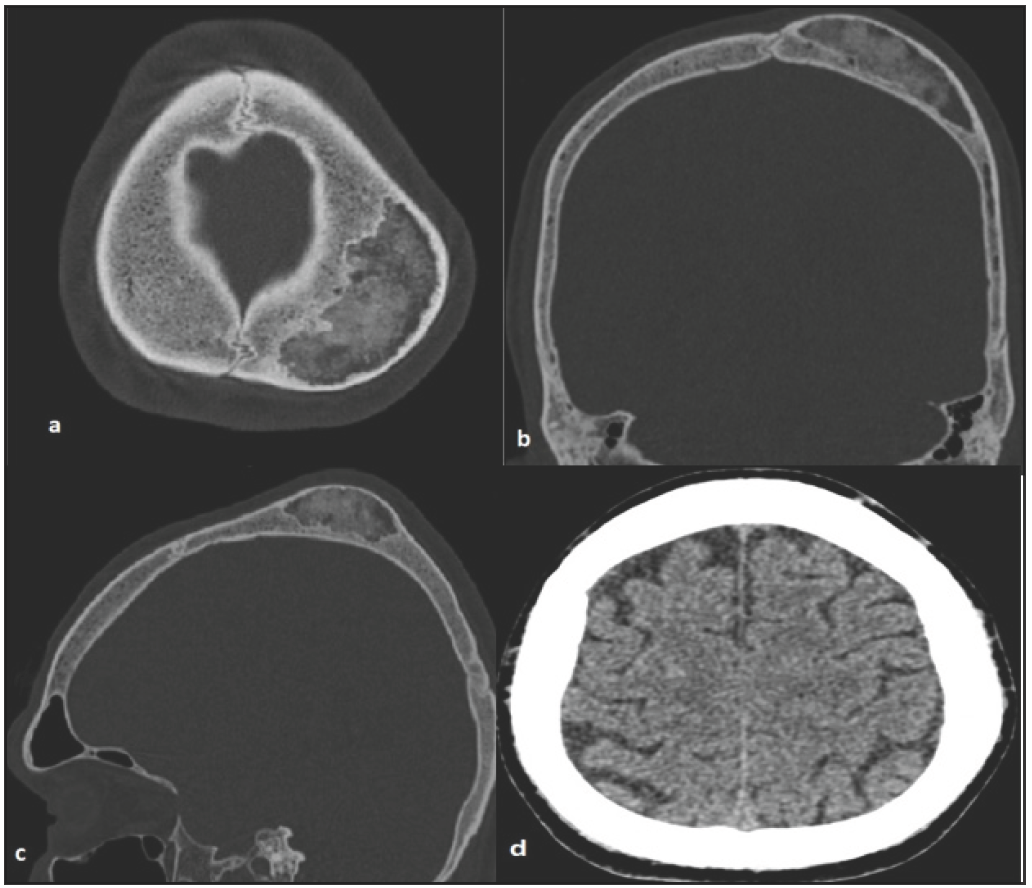
- (a-c) CT brain axial, coronal, sagittal bone window shows a well defined osteolytic lesion with mixed matrix. Thinning of outer cortex noted. No inner cortex breech noted. (d) CT brain scan axial soft tissue window shows no parenchymal extension. CT: Computed tomography.
Tumor excision was planned to confirm the diagnosis, as further imaging with contrast could not be performed due to elevated renal parameters, followed by titanium mesh cranioplasty. The excised sample was sent for histopathological examination. Multiple sections of the lesion were examined after subjecting the bone to a decalcification procedure. The sections were stained with routine hematoxylin and eosin. The sections showed a hypocellular lesion comprised of bland spindle cells with abundant collagenous stroma. The lesion occupied the spaces between the bony trabeculae, which displayed cement lines. There were no hypercellular areas, necrosis, or mitoses. Histopathology confirmed the diagnosis of DF [Figure 2].

- (a) shows a microphotograph of the lesion under low power (x100) stained with H and E and spindle cells without any pattern with collagen fibers in between. Small bony bits are also seen. (b) shows a microphotograph of the lesion under high power (x400) stained with H and E. Spindle cells are seen scattered with thick collagen fibers staining pink. H and E: Hematoxylin and eosin stain
DISCUSSION
Intradiploic skull vault lesions can be benign or malignant, but are often an incidental finding. Diagnosis of osteolytic lesions of the skull vault can be challenging as the imaging features overlap for many pathologies. Skull X-ray is usually the first diagnostic tool, but its application is limited due to more accurate imaging modalities, like CT and magnetic resonance imaging (MRI).1
Intradiploic epidermoid cyst is the most common benign lytic lesion of the skull in all age groups.1 Although mostly benign, malignant transformation can occur on rare occasions. It is characterized by diffusion restriction in the MRI and does not show enhancement in the post contrast study.1
Hemangiomas are benign vascular tumors common in the skull, which are slow growing and expansile lesions seen in the CT scan. T1 hyperintense signals are characteristic for lipid rich hemangioma. A contrast study is helpful as it demonstrates the intense postcontrast enhancement in CT and MRI.1
Aneurysmal bone cyst (ABC) is another common lytic skull vault lesion, characterized by the blood-fluid level. In the skull, ABC often occurs as a secondary phenomenon in preexisting fibrous dysplasia. The other conditions in which secondary ABC can occur include giant cell tumors, nonossifying fibromas, hemangioma, osteoblastomas, simple bone cysts, chondroblastomas, chondromyxoid fibromas, and osteosarcomas.1
DF of bone is an extremely rare tumor and the counterpart of soft tissue fibromatosis. It is common in adolescents and young adults. It is common in long bones, especially the distal femur, proximal tibia, pelvis, and mandible. Patients can present with pain. Radiologically, it appears as an expansile lesion centered in the metaphysis of long bones. Focal cortical destruction can be seen as part of the aggressive nature of the tumor, even though it is in a benign condition.2–4
However, DF is rarely described in the skull. Lee et al.3 (2012) reported frontal bone DF in a 20-year-old man, who presented with complaints of headache and swelling. The radiological diagnosis may be difficult due to the rarity of the lesion and nonspecific findings.3 Rabin et al.4 (2003) elicited a temporal bone DF in a 43-year-old woman, notably for a prolonged 12-year history, depicting the slow-growing nature of this benign tumor.
Lath et al.5 (2006) reported the first case in India of a frontal bone DF in an 18-year-old male. They found a large intradural component of the tumor extending up to the lateral ventricle, proof of the aggressive nature of the tumor.5 Kakkar et al.6 (2016) did a retrospective study of skull bone tumor over a 12-year period, the largest study on skull tumor. They noted 125 benign and malignant tumors; however, no case of DF was encountered, stating its rarity.6
DF typically presents as lytic lesions with thinning of both inner and outer tables of the skull in the CT scan. On MRI, they show the heterogeneous signal intensity on T2-weighted images and a low degree of postcontrast enhancement. However, these imaging findings are often nonspecific and histopathology remains the gold standard for the diagnosis.1,3,5 It is important to remember that the aggressive nature of the tumor can mimic lymphoma or metastasis and hence can be a diagnostic dilemma. Excision of the tumor should be done for doubtful cases.3,4
CONCLUSION
DF, although a rare skull vault lesion, should be kept as a differential diagnosis for lytic lesions of the skull vault. The aggressive nature of the tumor can be confused with malignancy on imaging; hence, histopathology being the gold standard. Excision of the tumor is mandatory in doubtful cases to exclude malignancy.
Teaching points
-
1.
DF is a benign lesion, although locally aggressive mimicking malignancy.
-
2.
Imaging features are not typical for DF; hence, histopathological correlation is needed for suspicious lesions.
Differential diagnosis for benign lytic skull vault lesions
| 1. Intradiploic epidermoid cyst |
| 2. Hemangioma |
| 3. Aneurysmal bone cyst |
| 4. Browns tumor (in the background of CKD) |
| 5. Desmoplastic fibroma |
Authors’ contributions
SSJ, NA : Conception and design, data acquisition, analysis, interpretation, drafting and revision; KN, GR: Data acquisition, analysis, interpretation, drafting and revision.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI
REFERENCES
- Spectrum of lytic lesions of the skull: A pictorial essay. Insights Imaging. 2018;9:845-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fibroblastic and fibrohistiocytic tumors. bone and soft tissue pathology: a volume in the foundations in diagnostic pathology series, expert consult. Elsevier; 2009. p. :355-66.
- Desmoplastic fibroma of the cranium in a young man. J Korean Neurosurg Soc. 2012;52:561-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Desmoplastic fibroma of the cranium: Case report and review of the literature. Neurosurgery. 2003;52:950-4; discussion 954.
- [CrossRef] [PubMed] [Google Scholar]
- Desmoplastic fibroma of the frontal bone. Neurol India. 2006;54:314-5.
- [CrossRef] [PubMed] [Google Scholar]
- Primary bone tumors of the skull: Spectrum of 125 cases, with review of literature. J Neurol Surg B Skull Base. 2016;77:319-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





