Translate this page into:
Summary of initiatives for treating congenital heart disease: Enhancing quality of life and bridging the knowledge gap
* Corresponding author: Dr. Prachi Kukshal, Department of Genomics Research, Sri Sathya Sai Sanjeevani Research Centre, Palwal, Haryana, India. drprachi.kukshal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ahamad S, Kukshal P. Summary of initiatives for treating congenital heart disease: Enhancing quality of life and bridging the knowledge gap. Ann Natl Acad Med Sci (India) 2025;61:40-4. doi: 10.25259/ANAMS_242_2024
Abstract
Congenital heart disease (CHD) represents a significant global health concern, contributing to high infant mortality rates, particularly in low and middle-income countries (LMICs) like India. The primary obstacles that need to be addressed include low awareness, delayed diagnosis and referral, unavailability, inaccessibility, and unaffordability of essential medical care, high patient volumes, lack of dedicated research, and widespread malnutrition. In this web-based literature review, we aim to highlight the critical gaps in healthcare access for CHD by summarizing the disease burden and identifying organizations and initiatives that offer free cardiac interventions throughout India.
Keywords
Cardiac centers
Congenital heart disease
Free of cost
India
Schemes
CONGENITAL HEART DISEASE—CURRENT SCENARIO AND NEED–SUPPLY GAP
According to the Global Report of Birth Defects, approximately 7.9 million children are born annually with various birth defects, of which about 1.35 million cases are attributed to congenital heart disease (CHD), which ranks as the fourth leading contributor to global infant mortality, especially in low and middle-income countries (LMICs).1 The lack of access to congenital cardiac care and malnutrition are believed to be the primary barriers to progress in addressing CHD [Figure 1]. Evidence suggests that over 90% of patients could survive to a healthy adult life if they received timely screening, diagnosis, and treatment.2 While around 40% of fetal CHD cases can be detected by prenatal sonography, factors such as the tester’s expertise, equipment sensitivity, fetal positioning, and maternal obesity can affect the accuracy.3
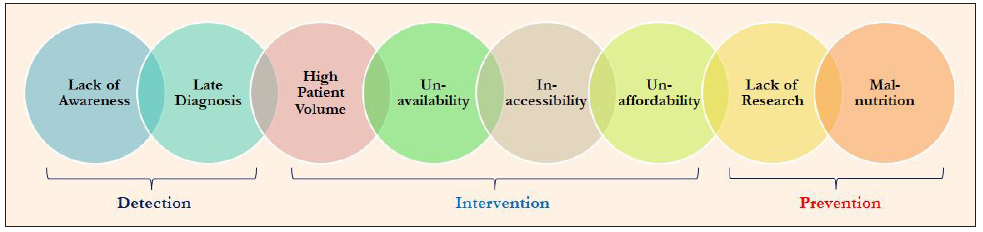
- Need–supply gap in pediatric cardiac care.
Unfortunately, nearly 90% of children born with CHD do not have lack to essential diagnostic services. Also, costly interventions, which can range from INR 1.75 to 4.25 lakhs (USD 2,050 to 5,050) can be yet other impediment.4–6 In Asia, the healthcare infrastructure is strikingly inadequate, with one cardiac center catering to 16 million people, resulting in a surgery ratio of only 0.5 per million in LMICs.2 In India, CHD affects 1 in 100 live births, resulting in roughly 0.3 million cases annually.7 Among these, at least 50,000 children require early intervention. However, only about one-fourth receive surgical treatment.8 The majority of cases are concentrated in Northern and Eastern India, where birth rates are comparatively higher.7
Saxena et al. (2020) prepared guidelines for the indications and timing of interventions for CHD within the Indian context, advocating for comprehensive physical and clinical examinations, echocardiograms, chest X-rays, and echocardiography as essential diagnostic tools.9 However, the availability of pediatric cardiac surgeons remains critically low, with only around 4,000 surgeons available globally, including ∼300 in India, serving about 90 cardiac centers.10,11 Financial constraints further worsen the high disease burden; World Bank’s Poverty, Prosperity, and Planet Report 2024 indicates that around 129 million individuals live in extreme poverty.12 Most pediatric cardiac facilities are located in major metropolitan areas, leaving a significant proportion of families affected by CHD in rural regions with limited access to medical care. A study conducted in Kerala, India, highlighted that half of the families borrowed money post-surgery to cover expenses during the follow-up period.13 Moreover, inadequate quality of care can result in higher morbidity and mortality rates than the absence of care altogether.
ORGANIZATIONS AND GOVERNMENT SCHEMES TO HEAL LITTLE HEARTS ACROSS INDIA
The public–private partnership (PPP) model, involving collaboration between hospitals, government entities, charitable non-governmental organizations, and corporate partners, has proven to be an effective strategy for building capacity and ensuring the sustainability of pediatric cardiac programs in India [Table 1].
| Scheme/Program | Implementing agency | Benefits |
|---|---|---|
| Ayushman Bharat (Pradhan Mantri Jan Arogya Yojana)14 | Govt. of India |
Financial assistance up to INR 5 lakhs/year Approximately, 1929 procedures including CHD for patients of any age group Covers cost of pre-hospitalization, medication, laboratory investigations, boarding and lodging, and 15 days’ post-hospitalization follow-up care |
| Rashtriya Bal Swasthya Karyakram15 | Govt. of India | Comprehensive screening and treatment of 4Ds—defects at birth, diseases, deficiencies and development delays for children (0–18 years) |
| Janani Shishu Suraksha Karyakram16 | Govt. of India |
Free care of pregnant woman and sick newborns 30 days after birth Covers cost of delivery, diagnostics, boarding and lodging, blood transfusion, and round-trip from home to hospital cost |
| Rashtriya Arogya Nidhi17 | Govt. of India |
Suffering from disease related to heart, kidney, liver, cancer, etc. Provides financial assistance up to INR 2 crores to economically weaker patients of any age group living below poverty line (BPL) |
| Sishu Saathi Scheme18,19 | Govt. of West Bengal | Free cardiac and neurosurgeries for children (0–12 years) |
| Hridyam for little hearts20 | Govt. of Kerala | Registry to screen and treat CHD children (0–18 years) |
| Rajiv Aarogyasri Scheme21 | Rajiv Aarogyasri Health Care Trust and Govt. of Telangana |
Approximately, 1672 procedures including CHD Financial assistance up to INR 10 lakhs/year to BPL patients of any age group |
| Ilam Sirar Irudhaya Padukappu Thittam (Adolescent Cardiovascular Protection Program)22 | Govt. of Tamil Nadu | Screening and treatment of CHD for children (0–18 years) |
| Delhi Arogya Kosh (DAK)23 | Govt. of NCT of Delhi |
Suffering from any illness including CHD Financial assistance of up to INR 5 lakhs (in govt. hospitals only) to patient of any age group with annual income up to INR 3 lakhs, along with diagnostics cost for ultrasound, ECHO, EEG, EMG, TMT, Doppler studies, and Mammography |
| Heart Care Program for CHD24 | Govt. of Assam |
Free screening, investigations, and surgeries for CHD of children (0–18 years) with annual income up to INR 6 lakhs Covers travel and accommodation cost |
| Mahatma Jyotirao Phule Jan Arogya Yojana25 | Govt. of Maharashtra |
Approximately, 34 medical specialties including cardiac care Financial assistance up to INR 5 lakhs/family/year for BPL patient of any age Covers cost of pre-hospitalization, medication, laboratory investigations, blood transfusion, boarding and lodging, and travel |
| Mukhyamantri Himachal Health Care Scheme (HIMCARE)26 | Govt. of Himachal Pradesh | Financial assistance up to INR 5 lakhs/year for BPL and other underprivileged patient of any age |
| Mukhyamantri Amrutum Yojana27 | Govt. of Gujarat | Covers surgery cost of cardiovascular, neuro, burns, poly trauma, cancer, renal, and neonatal diseases to BPL patients of any age |
| Mukhyamantri Chiranjeevi Swasthya Bima Yojana28 | Govt. of Rajasthan |
Covers surgical cost of cancer, heart, neuro, organ-transplantation, Covid-19, black fungus, etc. Financial assistance up to INR 25 lakhs to patients (0–75 years) with annual income up to INR 8 lakhs |
| Dr. NTR Vaidya Seva Scheme29 | Govt. of Andhra Pradesh |
Covers cost of admission, consultation, medical tests, medicine, surgery, boarding and lodging, travel, and 10 days’ post-discharge follow-up care Financial assistance up to INR 5 lakhs to patient of any age with annual income up to INR 5 lakhs |
| GIVE Model6 | Sri Sathya Sai Health and Education Trust | Covers cost of screening and treatment of CHD patient of any age along with free boarding and lodging along with free fetal echocardiography and maternal-child care across India |
| Public Charity30 | Hans Foundation | Financial assistance for treatment of CHD and other diseases to underserved patient of any age across India |
| Save Little Hearts31 | Genesis Foundation | Financial assistance for treatment of CHD children (0–18 years) with annual income up to 2.4 lakhs across India |
| Little Hearts Program32 | Being Human—The Salman Khan Foundation | Financial assistance for treatment of underprivileged CHD children (0–18 years) in remote areas across India |
| Making Heart Smile33 | Child Heart Foundation | Financial assistance for screening and treatment of BPL CHD children (0–18 years) across India along with training and education |
| Save a Heart Program34 | Fortis Foundation | Financial assistance for screening and treatment of underprivileged CHD children (0–18 years) across India |
| Healing Hearts with Compassion35 | Amrita Heart Care Foundation | Financial assistance for treatment of CHD children (0–18 years) across India |
CHD: Congenital heart disease, ECHO: Echocardiogram, EEG: Electroencephalogram, EMG: Electromyography, NCT: National capital territory, TMT: Treadmill test
A notable example of such a partnership is Hridyam, a web-based application launched by the Kerala government in 2017. This initiative collaborates with both private and government hospitals to facilitate the registration of children suspected of having CHD for early treatment.36
Another classic model is the GIVE framework—Government, Institutions and Individuals, Values, and Engagements—proposed by Sri Sathya Sai Sanjeevani Hospitals (India)—an initiative of the “Sri Sathya Sai Health and Education Trust (SSSHET).” This model aims to not only provide sustainable care for CHD patients but also ensure scalability across regions [Figure 2].6 The present study is conducted at the Sri Sathya Sai Sanjeevani Research Centre Palwal (Haryana)—a Department of Scientific and Industrial Researc (DSIR)-recognized Scientific and Industrial Research Organization (SIRO), a research arm of SSSHET, which focuses on unraveling the causal factors of CHD.

- Different domains to address the comprehensive care of congenital heart disease.
Current data indicate that government schemes and PPP initiatives cover approximately 40% and 20% of surgical care, respectively, while families are responsible for funding around 35% of interventions.7 A recent survey conducted at 24 hospitals across India examined the sources of funding for pediatric cardiac interventions in both government and private hospitals. The findings revealed that government schemes funded ∼55.3% in government hospitals and 42.9% in private institutions, while additional government aid accounted for 17.6% and 5.3%, respectively. Family funding represented 24.9% in government hospitals and 31.9% in private ones.37
CONCLUSION
Nearly 20% of CHD patients require cardiac interventions within their first year, highlighting the critical need of early diagnosis and timely treatment. Addressing CHD is essential for achieving Sustainable Development Goals 3.2 and 3.4 which aim to reduce child and premature deaths from noncommunicable diseases by one-third by 2030, as CHD accounts for one-third of all birth anomalies.
Efforts to enhance the care of children with CHD must be integrated by research that is locally relevant. Our study seeks to raise awareness of the availability and spectrum of free cardiac facilities across India, thereby assisting policymakers in making informed decisions about resource allocation in resource-limited settings to effectively mitigate the disease burden.
Furthermore, the implementation of a public–private business model can provide a pathway for sustainable and high-quality pediatric care in LMICs, ensuring that vulnerable populations receive the necessary interventions for improving health outcomes.
Acknowledgments
The authors wish to express their profound gratitude to Chairman Sir, esteemed trustees, cardiologists, surgeons, research team, management & technical team, and the entire hospital family for their unwavering commitment and selfless contribution to the noble cause of serving CHD patients totally free of cost with the motto of “Love All- Serve All.”
Authors’ contributions
SA: conceptualization, literature search, data acquisition and manuscript writing; PK: conceptualization, manuscript review and editing.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- March of Dimes global report on birth defects: the hidden toll of dying and disabled children. The March of Dimes Birth Defects Foundation; 2006. Available at https://www.prevencioncongenitas.org/wp-content/uploads/2017/02/Global-report-on-birth-defects-The-hidden-toll-of-dying-and-disabled]children-Full-report.pdf [Last accessed 2024 Oct 08]
- Global unmet needs in cardiac surgery. Glob Heart. 2018;13:293-303.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of biomarkers for congenital heart disease based on maternal amniotic fluid metabolomics. Front Cardiovasc Med. 2021;8:671191.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Congenital heart disease in low- and lower-middle-income countries: Current status and new opportunities. Curr Cardiol Rep. 2019;21:163.
- [CrossRef] [PubMed] [Google Scholar]
- Can the public-private business model provide a sustainable quality pediatric cardiac surgery program in low- and middle-income countries? World J Pediatr Congenit Heart Surg. 2023;14:316-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Free surgery for CHD through philanthropy—a sustainable model? Indian J Thorac Cardiovasc Surg 2024 Available from: https://doi.org/10.1007/s12055-024-01813-7 [Last accessed 2024 Sept 21]
- [Google Scholar]
- Congenital heart disease in India: A status report. Indian Pediatr. 2018;55:1075-82.
- [CrossRef] [PubMed] [Google Scholar]
- The outcome of surgery for congenital heart disease in India: A systematic review and metanalysis. Ann Pediatr Cardiol. 2024;17:164-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Indian guidelines for indications and timing of intervention for common congenital heart diseases: Revised and updated consensus statement of the working group on management of congenital heart diseases. abridged secondary publication. Indian Pediatr. 2020;57:143-57.
- [CrossRef] [PubMed] [Google Scholar]
- Global access to comprehensive care for paediatric and congenital heart disease. CJC Pediatr Congenit Heart Dis. 2023;2:453-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pediatric cardiology: Is India self-reliant? Ann Pediatr Cardiol. 2021;14:253-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Poverty, Prosperity, and Planet Report: Pathways out of the polycrisis. World Bank; 2024 Available at https://www.worldbank.org/en/publication/poverty-prosperity-and-planet [Last accessed 2024 Oct 07].
- Micro-economic impact of congenital heart surgery: Results of a prospective study from a limited-resource setting. PLoS One. 2015;10:e0131348.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pradhan Mantri Jan Arogya Yojana (PM-JAY). National Health Authority, Government of India. Available at https://nha.gov.in/PM-JAY [Last accessed 2024 Oct 15]
- Rashtriya Bal Swasthya Karyakram (RBSK). Ministry of Health and Family Welfare, Government of India. Available at https://rbsk.mohfw.gov.in/RBSK/ [Last accessed 2024 Oct 15].
- Janani Shishu Suraksha Karyakaram (JSSK). Ministry of Health and Family Welfare, Government of India. Available at https://nhm.gov.in/index4.php?lang=1&level=0&linkid=150&lid=171 [Last accessed 2024 Oct 15].
- Rashtriya Arogya Nidhi (RAN). Ministry of Health and Family Welfare, Government of India. Available at https://mohfw.gov.in/sites/default/files/RAN_Guideline_2019.pdf. [Last accessed 2024 Oct 15].
- Public-private partnership for treatment of congenital heart diseases: Experiences from an Indian state. World J Pediatr Congenit Heart Surg. 2024;15:439-45.
- [CrossRef] [PubMed] [Google Scholar]
- Sishu Saathi. Government of West Bengal. Available at https://wb.gov.in/government-schemes-details-sishusaathi.aspx [Last accessed on 2024 Oct 16].
- Hridyam. National Health Mission, Government of Kerala. Available at https://hridyam.kerala.gov.in/#doc [Last accessed 2024 Oct 12].
- Rajiv Aarogyasri Nidhi. Rajiv Aarogyasri Health Care Trust and Government of Telangana. Available at https://www.rajivaarogyasri.telangana.gov.in/ASRI2.0/ [Last accessed 2024 Oct 12].
- Ilam Sirar Irudhaya Padukappu Thittam (Adolescent Cardiovascular Protection Program). Government of Tamil Nadu. Available at http://164.100.117.80/sites/default/files/Heart%20Surgery%20Programme%20for%20School%20Children%20in%20Tamil%20Nadu.pdf [Last accessed 2024 Oct 13].
- Delhi Arogya Kosh (DAK). Directorate General of Health Services, Government of NCT of Delhi Available at https://dgehs.delhi.gov.in/dghs/delhi-arogya-kosh [Last accessed 2024 Oct 15].
- Heart Care Program for Congenital Heart Disease. National Health Mission, Health and Family Welfare, Government of Assam. Available at https://nhm.assam.gov.in/schemes/free-operations-for-children-having-congenital-heart-disease [Last accessed 2024 Oct 15].
- Mahatma Jyotirao Phule Jan Arogya Yojana (MJPJAY). Government of Maharashtra. Available at https://www.jeevandayee.gov.in/MJPJAY/ [Last accessed 2024 Oct 15].
- Mukhya Mantri Himanchal Health Care Scheme- HIMCARE. Himanchal Pradesh Swasthya Bima Yojna Society, Government of Himanchal Pradesh. Available at https://www.hpsbys.in/content/mmmn [Last accessed 2024 Oct 15].
- Mukhyamantri Amrutum Yojana. National Health Mission, State Health Society, Health and Family Welfare Department, Government of Gujarat . Available at https://nhm.gujarat.gov.in/mukhya-mantri-amrutam.htm [Last accessed 2024 Oct 13].
- Mukhyamantri Chiranjeevi Swasthya Bima Yojana. Government of Rajasthan. Available at https://lokpahal.org/mukhyamantri-chiranjeevi-yojana/ [Last accessed 2024 Oct 13].
- Dr. NTR Vaidya Seva Scheme. Dr. Nandamuri Taraka Rama Rao Vaidya Seva Trust, Government of Andhra Pradesh. Available at https://drntrvaidyaseva.ap.gov.in/asri [Last accessed 2024 Oct 13].
- The Hans Foundation, India. Available at https://thehansfoundation.org/ [Last accessed 2024 Oct 10].
- Save Little Hearts. The Genesis Foundation, India. Available at https://www.genesis-foundation.net/ [Last accessed 2024 Oct 11].
- Little Hearts Program. Being Human-The Salman Khan Foundation, India. Available at https://beinghumanonline.com/ [Last accessed 2024 Oct 07].
- Making Heart Smile. The Child Heart Foundation, India. Available at https://www.childheartfoundation.com/ [Last accessed 2024 Oct 07].
- Save a Heart Program. The Fortis Foundation, India. Available at https://www.fortishealthcare.com/ [Last accessed 2024 Oct 07].
- Healing Hearts with Compassion Program. Amrita Heart Care Foundation, India. Available at https://amritaheartcare.org/ [Last accessed 2024 Oct 07].
- A population health approach to address the burden of congenital heart disease in Kerala, India. Glob Heart. 2021;16:71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pediatric cardiac procedures in India: Who bears the cost? Ann Pediatr Cardiol. 2024;17:1-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






