Translate this page into:
The correlation between esophageal pressure topographic metrics and symptom severity in patients with laryngopharyngeal reflux disease refractory to proton pump inhibitors
* Corresponding author: Dr. Deepanjan Dey, MD, Department of Physiology, Armed Forces Medical College, Pune, India. ddey1976@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Raj P, Dey D, Manrai M, Pandey P. The correlation between esophageal pressure topographic metrics and symptom severity in patients with laryngopharyngeal reflux disease refractory to proton pump inhibitors. Ann Natl Acad Med Sci (India). doi: 10.25259/ANAMS_103_2024
Abstract
Objectives
Laryngopharyngeal reflux disease (LPRD) cases are usually diagnosed based on a reflux index score of over 13 and are then treated by a 12-week intervention with proton pump inhibitors (PPIs). However, many such patients also have associated primary motility disorders when subjected to high-resolution esophageal manometry, and therefore analysis of the latter may reveal correlations of its metrics, if any, with the symptom severity after proton-pump therapy.
Material and Methods
Patients with LPRD (41) having a reflux index score of 13 and above were treated with a 12-week regimen of PPIs. Of them, 23 did not show significant improvement in their scores, while the remaining 18 did. Both these groups of patients were then subjected to high-resolution esophageal manometry. Various esophageal pressure topographic metrics were recorded and analyzed for participants from both groups.
Results
The most common manometry finding among participants from both groups was an esophageal motility pattern with all topographic metrics falling within the normal limits. Patients with high reflux symptom scores but normal esophageal motility had normal esophageal topographic metrics regardless of their response to PPIs. However, median basal lower esophageal sphincter pressure, median integrated relaxation pressure, and median distal contractile integral were found to be very strongly correlated to the symptom severity scores among the patients who responded to therapy.
Conclusion
Symptom severity scores provide a general guideline for clinicians to initiate a 12-week regimen of PPIs to which many of the patients of LRPD eventually respond. In addition, high-resolution manometry identifies those cases having an associated primary motility disorder but does not provide information on whether the high symptom severity scores are because of these disorders, reflux or a combination of both. While esophageal pressure topographic metrics by far do not single out laryngopharyngeal disease from a group of patients with mixed disorders, a few of these metrics do have a strong correlation with the changes in the symptom severity scores following a 12-week intervention with PPIs. Thus, high-resolution manometry should be performed in such patients as an adjunct for a more robust diagnostic armamentarium.
Keywords
Esophageal pressure topographic metrics
High-resolution manometry
Laryngopharyngeal Reflux disease
Reflux symptom index
INTRODUCTION
Laryngopharyngeal reflux disease (LPRD) manifests with a spectrum of symptoms ranging from a mild pharyngeal globus to severe frank dysphonia.1 While being regarded as an atypical form of the wider entity that is gastroesophageal reflux disease (GERD), LPRD is now considered an altogether distinct and independent disease having its own pathophysiology.2 Extensive review of available literature does not yield a conclusive and consensus-oriented approach to the definitive role of proton pump inhibitors (PPIs) in the management of LPRD, other than an empirical trial for eight to 12 weeks.1,3 LPRD, as confirmed by the popularly used reflux symptom index (RSI) scoring, laryngoscopy, and a 24-hour ambulatory pH-metry has been recommended to be followed up with a trial of PPIs.4 However, pH-metry does not describe the pressure topographic metrics of the esophageal body or the lower esophageal sphincter (LES). Moreover, hypopharyngeal-esophageal multichannel intraluminal impedance pH-metry (HEMII-pH) has been recommended as a more reliable tool for detecting LPRD, as compared to dual channel pH-metry.5 The facility for HEMII-pH, however, is highly restricted, even in the developed world. In order to delve deeper into the mechanism of the motor pathophysiology of the body of the esophagus and its sphincters, LPRD patients have been subjected to high-resolution manometry (HRM) with the objective of studying the amplitudes of esophageal peristalsis and LES behavior. It has been revealed that LES pressures were reduced in such patients, along with an increased duration of LES relaxation.6 It has also been found by way of HRM, that LPRD patients with high RSI scores (>13) have weaker or absent esophageal peristalsis and, hence, abnormal esophageal motility.7 After deliberating upon all available evidence on the subject matter, the International Federation of Otorhinolaryngological Societies (IFOS) consensus recommends HRM studies only in LPRD patients predominantly having esophageal symptoms and in those who might be manifesting LPRD as a result of an underlying esophageal dysmotility.8 However, the consensus does not clarify whether such an underlying esophageal dysmotility could possibly be a reason for PPI refractoriness.
Reckoning only the RSI scores for its diagnosis and symptom severity, the prevalence of LPRD in India has been found to be around 11%, with no significant difference between the sexes.9 The medical subject headings (MeSH) thesaurus search with the words ‘laryngopharyngeal reflux” and ‘prevalence” yields additional information on the worldwide prevalence. Information gathered from the first page of the search reveals a study reporting the prevalence based on the RSI as well as the reflux finding score (RFS) as 18.4 in Tanzania,10 while another RSI-based multi-centric cross-sectional study on more than an astounding 90,000 LPRD cases yields a prevalence of 14.09% in China.11 The first page of the MeSH search does not reveal any study conducted in the Americas, but does show an older study reporting the prevalence based on RSI to be as high as 18.8% among the Attican Greeks.12 Whatever the ethnic and geographical variations in prevalence, it is evident that LPRD is a common disease affecting individuals across the globe, including those in India. However, research in Indian sub-populations with LPRD has not received the kind of attention that such a vast and diverse demography of the subcontinent deserves. It is therefore strongly felt that research directed towards the pathophysiology of LPRD needs to be given its due in order to address the requirement of the community in general and to the patients in particular.
With the data on the prevalence of LPRD being largely based on RSI, the relationship between the latter and esophageal motor pathophysiology is still limited. Added to it is the fact that resistance to PPIs remains a matter of concern for such patients and their treating clinicians. The present study was designed with the objective of establishing a relationship, if any, between the various esophageal topographic metrics and symptom severity in LPRD patients who are refractory to PPI trials.
MATERIAL AND METHODS
This multidisciplinary, single-center, cross-sectional, descriptive study was conducted jointly by the departments of otorhinolaryngology (ENT), physiology, and gastroenterology of a tertiary care medical institute. After obtaining the necessary ethical approval from the Institute Ethics Committee, informed consent was obtained from fresh cases of LPRD, who in turn were drawn out of the patients reporting to the department of ENT with symptoms suggestive of the disease over a span of 18 months, from September 2022 to February 2024. Patients less than 18 years of age were excluded, and so were those with clinical, endoscopic, or pH-metric evidence of GERD, other esophageal motility disorders, and evidence of past surgery involving the gastrointestinal tract. Dual probe 24-hour ambulatory pH-metry was not undertaken because the latest algorithm recommended by the IFOS consensus8 does not mention it but prefers the HEMII-pH instead. The latter, in turn, is not yet available at this center, or anywhere else in the vicinity, for that matter. Patients who had been on PPIs for any other reason within the last three months were also excluded. After a provisional diagnosis of LPRD was made on the basis of history and clinical examination, each patient was administered with the RSI scoring system. An RSI score > 13 was considered significant for the diagnosis of LPRD. Patients (49) who were found with RSI > 13, were then prescribed PPIs for 12 weeks, following which they were advised to review. Of them, 41 patients reported after eight weeks of PPI therapy for review, while the remaining eight patients were lost to follow-up. RSI scoring was repeated for all 41 patients after eight weeks of PPI therapy. Despite PPI therapy, 23 out of the 41 patients continued to have an RSI > 13, whereas the remaining 18 reported significant relief from symptoms, as evidenced by the values of their RSI being < 13. All 23 patients who were refractory to PPIs underwent upper gastrointestinal endoscopy, which was performed to rule out structural lesions. No structural lesions were detected in them, except for three patients who were coincidentally found to be having hiatus hernia. The remaining 18 patients with RSI < 13 also underwent endoscopy as a preliminary test preceding HRM. Thus, 23 patients refractory to PPIs were placed in Group A, and the remaining 18 were placed in Group B. All patients from Groups A and B thereafter underwent HRM. HRM was not performed prior to the initiation of PPI therapy because the results obtained therein would have identified and filtered out the patients with primary motility disorders and, along with them, LPRD patients with overlapping pathophysiology, and also because PPIs were unlikely to alter the HRM metrics in most patients with primary motility disorders.
HRM in all patients was performed in the gastrointestinal motility laboratory in the department of physiology and reported by the same intervention physiologist, with the help of a 16-channel water perfusion manometer (High-Resolution Manometry System, M/s Royal Melbourne Hospital, Parkville, Melbourne, Victoria, Australia). The HRM catheter was introduced through the nose and further negotiated along the esophagus into the stomach, with its tip positioned to the gastric lumen in a manner that allowed its distal high-resolution zone to traverse the LES. After allowing for initial stabilization and baseline settings, all channels were referenced to the intragastric pressures. A series of 5 mL drinking water swallows were then given to the patients in supine and upright positions, respectively, and real-time pressure topographic recordings of the esophageal peristalsis and LES were made. The esophageal pressure topographic metrics thus obtained were subjected to analysis by the built-in software (Trace! Oesophageal 1.3.4 (c), Royal Melbourne Hospital, Melbourne, Victoria, Australia), and swallows were classified as per the laid down Chicago Classification 4.0 guidelines (CC v4.0).13 The metrics obtained were basal LES pressure (BLESP), esophago-gastric junction contractile integral (EGJ-CI), integrated relaxation pressure (IRP), and distal contractile integral (DCI). The data sets obtained were tabulated and subjected to appropriate statistical analysis.
RESULTS
RSI scores before and after the PPI interventions have been summarized in Table 1. HRM topographic metrics, as obtained from the patients following the PPI intervention have been summarized in Table 2. Non-normal distribution of data was obtained by applying the Shapiro-Wilk test of normality, while the paired T-test was done using the Wilcoxon rank sum test for comparison of RSI scores before and after PPI intervention, both of which have been summarized in Table 3. Initial RSI scoring among the Group A non-responders (NR) and the Group B responders (R) showed no significant difference between the groups. However, significant changes in RSI score were seen in the R group as compared to the NR group following the PPI intervention. Gender differences in motility patterns are depicted in Figure 1, while specific motility patterns as per CC v4.0 among NR and R groups are depicted in Figure 2. Finally, the correlation plots depicting the strength and direction of the association between RSI scores and HRM indices are depicted in Figure 3.
| RSI scores | Response to PPI | Median | SD |
p-value (RSI before PPI versus RSI after PPI) |
|---|---|---|---|---|
| RSI before PPI | R | 21.0 | 4.70 | |
| RSI after PPI | R | 10.0 | 1.47 | <0.001* |
| RSI before PPI | NR | 20 | 6.83 | |
| RSI after PPI | NR | 19 | 5.07 | 0.669 |
RSI scores before and after PPI in responders (Group B) and non-responders (Group A) were compared using the Wilcoxon rank sum test because the Shapiro-Wilk test did not show a normal distribution of data. p-value <0.05 was considered significant. There is a significant reduction in RSI scores in Group B after PPI treatment as compared to Group A.
SD: Standard deviation, RSI: Reflux symptom index, PPI: Proton pump inhibitors. *Significant p-value.
| HRM indices | Motility pattern on HRM | Median | SD |
|---|---|---|---|
|
Median BLESP (mmHg) |
EGJOO | 8.50 | 3.54 |
| Normal esophageal motility | 11.50 | 3.60 | |
| Ineffective Esophageal Motility (IEM) | 12 | 3.62 | |
|
EGJ-CI (mmHg.cm) |
EGJOO | 34.00 | 2.83 |
| Normal esophageal motility | 29.50 | 10.39 | |
| Ineffective Esophageal Motility (IEM) | 22 | 6.88 | |
|
Median IRP (mmHg) |
EGJOO | 29.15 | 1.48 |
| Normal esophageal motility | 9.00 | 3.76 | |
| Ineffective Esophageal Motility (IEM) | 6.90 | 2.72 | |
|
Median DCI (mmHg.s.cm) |
EGJOO | 8138.50 | 2413.36 |
| Normal esophageal motility | 3407.50 | 1030.92 | |
| Ineffective Esophageal Motility (IEM) | 350 | 120.08 |
HRM indices expressed as median and standard deviation (SD) for the three motility patterns seen in both Groups A and B. EGJOO: Esophago-gastric junction outflow obstruction, BLESP: Basal LES pressure, EGJ-CI: Esophago-gastric junction contractile integral, IRP: Integrated relaxation pressure, DCI: Distal contractile integral, SD: Standard deviation, LES: Lower esophageal sphincter. HRM: High-resolution manometry.
| Variable | Statistical method and p-value | RSI after PPI | Median BLESP (mmHg) | EGJ-CI (mmHg.cm) | Median IRP (mmHg) | Median DCI (mmHg.cm.s) |
|---|---|---|---|---|---|---|
| RSI after PPI | Kendall’s tau-b | — | ||||
| p-value | — | |||||
| Median BLESP (mmHg) | Kendall’s tau-b | -0.491 | — | |||
| p-value | < 0.001*** | — | ||||
|
EGJ-CI (mmHg.cm) |
Kendall’s tau-b | -0.044 | 0.051 | — | ||
| p-value | 0.693 | 0.651 | — | |||
|
Median IRP (mmHg) |
Kendall’s tau-b |
0.460 | -0.351 | 0.210 | — | |
| p-value | < 0.001*** | 0.002** | 0.057 | — | ||
|
Median DCI (mmHg.cm.s) |
Kendall’s tau-b | 0.407 | -0.280 | 0.116 | 0.484 | — |
| p-value | < .001*** | 0.012* | 0.290 | < .001*** | — |
Correlation matrix for high-resolution manometry (HRM) indices with the RSI scores after PPI treatment among the responders (Group B). Kendall’s tau-b correlation coefficient was applied because the data did not follow normal distribution.
P-values were taken as: * p < 0.05, ** p < 0.01, *** p < 0.001. RSI: Reflux symptom index, PPI: Proton pump inhibitors, BLESP: Basal LES pressure, EGJ-CI: Esophago-gastric junction contractile integral, IRP: Integrated relaxation pressure, DCI: Distal contractile integral, LES: Lower esophageal sphincter.
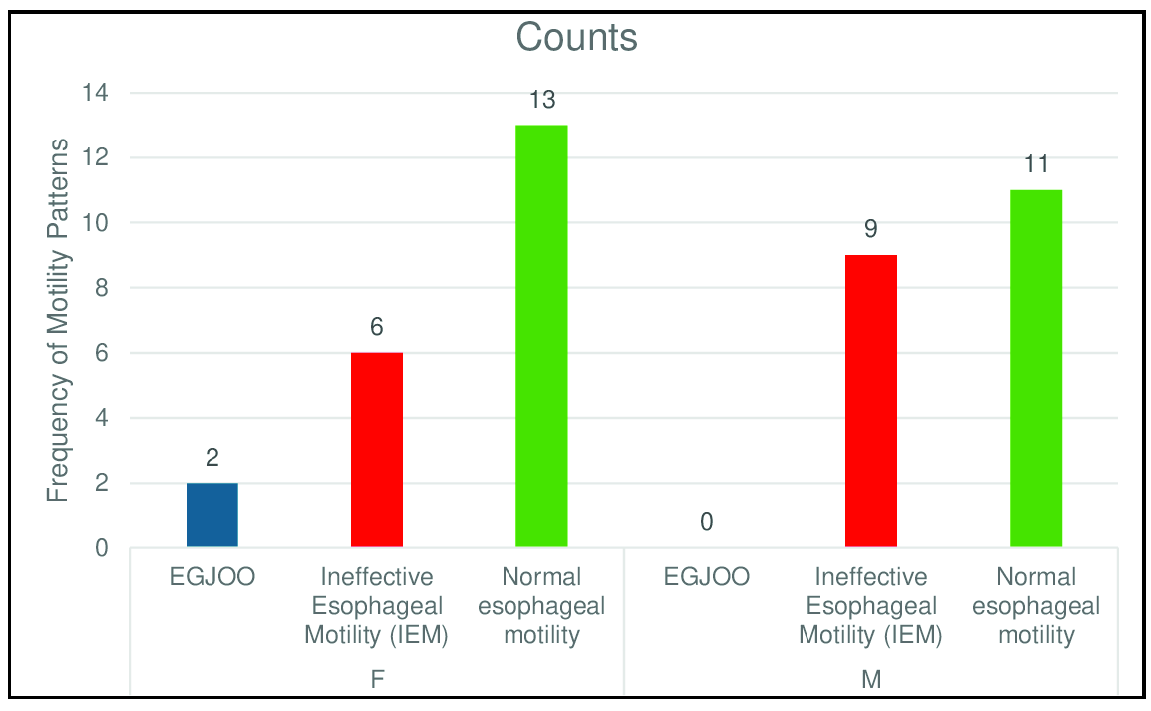
- Gender differences (Female: N=20, Male: M=20) in motility pattern observed after performing high-resolution manometry (HRM). Overall, females show a higher number of normal esophageal motility as well as esophago-gastric junction outflow obstruction (EGJOO) as compared to male participants. Numbers on bar represent the cases of specific motility disorders as detected by manometry.
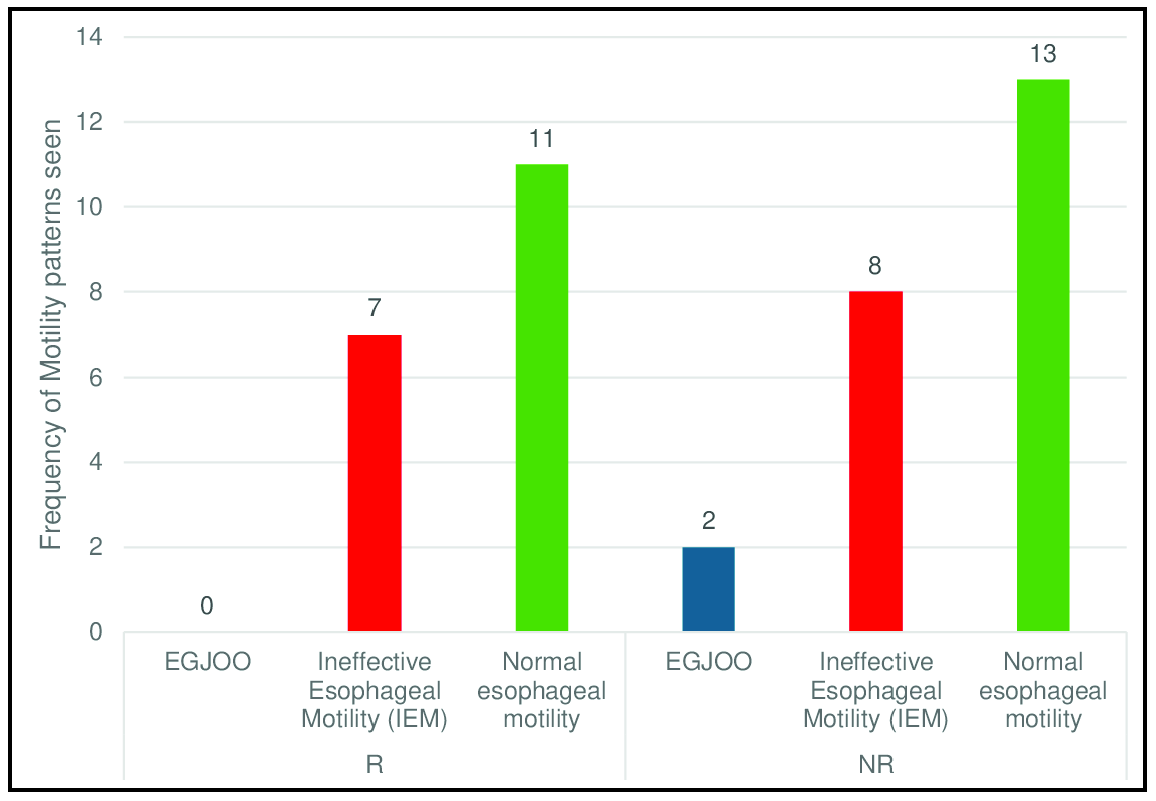
- HRM motility patterns observed in Group B (responders - R) and Group A (non-responders - NR) after performing HRM following PPI treatment. EGJOO: Esophagogastric junction outflow obstruction, HRM: high resolution manometry, PPI: proton pump inhibitors. Numbers on bar represent the cases of specific motility disorders as detected by manometry.
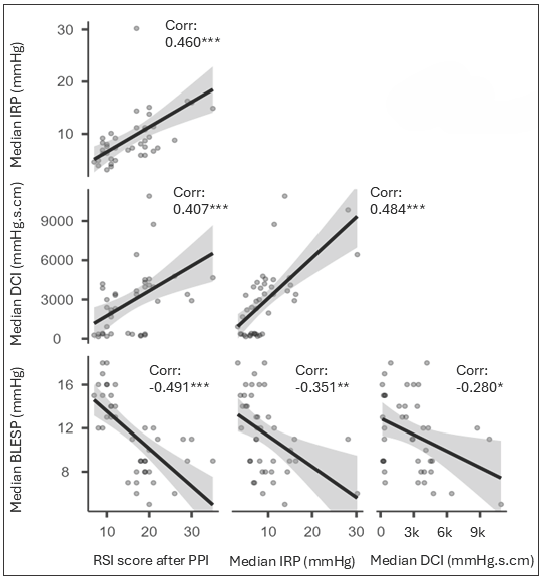
- Correlation plot depicting the strength and direction of association between reflux symptom index (RSI) scores and various manometric indices. Grey areas indicate the confidence interval bands, dots idicate the data points and solid black lines indicate the correlation trend. *p<0.05, **p<0.01, ***p<0.001. PPI: Proton pump inhibitors, IRP: Integrated relaxation pressure, DCI: Distal contractile integral, BLESP: Basal lower esophageal sphincter pressure, Corr: Correlation value.
DISCUSSION
It is evident from Table 1 that there was a predictable and significant reduction in RSI scores following PPI intervention in several patients (Group B, 18 out of 41). However, the remaining 23 patients did not show a similar improvement. Although not an objective of the study, the female preponderance noticed in patients [Figure 1] who had HRM evidence of esophago-gastric junction outflow obstruction (EGJOO) has been documented by several studies and was, therefore, an anticipated finding.14,15 EGJOO itself has been found to be present in almost one-tenth of LPRD patients when subjected to HRM analysis16, and which the present study agrees to, albeit with its limited sample size. All four LPRD patients with EGJOO were females [Figure 2], and all of them were from Group A, who did not respond to PPIs. Recent evidence supports the fact that EGJOO may manifest either secondary to reflux disease or can coexist with LPRD.17 With EGJOO being an independent motility disorder by itself, it may not be scientifically prudent at the moment to conclude in favor of a possible cause-effect relationship between it and LPRD. However, it may be explained with reasonable confidence that PPI resistance in the four female patients of EGJOO with high RSI scores was because of the simple fact that they did not have LPRD at all.
The most common HRM finding among PPI responders and non-responders was a normal esophageal motility pattern, with all the esophageal topographic metrics falling within the normal limits. In other words, a significant proportion of LPRD patients do not have a primary motility disorder, thereby alluding to a peculiar pathophysiology, which is independent of one that affects esophageal motor functions. It has, therefore, been appropriately suggested that LPRD patients with normal HRM findings usually report symptoms other than dysphagia.18 Further, failed peristalsis on HRM has been independently associated with high RSI scores, even following symptomatic relief of reflux or a normal HEMII-pH report.7 Thus, on one hand, failed peristalsis itself may cause symptoms leading to high RSI scores, which in turn can lead to an erroneous diagnosis of LPRD, while on the other, RSI scores would continue to remain high in these patients despite PPI intervention, since PPIs would treat the reflux but not the failed peristalsis, thereby misleading the clinician to classify the patient as one who is PPI-refractory. Thus, classifying patients as PPI-refractory purely on the basis of RSI scores may be premature, especially without considering HRM findings.
Attempts to tabulate the various HRM esophageal pressure topographic metrics separately for both the groups (A & B) did not yield any statistically significant difference, either in patients with normal motility or with a primary motility disorder, and so, the findings have been combined together. Thus, patients with high RSI scores but normal esophageal motility did have normal BLESPs, EGJ-CIs, IRPs, and DCIs regardless of their response to PPIs. Moreover, the available literature is lacking on whether patients with primary motility disorders who do not require surgical intervention should be administered a PPI regimen regardless of RSI scores. All patients from both groups with or without PPI response had similar HRM metrics as those without LPRD. Therefore, it is clear that primary motility disorders co-exist with LPRD.16 These metrics show that even if LPRD patients had coexisting primary motility disorders, there is no reliable HRM metric to support or refute the fact that high RSI scores are only because of LPRD. HRM performed on LPRD patients simply diagnoses a concomitant primary motility disorder, which may or may not be responsible for the associated symptoms that influence the RSI scorings.
The most significant findings of this study, however, have been summarized in Table 3. Median BLESP was found to be very strongly correlated to post-PPI RSI scores among the responders (Group B). BLESP is known to play a crucial role in the etiopathogenesis of reflux disease, especially in those with more upright than supine reflux patterns.19 It is expected to be low in LPRD patients and in those having IEM since the latter are known to have a low IRP and DCI.13 However, HRM metrics have not been shown to play a role in predicting PPI response in patients with reflux diseases.20 In the present study, the median IRP was found to be strongly correlated with post-PPI RSI scores. IRP has been found to be having the ability to differentiate IEM due to reflux from that due to a primary motility disorder.21 However, the role of IRP in predicting similar differences among LPRD patients without associated IEM remains ambiguous. The median DCI was found to be strongly correlated with post-PPI RSI scores. DCI represents the contraction vigor of the distal esophageal peristaltic wave and was initially used to differentiate the jackhammer esophagus from other forms of hypercontractile motility disorders. It denotes the median amplitude of the peristaltic wave over the distal one-third of the esophageal body over a particular duration. EGJ-CI is mathematically derived by dividing DCI by the duration of three successive respiratory cycles in seconds, and accordingly, is expressed in mmHg.cm. EGJ-CI is better suited to quantify EGJ contraction rather than the DCI. It was described almost a decade ago that EGJ-CI was also one of the best HRM parameters to differentiate PPI non-responders in reflux disease.22 Thus, EGJ-CI needs to be preferred over DCI when HRM metrics in PPI responders are considered for GERD patients. It is uncertain whether the same could hold for LPRD patients as well, especially after the present study found that EGJ-CI was not correlated with RSI scores after PPI intervention, but DCI was.
CONCLUSION
There is no doubt that RSI scores do allow LPRD patients to be initiated on PPIs, to which many of them eventually respond. HRM identifies LPRD cases which have an associated primary motility disorder but does not provide information on whether high RSI scores are due to these disorders, reflux, or a combination of both. HRM metrics, by far, do not single out LPRD cases from a group of patients with mixed disorders. However, a few of these metrics do have a strong correlation with the changes in RSI scores following a PPI intervention. Indian centers with HEMII-pH facilities are few and far between. However, HRM facilities are available in several tier two and three cities and towns in India. HEMII-pH as an investigation for LPRD cases seems impractical to be routinely carried out in India at the moment. However, the translational value of the present study is well emphasized by its inference, which reveals that the statistically significant correlation between more than one esophageal topographic metric and symptom severity scores in LPRD cases has the potential to allow clinicians to manage LPRD better, thereby leading to improved outcomes.
Acknowledgements
The authors duly acknowledge the support of the biostatistics department of the home institute.
Authors’ contributions
DD: Overall project coordinator, study concept, study design and methodology, HRM recording, HRM interpretation, data acquisition, data management, statistical interpretation of results, manuscript preparation, manuscript editing and manuscript submission; MM: Intellectual contribution in study design, methodology, conducting pre-HRM endoscopy and barium studies, data acquisition, HRM interpretation, statistical interpretation of results, consultations with statistician, manuscript preparation and manuscript editing; PP: HRM recording, data acquisition, data storage, data assortment and management, obtaining statistical consultation, manuscript preparation; PR: Obtaining ethics approval and referring the LPRD patients for HRM.
Ethical approval
The research/study approved by the Institutional Review Board at Armed Forces Medical College, number IEC/2022/165A, dated 03rd October 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- An update on current treatment strategies for laryngopharyngeal reflux symptoms. Ann N Y Acad Sci. 2022;1510:5-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Laryngopharyngeal reflux and atypical gastroesophageal reflux disease. Gastrointest Endosc Clin N Am. 2020;30:361-76.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and management of laryngopharyngeal reflux disease: State of the art review. Otolaryngol Head Neck Surg. 2019;160:762-82.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of oropharyngeal pH-Monitoring in the assessment of laryngopharyngeal reflux. J Clin Med. 2021;10:2409.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical update findings about pH-Impedance monitoring features in laryngopharyngeal reflux patients. J Clin Med. 2022;11:3158.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Esophageal pressure and clinical assessments in the gastroesophageal reflux disease patients with laryngopharyngeal reflux disease. J Clin Med. 2021;10:5262.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Failed swallows on high-Resolution manometry independently correlates with severity of LPR symptoms. J Voice. 2022;36:832-7.
- [CrossRef] [PubMed] [Google Scholar]
- The dubai definition and diagnostic criteria of laryngopharyngeal reflux: The IFOS consensus. Laryngoscope. 2024;134:1614-24.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of laryngopharyngeal reflux disease in Indian population. Indian J Otolaryngol Head Neck Surg. 2022;74:1877-81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Laryngopharyngeal reflux disease, prevalence and clinical characteristics in ENT department of a tertiary hospital Tanzania. World J Otorhinolaryngol Head Neck Surg. 2020;7:28-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An epidemiological survey of laryngopharyngeal reflux disease at the otorhinolaryngology-head and neck surgery clinics in China. Eur Arch Otorhinolaryngol. 2020;277:2829-38.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngopharyngeal reflux disease in the greek general population, prevalence and risk factors. BMC Ear Nose Throat Disord. 2015;15:7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021;33:e14058.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical presentation and disease course of patients with esophagogastric junction outflow obstruction. Dis Esophagus. 2017;30:1-6.
- [CrossRef] [Google Scholar]
- Upright integrated relaxation pressure facilitates characterization of esophagogastric junction outflow obstruction. Clin Gastroenterol Hepatol. 2019;17:2218-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Esophageal manometry, pH testing, endoscopy, and videofluoroscopy in patients with globus sensation. Laryngoscope. 2020;130:2120-5.
- [CrossRef] [PubMed] [Google Scholar]
- Esophagogastric junction outflow obstruction (EGJOO): A manometric phenomenon or clinically impactful problem. Curr Gastroenterol Rep. 2024;26:173-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and clinical significance of esophageal motility disorders in patients with laryngopharyngeal reflux symptoms. J Gastroenterol Hepatol. 2021;36:2076-82.
- [CrossRef] [PubMed] [Google Scholar]
- 24-hour dual-probe ambulatory pH-metry findings in cases of laryngopharyngeal reflux disease. J Laryngol Voice. 2011;1:18-21.
- [CrossRef] [Google Scholar]
- Ineffective esophageal motility in chicago classification version 4.0 better predicts abnormal acid exposure. Esophagus. 2022;19:197-203.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Integrated relaxation pressure (IRP) distinguishes between reflux-predominant and dysphagia-predominant phenotypes of esophageal “absent contractility”. J Clin Med. 2022;11:6287.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-contractile integral: Normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






