Translate this page into:
Universal Health Coverage in India: Where Rubber Hits the Road?
Address for correspondence D.C. Nanjunda, D. Litt., Centre for the Study of Social Exclusion and Inclusive Policy, Humanities Block, University of Mysore, Mysore 570006, Karnataka, India (e-mail: ajdmeditor@yahoo.co.in).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Poverty and healthcare issues are the most debatable topics today. Developing countries like India have as much as 45% of its population trapped in poverty because of various urgent healthcare needs. Universal health coverage (UHC) is a unique insurance system to provide financial protection to the marginalized groups of the country. It facilitates appropriate and immediate health needs, including required diagnostic, therapeutic and operational costs. However, UHC, a unique plan which focuses on the disadvantaged sections of the society, has some serious lacunae when it comes to its implementation in real life. This includes finances and human resources. Experts are reallocating adequate budgetary expenditure on healthcare issues, and in the meantime, a shortage of skilled health manpower is hunting down the UHC scheme in India. In recent times, different state governments are increasing budget allocation for the health sector. UHC is targeting low-income and poor families, forgetting the affordable and timely healthcare by way of improving services offered at the primary health centers and rapid expansion of the skilled health manpower across the country. UHC needs to focus on health paradigm systems, including improved healthcare-seeking behavior, nutrition, sanitation, potable water, reducing maternal and infant mortality, and dissemination of information of current technology to provide quality health services to the underserved and marginalized population of the country. These changes would symbolize a real way forward toward the immediate fulfillment of UHC goals for India.
Keywords
universal health coverage
health
Ayushman Bharat
poverty
cost
quality
Introduction
In 1998, the World Health Assembly made new commitments to ‘Health for All’ for the 21st century. The commitment included, in part, “we commit ourselves to strengthen, adapting and reforming as appropriate our health systems including essential public health functions and services to ensure universal access to health services that are based on scientific evidence of good quality and within affordable limits, and that are sustainable for the future. We will continue to develop health systems to respond to the current and anticipated health conditions, socio-economic circumstances and the needs of people, communities and countries concerned to appropriately manage public and private actions, and investments in health” 1
The Government of India and State Governments have the general obligation to extend free universal health coverage (UHC) services, and ensure that the marginalized sections of the society should be in a position to obtain quality healthcare services, directly or indirectly, offered by any healthcare service provider at any given point in time. The strange thing is India is exporting software to the Western countries, but it trails in health outcomes when compared with Bangladesh and Sri Lanka! The 11th 5-year plan has set goals for reducing maternal and infant mortality, increasing child sex ratio, and reducing malnutrition among children and women in the country. The same five year includes states health for all marginalized groups at a reasonable cost. On this issue, the Government of India has set minimum standards and requisite control mechanisms or systems, focusing on paneled health providers.2
Today, health exclusion has become one of the major concerns, because of which inclusive development is not possible in a country like India. Since time immemorial, poverty and health problems are intertwined. Poverty plays a very crucial role in the onset of various simple and complicated health problems. The then planning commission had estimated that 39 million people are afflicted with various health problems just because of poverty. Around 47% in rural area and 31% in urban areas people are taking loans and selling assets just to attend to their health needs. Moreover, the same report says 20% in urban areas go untreated due to financial constraints and 30% in the case of rural India.3
Providing timely finances for the health and healthcare of the needy is a significant issue; it is the building block of any health system and critical to a well-performing healthcare system. As we know, many poor Indian states are struggling to get sufficient funding for health and healthcare needs. Moreover, many developed Indian states have still not scientifically prearranged their different health services to make sure equitable, affordable and easily accessible and universal healthcare for all walks of life and geographies.4
Also, the health sector in India suffers from inadequate funding, shortage of skilled health professionals, failure of the health programs, issues in healthcare management, weak institutional regulatory system, and neglecting traditional systems of medicines. Today, the healthcare system has become highly commercialized, and only the rich people can access quality healthcare. It is also quite evident to write that the healthcare system in the country suffers from poor health infrastructure, especially in rural and tribal settings. Even today in rural areas, people are not getting quality health services because of poor management and lack of infrastructure in rural-based government hospitals as per the recent Niti Aayog report. There are interstate disparities and differences between rural and urban health indicators in India. There is a target to provide safety, health and environment to its citizens through universal quality healthcare services, and regulatory mechanisms in the part of the private healthcare sector, by the year 2025; also, to increase the GDP allocation for the health sector gradually.5
Aayushman Bharat is an iconic UHC Program of India to fulfil its promise in the National Health Policy of 2017. Ayushman Bharat Yojana or National Health Protection Scheme is a program to provide quality healthcare services to more than half of the total underserved Indian population. The socioeconomic caste census database shall be utilized to recognize needy beneficiaries for this scheme in the country. As we know in India, expenditure on healthcare for the year 2013–2014 was about around 4.02% of the total GDP, and the government share was just 1.15% against 5.99% of the global average. The government is committed to hiking money for UHC in budgetary allocations of 2.5 percent of GDP by 2025.6 Currently, India is using 0.1% of total GDP for the health sector for the purpose of health inclusion. The National Health Policy of 2017 governments is intended to spend at least 70% of the total healthcare budget for only primary healthcare centers (PHCs) (►Figs. 1–3).
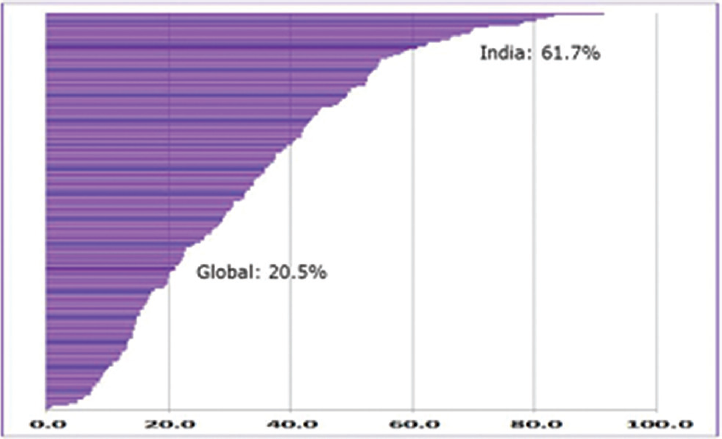
- Out-of-pocket health expenditure as proportion of total health expenditure.
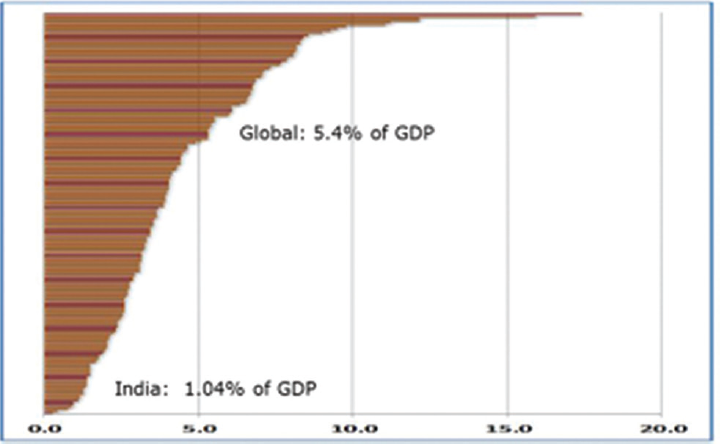
- Government health expenditure as proportion of GDP.
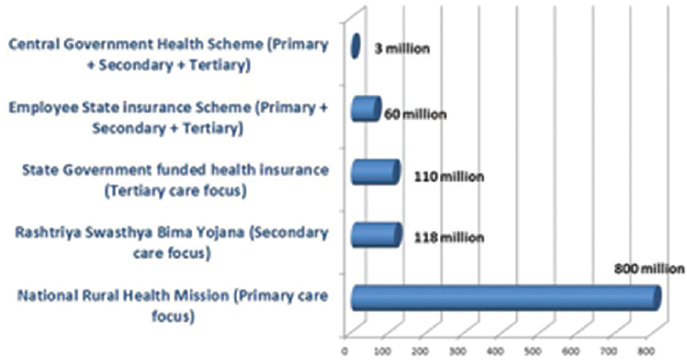
- Population coverage under various health schemes in India.
This new UHC health scheme is a much awaited health program because it reduces the catastrophic health expenditure on the part of the poor patient, and it also indirectly helps the quality services on the part of the government hospitals. Ayushman Bharat has two major segments–1. National Health Protection Scheme and 2. creation of wellness centers in place of subcenters. The national health protection scheme has two major agendas–1. pressing the need for good network among health and wellness infrastructure across the country to deliver quality healthcare services and 2. the most important point is to deliver integrated healthcare service through insurance coverage, covering, at least, 50% of India's population who are under below the poverty line or deprived sections.7
In India, the majority of marginalized sections are deprived of quality secondary and tertiary healthcare services. The basic idea of introducing a new National Health Protection Scheme is to provide cashless treatment to the marginalized people in any government or private hospitals, including secondary and tertiary healthcare services. Earlier, we had subcenters ahead of PHCs. Now, wellness centers will replace the subcenters, expecting a key role, especially in the rural parts of the country. Still, it is an unanswered question as to why people will not choose government hospitals for their health needs over a period of time despite government hospitals doing really well in some areas. Also, in India, people visiting the PHCs first would rather visit the secondary and tertiary healthcare centers directly for their various simple health needs without any referral. It is a topic for the study. In US/Europe, it is not possible, unless one has a strong referral from the lower healthcare facility.8
If the people visit the PHCs immediately for their health needs, the burden on the secondary and tertiary healthcare will automatically be reduced. Keeping this in mind, the government has created wellness centers to provide primary healthcare education and services. Meanwhile, various state governments also have introduced different health insurance schemes that should not interfere with the Ayushman Bharat scheme which cause a kind of confusion among people. There are some issues like the referral system. If anyone wants to get benefits under the Aayushman Bharat scheme in private hospitals, they must have the referral slip from any government. hospital. Here, if the required service is not available in the government hospital, only then should the patient be given the referral slip to go to the higher medical center. This is not happening. Patients pay bribes to get referral slips from government hospitals; sometimes, through political influence too. It shows people still do not have any faith in government hospitals. This leads to having a kind of institutional corruption in the scheme.9
There is one more argument that this scheme is only helpful to the insurance companies, enriching their profit. However, this concern is a totally unestablished theory to date. It is found that most of the states are actually willing to go with a legal trust mode, focusing on a high-volume, low-margin model. For insurance companies, there is a legal provision in the basic contract such that the insurance companies can make 15% profit out of the total premiums.6 Due to heavy competition and nonprofit, insurance companies are asking for comparative premiums under UHC. Another question was the lack of supply to match the demand generated after implementing the UHC scheme. Experts opine the new demand may be met through existing capacity with the private sector in a more efficient manner or government. health institutes could need more infrastructure and manpower capacity soon.10
Quality is an essential contributor to the UHC efforts with stress on grounded technical work that can be contextualized and simulated across all government hospitals. Cross-cutting technical areas with clear linkages with quality UHC is a necessity in case of public health functions and health-related issues. There is a big issue that the majority of government hospitals are providing free health services including tertiary healthcare. Still, the majority of patients are spending a lot of money from their pockets for their health needs. Hi-tech facilities are not being offered by any government hospitals including CT/MRI scans and other higher end services. Sometimes, required pathological laboratory and other diagnostic services are available even in the urban-based secondary/tertiary care government hospitals. In this situation, every patient should go to the private centers for diagnostic service, drugs and implants, according to the need. It is also better to note that all public hospitals charge a user fee for the major health issues, including heart, cancer care kidney, liver, etc.11
Health is highly unsure and changeable; moreover, it is catastrophic to the poor families. Poor households not only spend huge money for their healthcare needs but also suffer wage loss to get their health back. Some health experts have argued that this UHC scheme is not able to reduce catastrophic expenditure on the part of the patient. Hence, this is the time to doubly ensure effectively reducing catastrophic expenditure through UHC. The UHC health benefit scheme covers around Rs. 5 lakh which is sufficient to provide any type of healthcare /treatment in all types of hospitalization conditions. Moreover, this benefit package covers mostly every health condition that requires hospitalization, daycare, and surgeries, etc. The payment system has been designed to cover all the costs, and the patient is not needed to pay anything from his/her pocket at any point of time. Health economists say the scheme is going to increase the cost of healthcare. However, the proposed UHC will considerably manage the cost of health service by moving toward a high-volume, low-margin model. Hence, UHC is a really good scheme for the time being.12
Will Ayushman Bharat be affordable in the long run? The government should have brought this scheme long before, and it depends on the strong political will of the next government or available resource, or how much government is willing to spend in the future and. Several states have their ongoing healthcare schemes, and they are not showing interest in joining the current Ayushman Bharat scheme, for example, Delhi government. The scheme offers some special provisions to all the states like human resources, financial resources, state-of-the-art facilities, customizable technological platforms, implementation systems, audit systems, and effective monitoring systems at no additional cost from the state exchequer. It is generally agreed that we need to have strong information and communications (ICT) technology because every beneficiary must get nationwide network hospitals if it is required for the healthcare system.5
If we focus exclusively on the primary healthcare sector, then the burden on the secondary and tertiary healthcare will be lessened. Not only hospitals but it will also be useful to the family, mentally and financially. The ICT government must focus more on PHCs, so that any health issues can be solved if we diagnose it in an early stage. It is also found that the strategic purchasing pathway will be adopted to procure and pay for secondary and tertiary healthcare services from public and private healthcare service providers. These two ideas have now been clubbed together in the budget of 2018 to provide the required engine for the India's big plan toward UHC. However, there are some experts who opine ‘this scheme addresses the wrong problem or provide a wrong solution even if it tends to address the right problem.” The government must opt for the public–private model (PPM) and that would be the best idea for the success of the Ayushman Bharat scheme13
Health economists are of the opinion that the private sector in a UHC scheme is poorly regulated, and the government needs to focus on strengthening the obligate regulations on the part of the private sector. The purchaser of the different health services can play a vital role in making a system strong through their financial power over the private sector, and now the government is required to focus on the following segments of the UHC:
Setup price system effectively.
The proper establishment of the price regulatory mechanism.
Focusing on the quality of health services.
An incentive to the government hospital to improve quality.
Using electronic data sharing system with the help of information technology.14
The UHC should be based on the PPM system. Moreover, it ought to be noted that the government should not use its limited financial and human resources to improve health services through the private sector. This idea may not be good for the Indian health system and budget. Private people can make their presence felt in a UHC system, but their concentration will be only toward the profit motive. Determine understanding and the part of both the government and private sector, so that the private sector should make use of their capacity, skill, and financial issues in providing quality service to the marginalized sections of the society. The private sector in health healthcare issues is required for their well-organized and capable network. They must go for reasonable prices and be dictated by service motives.15
Policy Outcome
UHC should be treated like “one nation, one scheme.”
After implementing UHC, the workload has been mounting on the existing hospital staff in all government hospitals. Hence, empowerment of government hospitals in terms of quality, infrastructure, drugs, and modern facility is the need of the hour for the success of the UHC program.
The disparity in the quality of healthcare services in the public and private sector is continuing and the regulatory standards are neither established nor enforced correctly by the government agencies.
Outpatient visits, which constitute a bigger part of out of pocket expenditure, should be included in Ayushman Bharat.
Prices fixed by the government are far below market rate and it would be unsustainable to operate at such costs while providing high-quality outcomes under UHC. The majority of private hospitals are not showing interest to register under UHC, and they show interest to extend medical treatment only in certain cases. Hence, the government needs to hike the rate, depending on the treatment every year, and should have a realistic pricing mechanism in place.
Since the referral letter is a must from the government hospital to get treatment in a private hospital under Ayushman Bharat–Arogya Karnataka, there is a chance for prevailing more corruption and unnecessary delay. The referral system must be cancelled if possible. Moreover, critical procedures as announced by the government under UHC need to be simplified.
Establishing a well-structured and well-organized referral system in the rural and tribal areas, providing comprehensive services on the concept of primary health is required, so that the burden on secondary and tertiary healthcare may be minimized.
This is the time to focus on time surveillance of “at risk” and “highly vulnerable sections” for various communicable diseases like diabetes, BP, and cancer.
Proposal to outsource monitoring, empanelment, settling of claims, grievance redressal—all vital functions of a UHC—to commercial companies needs a new way out.
Separate institutional mechanism required at the district and state levels to oversee the program, with a new health system approach bringing all stakeholders together.
Need to retain focus on increasing government investment on health, and there is a need to raise new resources including CSR fund to meet the huge cost of UHC.
There must be a special provision for cancer and road accident patents in UHC.
The unifying framework should be provided, so that actions at all levels and by all stakeholders are mutually supportive.
India must invest in addressing inequalities in access to health services and reducing reliance on out-of-pocket (OOP) payments, and action is needed to improve regulatory framework and mediatory mechanisms if it is to achieve UHC by 2030.
Comprehensive improvement in all health system building blocks, such as financing, governance, and human resources, should be planned and operationalized for UHC.
Engage the private sector in the provision of primary care influence of medical audits to improve quality of care, use costing studies to inform evidence-based provider payment policy and data analytics to monitor provider payment systems, and ensure quality of care is need of the hour.
Existing village and health sanitation committees should be transformed into actively participating in health councils. The role ofPanchayat Raj institutions in rural areas and local bodies in urban areas are very vital in this scheme.
Governments and nongovernmental organizations, like health professional associations and national health societies, should be encouraged to contribute to the implementation of the UHC process by integrating risk factor control in their health sector strategies for certain common health issues.
The National Health Regulatory and Development Authority (NHRDA), which regulates and monitors public and private healthcare providers, must be given more powers and autonomy.
(Sources: Proceedings of the National Academy of Medical Sciences Funded National Workshop on UHC held at Mysore University (India) on June 19 and 20, 2019).
Remarks
The unifying framework for the UHC should be provided, so that actions at all levels and by all stakeholders are mutually supportive, Governments and nongovernmental organizations, health professional associations, etc. should be encouraged to contribute to the implementation of the process by integrating risk factor control in their health sector strategies. Multisectoral action is necessary at all stages, because many preventive risk factors lay outside the direct influence of the health sectors. Other departments and agencies whose work touches on preventive care must also be mobilized (e.g., customs and excise, trade and commerce, agriculture, law and justice, labor, transport and public services, education, and the environment).18 The key need of concern in fulfilling the aim of UHC includes a well-structured financing model for quality healthcare delivery; good training for senior health staff in public health institutes; good package and the cost of healthcare interventions; and increasing state budget allocations for public health. While substantial applied research and findings are available today regarding our journey toward UHC, sensible information to address widespread constraints and support the planned policy, decision touching health policies remain an area with incomplete insights. Eventually, India needs sensible solutions to move quantifiable development regarding UHC, and the general population thinks there's no better.16
Future Research—Must Focus On
Reveal the organization, financing, management, and resources to deliver universal healthcare services in India.
Study on health and wellness centers and national health protection schemes under UHC.
Identify the issues and challenges to achieve UHC in the country.
Impact of universal healthcare services on promotive, preventive curative, and rehabilitative health issues, especially for the rural and tribal sections.
Possible drivers of present health inequities within UHC efforts, and possible approaches to shifting the curve toward proequity strategies
Tentative Conclusion
The most common critique against the Ayushman Bharat scheme is that the government is not stressing more on preventive and promotive care. However, the real and tough challenge is how to provide both preventive and curative at the same time. Also, we need to focus on growing catastrophic health expenditure among the poor people. In India, normally, people will give up needy treatment because of the cost factor. People sell their movable and immovable properties just because of medical reasons, putting them into a cycle of poverty. Hence, the experts opine that the state should focus more on curative aspects to minimize the burden on the universal healthcare programs.17 Moreover, it is also very important to bring strong government planning to involve citizens regarding health behavior change through health communication and evidence-based health governance. Introducing prevention-based health checkups in every government health facility is the need of the hour. There is a need for a well-organized referral system in the rural areas, providing complete services and focusing on primary healthcare. A well-structured system for occupational health diseases and the introduction of the concept of occupational healthcare providers is also a must.18 We need quality mass surveillance of “at risk” and “vulnerable populations” for some life-threatening diseases like cancer, heart, hypertension, and diabetes on an urgent basis. More importantly, geographical coverage for endemic diseases are the need of the hour.
Conflict of Interest
None declared.
References
- The World Health Report 1998 Life in the 21st Century: A vision for all. Available at: https://www.who.int/whr/1998/en/. (accessed )
- [Google Scholar]
- Extending health insurance to the poor in India: An impact evaluation of Rashtriya Swasthya Bima Yojana on out of pocket spending for healthcare. Soc Sci Med. 2017;181:83-92.
- [CrossRef] [PubMed] [Google Scholar]
- The introduction of universal access to health care in the oecd: lessons for developing countries. In: S. Nitagyarumphong, A. Mills, eds. Achieving Universal Coverage of Health Care. Bangkok: Ministry of Public Health; 1998. p. :103-124.
- [Google Scholar]
- Creating, reclaiming, defending: non-commercialized alternatives in the health sector in Asia. In: McDonald D, Ruiters G, eds. Alternatives to Privatization: Public Options for Essential Services in the Global South. New York: Routledge Press; 2012. p. :202-204.
- [Google Scholar]
- Universal health coverage in India: Progress achieved & the way forward. Indian J Med Res. 2018;147(04):327-329.
- [CrossRef] [PubMed] [Google Scholar]
- Progress toward universal health coverage: a comparative analysis in 5 South Asian Countries. JAMA Intern Med. 2017;177(09):1297-1305.
- [CrossRef] [PubMed] [Google Scholar]
- Healthcare inequity and physician scarcity: Empowering non-physician healthcare. Econ Polit Wkly. 2013;48(13):112-117.
- [Google Scholar]
- Reflections on and alternatives to WHO's fairness of financial contribution index. Health Econ. 2002;11(02):103-115.
- [CrossRef] [PubMed] [Google Scholar]
- What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet. 2016;388(10044):596-605.
- [CrossRef] [PubMed] [Google Scholar]
- Available at: http://www.cdsco.nic.in/writereaddata/National-Health-Policy .pdf. (accessed )
- [Google Scholar]
- Subodh Sharan Gupta Ayushman Bharat and road to universal health coverage in India. Journal of Mahatma Gandhi Institute of Medical Sciences. 2019;24(02):65-57.
- [CrossRef] [Google Scholar]
- Cabinet Approves Ayushman Bharat-National Health Protection Mission. Available at: http://www.pib.nic.in/newsite/PrintRelease.aspx?relid=177816. (accessed )
- [Google Scholar]
- Does quality of healthcare service determine patient adherence? Evidence from the primary healthcare sector in india. Hosp Top. 2015;93(03):60-68.
- [CrossRef] [PubMed] [Google Scholar]
- Health insurance in India: Rajiv Aarogyasri health insurance scheme in Andhra Pradesh. IOSR Journal of Humanities and Social Science. 2013;8(01):7-14.
- [CrossRef] [Google Scholar]
- ‘Where is the public health sector?’ Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy. 2007;84(2-3):269-276.
- [CrossRef] [PubMed] [Google Scholar]
- The impoverishing effect of healthcare payments in India: new methodology and findings. Econ Polit Wkly. 2010;45(16):65-71.
- [Google Scholar]
- Health insurance in India: prognosis and prospects. Econ Polit Wkly. 2000;35(04):207-217.
- [Google Scholar]
- Universal health insurance in India: ensuring equity, efficiency, and quality. Indian J Community Med. 2012;37(03):142-149.
- [CrossRef] [PubMed] [Google Scholar]





