Translate this page into:
Unmasking molluscum contagiosum: Navigating atypical presentations in a clinical mosaic
*Corresponding author: Dr. Sufian Zaheer, MD, Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. sufianzaheer@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ahuja S, Sharma P, Zaheer S. Unmasking molluscum contagiosum: Navigating atypical presentations in a clinical mosaic. Ann Natl Acad Med Sci (India) 2025;61:31-5. doi: 10.25259/ANAMS_11_2024
Abstract
Molluscum contagiosum is a poxvirus-mediated, highly contagious infection predominantly affecting the face, trunk, and extremities of children and young adults. Although typically characterized by flesh-colored papules with central umbilication, atypical presentations, particularly in immunosuppressed and HIV-infected individuals pose diagnostic challenges. This retrospective study, spanning from January 2013 to January 2016, examined 19 cases of molluscum contagiosum, emphasizing unusual clinical and histopathological features. Three atypical cases were identified, including a 24-year-old female with a subcutaneous lump on the left areola, a 34-year-old male with genital lesions resembling lichen nitidus, and a 17-year-old male with a cystic scalp swelling. Histopathological examination confirmed molluscum contagiosum in all cases, revealing characteristic eosinophilic inclusions within squamous cells. Notably, the study expands the understanding of atypical presentations, such as lesions on the areola and cystic forms, which are infrequently reported in the literature. Despite the absence of immunosuppression or HIV infection in the atypical cases, the study highlights the need for clinicians to consider molluscum contagiosum in diverse clinical scenarios. The accurate diagnosis, often requiring biopsy or cytology, underscores the importance of histopathological evaluation in guiding appropriate treatment strategies, including surgical excision or topical antiviral agents. Overall, these case reports contribute valuable insights into the varied manifestations of molluscum contagiosum, emphasizing the necessity for vigilance in recognizing atypical presentations.
Keywords
Atypical presentation
Histopathological
Inclusions
Molluscum contagiosum
Poxvirus
INTRODUCTION
Molluscum contagiosum is a highly contagious infection caused by the poxvirus that primarily affects children and young adults’ faces, trunks, and extremities. The latter could also exhibit genital involvement as a consequence of intercourse.1,2 Clinical diagnosis of these lesions is aided by typical umbilicated flesh-colored papules and common locations of involvement. Larger versions of these papules have also been documented; however, they most typically measure 3–5 mm.3 But, not every instance exhibits the traditional clinical traits. Not only are unusual places involved. The lesions’ clinical characteristics can also make it difficult for clinicians to make a preoperative diagnosis. These aberrant presentations, which include bigger lesions at odd locations and a peculiar clinical picture, are typical in HIV-positive and immunosuppressed patients.1,4 As per the study conducted by Al-Hilo et al. (2012), a typical presentation of umbilicated papules was found in 92.12% of their study population, while 7.78% patients were clinically atypical.5
Only scattered case reports of unusual presentations of molluscum contagiosum are on record without any large-scale studies. Keeping in view these considerations, we retrospectively reviewed all patients with molluscum contagiosum at our institution with special emphasis on atypical case presentations and morphological features on histopathological and cytopathological evaluation.
CASE REPORTS
The archives of the Department of Histopathology were retrospectively reviewed from January 2013 to January 2016. Of the 45,220 pathology case records reviewed, 19 cases of molluscum contagiosum were retrieved. Of these, unusual sites involved and atypical clinical presentations were included in the study. Following surgical excision, the excised specimen was fixed in 10% neutral-buffered formalin and sent for histopathological evaluation. The diagnosis was confirmed on hematoxylin and eosin (H&E)-stained formalin-fixed paraffin-embedded sections. All the fine needle aspiration cytology (FNAC) smears and histopathology slides were reviewed by two experienced pathologists.
The mean age of the patients was 24.4 years with an age range of 9–54 years. The male-to-female ratio was 2:1. Of these, three atypical cases were observed and included in the study. The clinicopathological features of these cases are described in Table 1. None of these atypical cases showed evidence of immune suppression, and all were negative for HIV testing.
| Cases | Age | Sex | Clinical presentation | Provisional clinical diagnosis | FNAC |
|---|---|---|---|---|---|
| Case 1 | 24 | F | Polypoidal mass on the left breast (areola) measuring 1 cm × 0.8 cm | Fibroepithelial polyp | Not attempted |
| Case 2 | 34 | M | Multiple skin-colored pinpoint to pinhead papules over the shaft of the penis | Lichen nitidus | Features suggestive of molluscum contagiosum |
| Case 3 | 17 | M | Soft to firm swelling on the scalp measuring 4 cm × 3 cm | Sebaceous cyst | Nucleated squamous cells only |
FNAC: Fine needle aspiration cytology
A 24-year-old female, 34-year old male, and 17-year old male presented with unusual clinical characteristics. The first case was a 24-year-old female with a subcutaneous lump in the left areola for 3 weeks [Figure 1a]. The swelling was firm in consistency, measuring 2 cm × 1 cm. A provisional clinical diagnosis of skin appendageal tumor was made.

- (a) Subcutaneous firm lump (black arrow) in the left areola measuring 2 cm × 1 cm. (b) Multiple symptomatic skin-colored pinpoint to pinhead papules (black arrows) present discretely as well as grouped over the shaft of the penis. (c) Young male with a scalp swelling (black arrow) measuring 4 cm × 3 cm. The swelling was cystic with well-defined margins.
The second case was a 34-year-old gentleman with multiple symptomatic skin-colored pinpoint to pinhead papules present discretely as well as grouped over the shaft of the penis for 2 weeks [Figure 1b]. The patient gave a history of unprotected intercourse 4 weeks before presentation. The clinical profile of the patient was suggestive of lichen nitidus. Fine-needle aspiration was performed which revealed whitish material and features suggestive of molluscum contagiosum.
The third atypical case of molluscum contagiosum was in a 17-year-old male who presented with a scalp swelling measuring 4 cm × 3 cm [Figure 1c]. The patient noticed the swelling 1 week prior, and the swelling was increasing in size. On palpation, the swelling was soft to firm in consistency with well-defined margins. FNAC revealed pultaceous material which correlated with the presence of anucleated squamous cells on microscopic examination of smears. No amorphous intracytoplasmic bodies were noted in this case, thus rendering a cytological diagnosis of epidermal inclusion cyst.
Fine-needle aspiration cytology was done in only one case with a provisional diagnosis of sebaceous cyst. The other two cases had a clinical differential diagnosis of a fibroepithelial polyp and lichen nitidus, respectively. Hence, FNAC was not done. Surgical excision of the cases was performed. Histopathological examination revealed skin-covered tissue showing the presence of acanthosis and mild epitheliomatous hyperplasia. There were numerous intracytoplasmic eosinophilic inclusions, molluscum bodies, or Hendersen–Peterson bodies seen within these squamous cells [Figure 2a-2b]. These inclusions showed a change in color from eosinophilic to basophilic at the level of the stratum malpighi. The underlying stroma showed mild lympho-mononuclear inflammatory infiltrate, while a single case of molluscum contagiosum of the breast additionally showed the presence of foreign body giant cell reaction. The atypical case of the scalp and penile swelling also showed similar features; however, the lesion was cystic. This cyst was lined by stratified squamous epithelium with the presence of molluscum bodies [Figure 2c-2d].
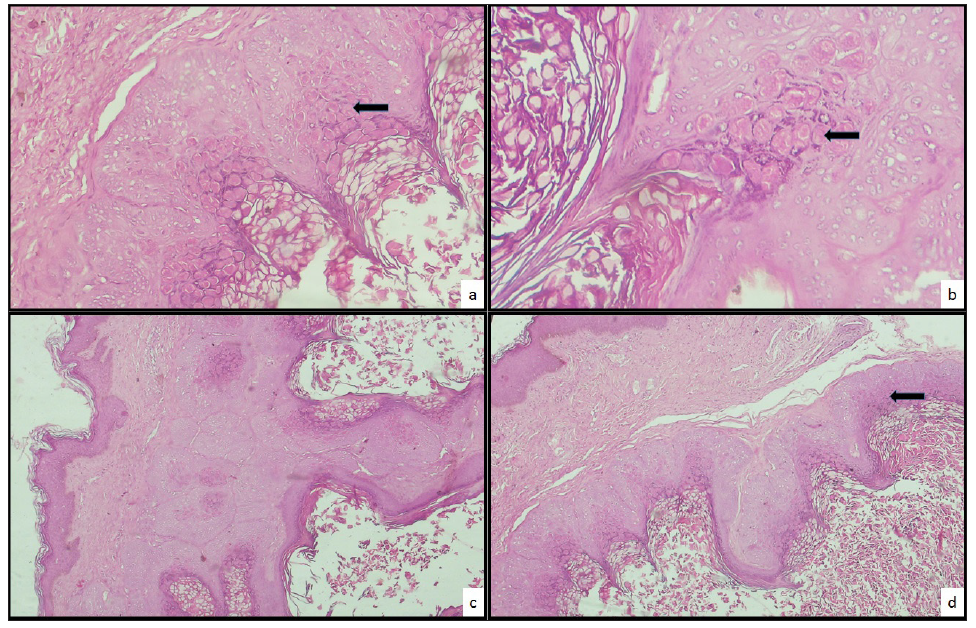
- (a) Photomicrograph showing skin-lined tissue with numerous intracytoplasmic eosinophilic inclusions or molluscum bodies (black arrow) within the squamous cells (H & E; × 200). (b) Higher magnification showing molluscum bodies (black arrow) (H & E; ×400). (c & d) Photomicrograph showing skin-lined tissue with the presence of a cyst lined by stratified squamous epithelium showing intracytoplasmic molluscum bodies (black arrow) (H & E; ×200). H&E: hematoxylin and eosin stain.
The postoperative period was uneventful.
DISCUSSION
The term “molluscum contagiosum infection” was originally used by Bateman in 1817. The disease affects 2%–10% of people globally, with HIV-positive people and other immunocompromised people having an incidence of up to 5%–18%.6 None of the cases in our study showed any evidence of immunosuppression.
The DNA virus that causes molluscum contagiosum infection is a member of the Poxviridae family.7 It comprises four genotypes, of which molluscum contagiosum virus genotype-1 (MCV genotype-1) is the predominant genotype, accounting for 75%–90% of cases in the United States of America, while other genotypes mainly affect the populations in other countries as well as immune-compromised individuals.5,7,8 However, these genotypes are clinically indistinguishable.
MCV is highly contagious, and transmission takes place through direct contact, sexual contact, autoinfection, fomites on towels, salons, and swimming pools. The average incubation period for MCV is 2–7 weeks; however, it can be extended up to 6–18 months. MCV causes epithelial lobules to develop after infecting epidermal keratinocytes. Molluscum bodies are found in these downward-growing lobules of epithelial proliferation. In the event that MCV infection occurs in the hair follicle infundibulum, the patient may occasionally present with comedones or abscesses.
Clinically, immunocompromised people, sexually active adults, and children are often affected by molluscum contagiosum. While childrens trunk, neck, arms, armpits, and faces are most frequently affected, genital lesions are also seen in sexually active adults. It is also frequently noticed that mucous membranes, such as the tongue, lips, and buccal mucosa, are involved. Finally, immunocompromised people can present with atypical appearances such as large forms and disseminated disease. This can also be seen in immunocompetent patients. However, the etiology of the latter remains elusive.9,10
Among the 19 cases of molluscum contagiosum included in our study, we found 3 cases with atypical presentations. Our first case was a 24-year-old female with a molluscum contagiosum lesion over the areola. Firstly, lesions of molluscum contagiosum are small, dome-shaped, skin colored with a characteristic central umbilication. However, in our case, the patient presented with a firm subcutaneous mass misleading the clinician toward a diagnosis of skin appendageal tumor. Secondly, localization of molluscum contagiosum lesions over the nipple and areola is unusual with only eight similar cases reported in the literature [Table 2].1,11-17 The age range of these patients is 18–45 years with 3 cases on the nipple and 5 cases involving the areola. Thus, our case adds to the list of this common lesion at an uncommon site, i.e., areola. It also highlights that an immunocompetent patient can also have atypical presentations of molluscum. Furthermore, this uncommon localization can be confused with other commonly found diseases such as warts, Paget’s disease, and epidermal lesions, thereby making pathological examination a gold standard for diagnosis.
| Case | Age (years) | Site | Clinical features | Treatment |
|---|---|---|---|---|
| Carvalho et al.11 (1974) | 22 | Areola | Initially painless, later infected and painful | Not available |
| Schmid-Wendtner et al.12 (2008) | 20 | Areola | Rapidly growing, raised, yellowish papule | Not available |
| Parlakgumus et al.13 (2009) | Not available | Areola | Pearly popular lesions | 5% imiquimod therapy – 3 times a week for 2 months |
| Kumar et al.1 (2010) | 45 | Areola | Nodular lesions with ulceration | Not available |
| Marwah et al.14 (2012) | 30 | Nipple | Small, papular, nonpainful lesion | Not available |
| Likhar et al.15 (2014) | 18 | Nipple | Papulo-nodular lesion with whitish discharge | Excision |
| Caroppo et al.16 (2016) | 24 | Nipple | Small, flesh-colored, eczema-like plaques | Curettage |
| Hoyt et al.17 (2013) | 28 | Areola | 6 × 6 mm flesh-colored flattened papule | Excision |
| Current case | 24 | Areola | Subcutaneous mass measuring 2 cm × 1cm | Excision |
Another unusual case in our study was cystic molluscum contagiosum, simulating a sebaceous cyst. Molluscum contagiosum presenting as a cystic lesion is an extremely rare entity with only two cases reported in literature to date.5,18 Further borrowing from literature, the coexistence of molluscum contagiosum and epidermal inclusion cyst has also been reported. This rather unusual association can be explained either by co-inoculation of the poxvirus at the time of the cyst formation or invasion of a preexisting cyst by this virus.19
Molluscum contagiosum may simulate many common skin diseases as seen in an isolated case in our study. Although clinical features were suggestive of lichen nitidus, needle extraction revealed the final diagnosis of molluscum contagiosum. Clinical differential diagnoses of molluscum contagiosum include folliculitis, warts, nevi, and skin adnexal tumors such as syringoma and keratoacanthoma.20 However, the exact pathogenesis behind such atypical presentations in immunocompetent patients has not been fully understood.21
Diagnosis is mostly made by clinical evaluation; however, biopsy or cytology is required for a definitive diagnosis, especially in cases of unusual presentations. The lesions are confirmed by the demonstration of molluscum bodies. The latter also known as Henderson–Patterson bodies, are cytoplasmic, faintly granular eosinophilic inclusions that displace nuclei in the cells of the stratum malpighi. At the level of the granular layer, the staining reaction of molluscum bodies changes from eosinophilic to basophilic. Special stains like phosphotungstic acid-hematoxylin and carbon-aniline-fuchsin after mordanting with potassium permanganate are used to demonstrate molluscum bodies.22 The molluscum bodies can also be demonstrated on routine Papanicolau- and Giemsa-stained cytology smears, thus clinching an accurate diagnosis.23,24
Treatment can be in the form of curettage, laser, cryotherapy, or salicylic acid. Solitary intact lesions of molluscum contagiosum in immunocompetent patients can be treated by simple surgical excision. On the contrary, resistant cases in the immunocompromised may be treated with topical antiviral agents like cidofovir or intralesional interferon alpha.25
CONCLUSION
Molluscum contagiosum is a benign self-limiting infection which most frequently involves the trunk, extremities, and genitalia. Unusual sites of involvement along with an aggressive course of disease, although seen more frequently in immunocompromised individuals, can also be encountered in healthy individuals. Thus, the clinicians must keep in mind the differential diagnosis of molluscum contagiosum at rare sites such as areola and even in the setting of skin diseases or cystic lesions.
Authors’ contributions
SA, PS, SZ: Contributed study’s conception and design, material preparation, data collection and analysis; PS, SZ: The first draft of the manuscript was written; SZ, SA, and PS: Commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Cytological diagnosis of molluscum contagiosum with an unusual clinical presentation at an unusual site. J Dermatol Case Rep. 2010;4:63-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Molluscum contagiosum involving an epidermoid cyst: a rare association and potential source of clinical misdiagnosis. J Nepal Med Assoc. 2014;52:723-5.
- [Google Scholar]
- Solitary giant molluscum contagiosum presenting as lid tumor in an immunocompetent child. Indian J Ophthalmol. 2010;58:236-8.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical clinical presentation of molluscum contagiosum in Iraqi patients; clinical descriptive study. Al-Kindy Col Med J. 2012;8:18-27.
- [Google Scholar]
- A novel target and approach for identifying antivirals against molluscum contagiosum virus. antimicrobial agents and chemotherapy. . 2014;58:7383-89.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-53.
- [CrossRef] [PubMed] [Google Scholar]
- Molluscum contagiosum: Its clinical, histopathologic, and immunohistochemical spectrum. Int J Dermatol. 1999;38:664-72.
- [CrossRef] [PubMed] [Google Scholar]
- What is your diagnosis? Giant molluscum contagiosum. Cutis. 2011;88:164;170-2.
- [PubMed] [Google Scholar]
- Successful treatment of molluscum contagiosum in the immunosuppressed adult with topical injection of streptococcal preparation OK-432. J Dermatol.. 1996;23:628-630.
- [CrossRef] [PubMed] [Google Scholar]
- Molluscum contagiosum in a lesion adjacent to the nipple. Report of a case. Acta Cytol. 1974;18:532-534.
- [PubMed] [Google Scholar]
- Flat rapidly growing tumor in a 20-year-old woman. Hautarzt. 2008;59:838-840.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated molluscum contagiosum of nipple: A rare case study. J Evolution Medical Dental Sci. 2014;3:7696-700.
- [CrossRef] [Google Scholar]
- Molluscum contagiosum diagnosis on nipple scraping sample. Breast J. 2016;22:120-1.
- [CrossRef] [PubMed] [Google Scholar]
- Molluscum contagiosum of the areola and nipple: Case report and literature review. Dermatol Online J. 2013;19
- [CrossRef] [Google Scholar]
- Molluscum contagiosum simulating a sebaceous cyst: A rare presentation. Int J Res Dermatology. 2016;2:18-21.
- [CrossRef] [Google Scholar]
- Molluscum contagiosum infestation in an epidermal cyst: still infectious? J Eur Acad Dermatol Venereol. 2010;24:81-3.
- [CrossRef] [PubMed] [Google Scholar]
- The cytology of molluscum contagiosum mimicking skin adnexal tumor. J Cytol. 2010;27:74-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cytologic diagnosis of molluscum contagiosum in scrape samples from facial lesions. Diagnostic Cytopathol. 2003;29:84.
- [CrossRef] [Google Scholar]
- Molluscum contagiosum. A case report with fine needle aspiration cytologic diagnosis and ultrastructural features. Acta Cytol. 2000;44:63-6.
- [CrossRef] [PubMed] [Google Scholar]
- Molluscum contagiosum of the cervix. Diagn Cytopathol. 2012;40:615-16.
- [CrossRef] [PubMed] [Google Scholar]





