Calming the Visual Storm: Management of Childhood Nystagmus
Address for correspondence Pradeep Sharma, MD, FAMS, Pediatric and Neuro-Ophthalmology Services, Centre for Sight, Safdarjung Enclave, New Delhi 110029, India (e-mail: drpsharma57@yahoo.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Childhood nystagmus creates a visual storm both for the affected child and the treating doctor. This problem occurring in the development phase of the child affects not only the vision but also the general development, if not diagnosed and managed in time. Moreover, some forms may even harbor a neurological tumor needing timely management. First, a brief introduction of nystagmus classification, a simplified approach to diagnose the common childhood nystagmus, and the value of electrophysiology will be presented. Next, the approach to treatment, using a thorough clinical examination, illustrated by patient examples of different types of nystagmus will be presented. The different forms of childhood nystagmus are described: idiopathic infantile nystagmus syndrome (IINS), sensory nystagmus (SN), fusion maldevelopment nystagmus (FMDN), spasmus nutans syndrome (SNS), nystagmus blockage syndrome, periodic alternating nystagmus, and others as well as their specific management. The role of electronystagmography and that of neuroimaging in specific conditions is life saving and is described. The role of auditory biofeedback, acupuncture, medical treatment, and surgical procedures like Augmented Anderson procedure, Hertle-Dell'Osso procedure, supra maximal retro-equatorial recession, and posterior fixation have been elucidated. Newer techniques have simplified the management options and improved the functional outcomes in childhood nystagmus. To conclude, children with nystagmus of types IINS, FMDN, SNS, or SN need to be managed differently. It is thus possible to timely manage these children, not only to save their life and improve their vision but also to improve their living quotient.
Keywords
childhood nystagmus
eye muscle surgery
infantile nystagmus
nystagmus
Introduction
The term “nystagmus” is derived from the Greek word “nustagmos” referring to the sleep-induced wobbly head movements, and comprises of regular, rhythmic, and repetitive to-and-fro movements of the eyes. Nystagmus may be divided into physiological and pathological,1 the former comprises of OptoKinetic nystagmus (OKN), vestibular or caloric nystagmus, and endpoint nystagmus. Pathological nystagmus is further subdivided into: (1) sensory nystagmus (SN), the type associated with poor ocular vision due to underlying retinal, optic nerve, or visual pathway defects; (2) acquired neurological nystagmus, which is due to underlying neurological anomalies; and (3) idiopathic infantile nystagmus syndrome (IINS) and other childhood nystagmus detailed below. Then, there are the nystagmoid conditions like convergence retraction nystagmus, Heimann-Bielschowsky phenomenon, ocular bobbing, ocular flutter, and opsoclonus.2
The prevalence of nystagmus, as described by the Leicestershire survey3 is estimated to be 24 in 10,000, of which neurological is 6.8 of 10,000 and sensory 2.4 out of 10,000. In the under 18, it was 16.6 out of 10,000, of which IINS with albinism was the most common variety.
Childhood Nystagmus
The nystagmus types commonly encountered in the early childhood include:
Sensory nystagmus
Idiopathic infantile nystagmus syndrome (INS) or manifest nystagmus
Fusion maldevelopment nystagmus (FMDN) or manifest latent nystagmus (MLN)
Spasmus nutans syndrome (benign and malignant varieties)
Nystagmus blockage syndrome (NBS)
Periodic alternating nystagmus (PAN)
Seesaw nystagmus
These need to be clinically diagnosed and managed differently.
-
Sensory nystagmus: These are typically pendular or pendular-cum-jerk and are associated with poor vision. The term “sensory” is applied to cases that have an inherent anomaly in the visual system as opposed to “motor” but these do not imply a causative mechanism as initially suggested by Cogan.4 The actual neurophysiologic causative mechanism is not known. Ocular examination in detail needs to be done for cataract or any congenital ocular media opacity, aniridia, iridocorneal dysgenesis in the anterior segment, as well as for retinal and optic nerve problems in the posterior segment of the eye (►Table 1). History of diminution of vision, night blindness, or extra sensitivity to light, as seen in achromatopsia, should lead to electroretinography and visually evoked response testing. Early management of bilateral cataract within a month has been seen to help restore vision.5
Brodsky has described four cardinal signs: Severe photophobia, bilateral high myopia, paradoxical pupillary reaction, and ocular digital sign suggestive of poor vision due to congenital retinal dystrophy.6
-
Idiopathic infantile nystagmus syndrome (IINS): This is the most common form of childhood nystagmus (►Fig. 1). It may or may not be associated with albinism. It is characterized by being bilateral, conjugate, uniplanar, mostly horizontal, worsening with fixation, and improving with convergence. Usually it has an eccentric null point leading to abnormal head posture. Oscillopsia is typically absent and two-thirds cases show an inverted OKN response.7
It has been seen to evolve in three phases: a large triangular waveform in the early infancy (►Fig. 2), which converts to a smaller pendular phase 2 at 6 to 8 months and then into a jerk nystagmus in later infancy, and finally settles with a head posture that stabilizes by 3 to 4 years.7
The anomalous head posture should be measured for surgery. This may be mostly horizontal: face turn to right or left but at times it may be vertical; chin up and down or rarely torsional head tilt.
Gelbart and Hoyt8 have emphasized that individuals with IINS have significantly better visual acuities (6/12 to 6/18) than those with primary visual disorders in SN (usually 6/18 or below). This finding implies normal visual sensory systems in these cases allowing better foveation strategies. It also implies that if the vision is poor, one should look for underlying visual system or neurological defect.
Periodic alternating nystagmus (PAN): This infantile PAN variant of IINS should be considered in all cases by looking for the head posture for extended times of about 5 minutes, not to miss them, which may be asymmetric at times.
-
Fusional maldevelopment or manifest latent Nystagmus: 9 It is typically seen to worsen on covering either eye and especially on covering the dominant eye. This is commonly associated with a strabismus or any other ocular anomaly causing fusion maldevelopment. These children have a fast component beating toward the direction of fixing eye alternating with the alternating cover of either eye. Also, they mostly have an adduction null, that is, damping of nystagmus with the dominant eye fixing in adduction. If that eye is covered, the head slowly turns away and the gaze shifted to allow the other eye now fixating in adduction. This is different from the eccentric gaze null in the IINS.
As the nystagmus worsens on covering of one eye, the conventional unilateral vision assessment method yields lesser vision so binocular assessment should be made and uniocular vision reassessed using a plus 4 diopter lens instead of an opaque occluder.
Spasmus nutans: This nystagmus typically presents in infancy as a triad of torticollis, head nodding, and an asymmetric or disconjugate nystagmus. While majority of the cases are benign and spontaneously resolve by 2 to 3 years, 15% cases may harbor an optic nerve pathway glioma and so imaging is mandatory.10,11 In general, any case of nystagmus in childhood that is mono ocular or disconjugate or vertical or accompanied with oscillopsia should definitely be subjected to imaging.
Nystagmus blockage syndrome (NBS): While most nystagmus damps on convergence, NBS is a special form of nystagmus characterized by inverse relationship between esotropia and nystagmus as described by Adelstein and Cuppers. These cases typically show nystagmus with orthotropia and no nystagmus with esotropia.12 Medial rectus (MR) posterior fixation in cases of straight eyes in rest position or with recession in case of esotropia is indicated.13
Seesaw nystagmus: It is an uncommon form of pendular nystagmus characterized by simultaneous elevation and intorsion of one eye, with depression and extorsion of the other eye, and reversal in a cycle. Seesaw nystagmus usually occurs in patients with large suprasellar tumors involving the optic chiasm and extending into the third ventricle. These children usually have a bitemporal hemianopia.14
| 1. Congenital cataract 2. Congenital glaucoma 3. Aniridia 4. Iridocorneal dysgenesis 5. Leber congenital amaurosis 6. Retinoblastoma 7. Retinal dysplasia 8. Ocular coloboma 9. Congenital stationary night blindness 10. Congenital retinoschisis 11. Achromatopsia 12. Ocular albinism with foveal hypoplasia 13. Optic nerve hypoplasia 14. Cicatricial retinopathy of prematurity |

- A child with oculocutaneous albinism having nystagmus with left face turn.

- An infant having the initial triangular waveform phase of infantile nystagmus syndrome.
“Neurological” Nystagmus
Though all nystagmus are inherently neurological, this term may include conditions with overt neurological problems, like: Leigh disease, Pelizaeus-Merzbacher disease, Joubert syndrome, infantile neuroaxonal dystrophy, hypothyroidism, Maple syrup urine disease, Down syndrome, and nutritional nystagmus.6
Nystagmoid Movements
These are irregular nonrhythmic movements that may appear like nystagmus: for example, convergence retraction “nystagmus,” Heimann-Bielschowsky phenomenon, ocular flutter, opsoclonus, and ocular bobbing. Also, some people may have ability to do voluntary nystagmus.6
Electronystagmography
The recording of the nystagmus by using electrodes at the lateral and medial canthi with a neutral at the forehead is used for horizontal nystagmus. Similarly, videonystamography can be done. A typical preoperative and postoperative recording of a case of IINS is shown in ►Fig. 3. It shows that the nystagmus is present in the primary position and worsens in 15- and 30-degree levoversions, but damps in 30-degree dextroversion, which is the null point. This corresponds with the 30-degree left face turn. Surgery is done by Augmented Anderson procedure and postoperatively the nystagmus damps in the primary position, 15- and 30-degree dextroversions. This leads to correcting the abnormal head posture. The intensity of nystagmus is a multiple of amplitude times frequency, and the amplitude and not the frequency is appreciated clinically better. Foveation time is the primary indicator of visual function, while amplitude and frequency are secondary measures that may not tally with visual acuity. Thus, patients with a high-frequency nystagmus may have better visual acuity than others with low-frequency infantile nystagmus, simply because they have more total foveation time. Dell'Osso et al have developed a nystagmus acuity function that depends solely on foveation quality with the primary emphasis on foveation time.15,16 The ENG in an IINS is characterized by a period of foveation followed by an increasing-velocity slip away from the target and, finally, a corrective saccade back toward the target, resulting in a typical accelerating slow phase as compared to the decelerating slow phase in FMDN or MLN.16
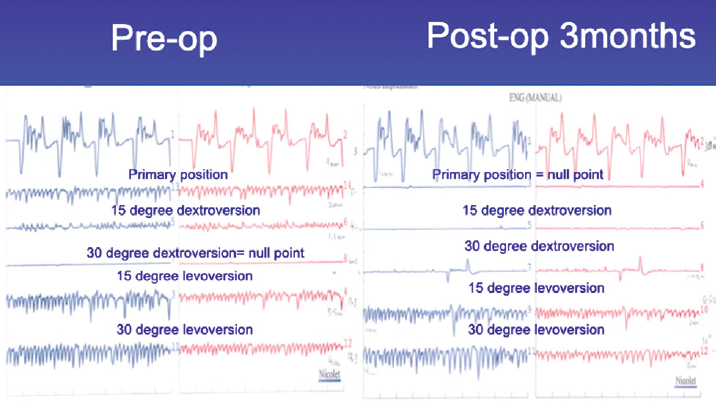
- The nystagmus is present in the primary position and worsens in 15- and 30-degree levoversions, but damps in 30-degree dextroversion, which is the null point. This corresponds with the 30-degree left face turn. Surgery is done by Augmented Anderson procedure and postoperatively the nystagmus damps in the primary position, 15- and 30-degree dextroversions.
Imaging in Nystagmus
Generally, imaging is not indicated in cases of nystagmus except for the following situations:6
In infants with infantile nystagmus with optic nerve hypoplasia, where magnetic resonance imaging (MRI) is indicated to evaluate the structural status of the pituitary infundibulum, cerebral hemispheres, and midline intracranial structures (septum pellucidum, corpus callosum). The nystagmus is sensory in nature due to optic nerve hypoplasia, and the purpose of neuroimaging is to search for associated central nervous system anomalies that commonly coexist with optic nerve hypoplasia.
MRI is indicated in infantile nystagmus and optic atrophy to rule out a congenital suprasellar tumor (e.g., chiasmal glioma, craniopharyngioma) or hydrocephalus.
MRI is indicated in children in whom the diagnosis of infantile nystagmus is uncertain and the possibility of spasmus nutans exists to rule out chiasmal gliomas or other suprasellar tumors.
Imaging is also indicated in infantile nystagmus accompanied by seesaw nystagmus, to evaluate for achiasmia.
Nonsurgical Management
In general, a good ophthalmic work-up and specific tests described above for specific types of nystagmus should be performed for optimal prescription of glasses to help improve vision and control nystagmus. Nystagmus with associated albinism is helped by photochromatic glasses. Persons with high myopia or high hyperopia may be given contact lenses but that does not damp the nystagmus.
Use of base out prisms to induce convergence has been found to be a helpful strategy. Use of auditory biofeedback by converting the ENG recording into an auditory biofeedback beeping signal has a transient damping effect lasting only during the duration of the treatment.17
Acupuncture has been studied in few cases where 0.2 mm needles have been used in the sternocleidomastoid acupoints and ENG recorded. The ENG showed a damping effect at the introduction of the needles and also while twirling of these every 5 minutes but the nystagmus returns back in the intervening periods. There was no lasting effect of the treatment.18
Medical treatment: Few pharmacological drugs have been found to be useful in the management of childhood nystagmus:
Medical treatment for acquired nystagmus has been through augmenting the inhibitory neurotransmitter system (e.g., gamma-amino-butyric acid [GABA]) or inhibiting the excitatory neurotransmitter system (e.g., glutamate).19,20 Downbeat nystagmus has been treated successfully with clonazepam (a GABA-ergic inhibitor). Gabapentin and memantine use have also been described by Shery et al.21 Gabapentin has also been seen to reduce Heimann-Bielschowsky phenomenon.22
Baclofen (an inhibitor of glutamate release) though useful in acquired PAN due to head injury or neurological insults has not been found to be effective in congenital PAN.7
Brinzolamide eye drops have been used with limited success in cases with no definite null position.23
However, the medical treatment is not cost effective and in the long run the results of the surgical treatment outshine the results of medical treatment.
Surgical Management
Strategies for surgical management include (►Table 2):1
| 1. Shifting the eccentric null position: Anderson–Kestenbaum procedure A. Anderson: yoke muscle recession B. Goto: yoke muscle resection C. Kestenbaum four-muscle recession resection (all muscles 5 mm) D. Parks: classic medial rectus (MR) recession/resection: 5, 6; lateral rectus (LR) recession/resection: 7, 8 E. Augmented Parks: 1: classic + 40% for 30 degrees F.2: classic + 60% for 45 degrees G. RPC: MR recession/resection: 6, 6; LR recession/resection: 9, 9 H. Augmented Anderson for 30 degrees: MR recession 9 mm, LR recession 12 mm I. Augmented Anderson for 45 degrees: MR recession 9 mm, LR recession 12 mm, plus opposite MR 6 mm and LR 9 mm resections 2. Artificial divergence: bilateral MR recession/± posterior fixation 3. Correcting associated strabismus for eso- or exotropia 4. Four horizontal muscle recession: supramaximal recessions 5. Hertle-Dell'Osso procedure: disinsertion and reinsertions without recession or resection |
Shifting the eccentric null position: horizontal/vertical/oblique
Artificial divergence: MR recession/posterior fixation
Correcting associated strabismus
Four horizontal muscle recession
Hertle-Dell'Osso procedure
Anderson–Kestenbaum (AK) Group of Procedures
For shifting the eccentric gaze null to the primary position (►Fig. 4), several procedures have been described; starting with Anderson, Kestenbaum, and Goto in the early fifties, and then their modifications from time to time:1

- Schematic drawing showing the shifting of eccentric gaze null in dextroversion corrected by yoke muscle surgery.
Anderson: yoke muscle recession
Goto: yoke muscle resection
Kestenbaum: four horizontal recti muscle-recession resection (all muscles 5 mm)
Parks: classic MR recession/resection: 5, 6; lateral rectus (LR) recession/resection: 7, 8
Augmented Parks: (1) classic + 40% for 30 degrees; (2) classic + 60% for 45 degrees
Modified Kestenbaum: MR recession/resection: 6, 6; LR recession/resection: 9, 9
Augmented Anderson: MR recession 9, LR recession 12
Our preference is for the Augmented Anderson procedure in which the yoke muscle recessions are done by augmented amounts of 9 mm for MR and 12 mm for LR to correct a head turn of 30 degrees. The pre- and postoperative face turns are shown in ►Fig. 5. In an earlier study,24 we demonstrated good results with this approach. The advantage apart from getting reasonable success with tackling two muscles is also that in case of a missed PAN the Augmented Anderson procedure can be done on the other two recti, without having to undo the resections as would have to be done if Kestenbaum procedure would have been done. For more than 40 degrees, the opposite recti are resected by 6 mm and 9 mm for MR and LR, respectively.

- The pre- and postoperative picture showing the right face turn in preoperative picture is corrected postoperatively.
For vertical head postures, chin up and down: on a similar principle as AK procedures, bilateral superior rectus recessions (with inferior rectus [IR] resections for over 20 degrees) for chin up and similarly IR recessions for chin down postures is done. And on the same principle for head tilts, the horizontal shifting of vertical recti, vertical shifting of horizontal recti, and advancement and recessions of anterior halves of the respective oblique muscles have been described for correcting it.
Cases having associated strabismus are tackled to correct both, the nystagmus, by operating on the dominant eye muscles only, and the strabismus, which can be managed by operating on either eye.
Artificial divergence surgery
The second strategy is to induce artificial divergence as suggested by Cuppers to excite convergence to damp the nystagmus by doing MR recession or posterior fixation procedures on the MRs. However, this may be suitable only in cases with good fusional vergences, else will create unfusable diplopia.
Correcting associated strabismus
This is the strategy for the associated strabismus in cases of FMDN or MLN. For cases like Ciancia syndrome, the MR recessions are done along with posterior fixation sutures to correct the adduction null. Similar strategy is for the NBS cases.
Four horizontal muscle recession
This is the strategy for the congenital PAN cases. This is also done for cases with no eccentric null to cause some dampening of nystagmus, as described by Bietii and Bagolini. Such patients would use active blockage of nystagmus associated with increased innervational effort (similar to that seen with active convergence) to damp their nystagmus.25,26
Hertle-Dell'Osso procedure
This is another surgery described whereas the four horizontal recti are disinserted and reinserted at their insertion points without any recession or resection on the premise of altering the feedback loop of the tendon receptors.
In a comparative prospective pilot study done by the author's team, it was observed that both the above procedures did damp the nystagmus for a few months and improved the vision subjectively but were not having a lasting effect.27
Cases with associated strabismus have to be tackled taking the deviation into account. The nystagmus surgery needs to be done on the dominant eye and the preexistent deviation or the deviation created by nystagmus surgery has to be tackled by the other eye muscles' surgery.1,28 Cases with no definite null have been a difficult challenge to handle. Auditory biofeedback, acupuncture, four-muscle supramaximal recession, or Hertle-Dell'Osso procedure have been done but to not much advantage in the long run. In the search of a remedy even drastic measures like total myectomy of all horizontal recti muscles using a snare have been suggested by Sinskey and its modifications have been reported by other workers,29 but these have more complications and may not be recommended.
To Conclude: Take-Home Points
Imaging to rule out underlying neurological conditions is recommended in all cases of: spasmus nutans, vertical nystagmus, seesaw nystagmus, all acquired cases, and any case with oscillopsia.
Optimal optical correction with glasses is recommended and for albinism photochromatic glasses are useful. Contact lenses may be helpful for high refractive errors.
Cases with definite eccentric gaze null up to 30 degrees respond very well to Augmented Anderson procedure.
For more than 40 degrees, resections of the opposing yoke muscles are added to increase the null shifting effect.
Cases with PAN: bilateral Augmented Anderson procedure is recommended.
Cases with FMDN with squint: correct the squint; this makes the manifest nystagmus latent.
Infantile esotropia with nystagmus in abduction (Ciancia syndrome), NBS: MR recession with posterior fixation suture.
Cases with adduction null, convergence dampening: posterior fixation on medial recti.
Cases with no definite null: auditory biofeedback, acupuncture, four-muscle supramaximal recession, or Hertle-Dell'Osso procedure may be done. These seem to work for some time only.
Medical treatments like brinzolamide eye drops or oral gabapentin, memantine, or baclofen have limited role.
Conflict of Interest
None declared.
References
- A National Eye Institute Sponsored Workshop and Publication on The Classification of Eye Movement Abnormalities and Strabismus (CEMAS) The National Eye Institute Publications at: www.nei.nih.gov/news/statements/cemas.pdf (accessed )
- [Google Scholar]
- The prevalence of nystagmus: the Leicestershire nystagmus survey. Invest Ophthalmol Vis Sci. 2009;50(11):5201-5206.
- [CrossRef] [PubMed] [Google Scholar]
- “Sensory” and “motor” nystagmus: erroneous and misleading terminology based on misinterpretation of David Cogan's observations. Arch Ophthalmol. 2007;125(11):1559-1561.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in nystagmus after simultaneous surgery for bilateral congenital cataracts. Jpn J Ophthalmol. 1993;37(03):330-338.
- [Google Scholar]
- Idiopathic infantile nystagmus diagnosis and treatment: Costenbader lecture. J AAPOS. 1997;1:67-82.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital nystagmus: a clinical perspective in infancy. Graefes Arch Clin Exp Ophthalmol. 1988;226(02):178-180.
- [CrossRef] [PubMed] [Google Scholar]
- The neural mechanism for latent (fusion maldevelopment) nystagmus. J Neuroophthalmol. 2010;30(03):276-283.
- [CrossRef] [PubMed] [Google Scholar]
- Spasmus nutans. A quantitative prospective study. Arch Ophthalmol. 1987;105(04):525-528.
- [CrossRef] [PubMed] [Google Scholar]
- Head nodding is compensatory in spasmus nutans. Ophthalmology. 1992;99(07):1024-1031.
- [CrossRef] [PubMed] [Google Scholar]
- The nystagmus blockage syndrome. Congenital nystagmus, manifest latent nystagmus, or both? Invest Ophthalmol Vis Sci. 1983;24(12):1580-1587.
- [Google Scholar]
- Surgical results in nystagmus blockage syndrome. Ophthalmology. 1986;93(08):1028-1031.
- [CrossRef] [PubMed] [Google Scholar]
- An expanded nystagmus acuity function: intra- and intersubject prediction of best-corrected visual acuity. Doc Ophthalmol. 2002;104(03):249-276.
- [Google Scholar]
- Congenital nystagmus waveforms and foveation strategy. Doc Ophthalmol. 1975;39(01):155-182.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of congenital nystagmus amplitude with auditory biofeedback. J AAPOS. 2000;4(05):287-290.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of acupuncture on waveform characteristics and visual acuity in idiopathic infantile nystagmus: a prospective interventional study. J Clin Diagn Res. 2022;16(05):NC05-NC08.
- [Google Scholar]
- Medical treatment of nystagmus and ocular motor disorders. In: Beck RW, Smith CH. eds. Neuro-ophthalmology. Boston: Little-Brown; 1986:251-264.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of gabapentin and memantine in acquired and congenital nystagmus: a retrospective study. Br J Ophthalmol. 2006;90(07):839-843.
- [CrossRef] [PubMed] [Google Scholar]
- Oral gabapentin treatment for symptomatic Heimann-Bielschowsky phenomenon. Am J Ophthalmol. 2006;141(01):221-222.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of topical brinzolamide on infantile nystagmus syndrome waveforms: eyedrops for nystagmus. J Neuroophthalmol. 2011;31(03):228-233.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective clinical evaluation of augmented Anderson procedure for idiopathic infantile nystagmus. J AAPOS. 2006;10(04):312-317.
- [CrossRef] [PubMed] [Google Scholar]
- Active blockage and rest position nystagmus: electromyographic demonstration of two types of ocular induced head-turn. Doc Ophthalmol. 1986;62(02):149-159.
- [CrossRef] [PubMed] [Google Scholar]
- Benefits of retroequatorial four horizontal muscle recession surgery in congenital idiopathic nystagmus in adults. J AAPOS. 2006;10(05):404-408.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective evaluation of retroequatorial recession of horizontal rectus muscles and Hertle-Dell'Osso tenotomy procedure in patients with infantile nystagmus with no definite null position. J AAPOS. 2016;20(02):96-99.
- [CrossRef] [PubMed] [Google Scholar]
- Oculographic and clinical characterization of thirty-seven children with anomalous head postures, nystagmus, and strabismus: the basis of a clinical algorithm. J AAPOS. 2000;4(01):25-32.
- [CrossRef] [PubMed] [Google Scholar]
- Myectomy of the extraocular muscles without reattachment as a surgical treatment for horizontal nystagmus. J Pediatr Ophthalmol Strabismus. 2016;53(03):156-166.
- [CrossRef] [PubMed] [Google Scholar]





