Translate this page into:
NAMS task force report on gunshot and blast injuries
*Corresponding author: Dr. Tanmoy Roy, Senior Consultant (Surgery), Armed Forces Medical Services, India. poonam_troy@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Roy T, NAMS task force report on gunshot and blast injuries. Ann Natl Acad Med Sci (India) 2024;60:299-323. doi: 10.25259/ANAMS_TFR_09_2024
INTRODUCTION
War, conflict, crime, and accidents have been omnipresent since the origin of humankind. All diseases may be conquered, but conflict, trauma, and war will remain. This is because neither the desire for dominance, supremacy, and control over resources will ever end, nor will the unexpected ever stop happening. However, the intense nature and severity of injuries due to gunshot wound (GSW), missiles, and explosives are progressively on the rise on account of the easy availability of firearms, a dramatic shift like warfare, changes in societal behavior as well as the demographic changes occurring in the world. Incidences of wounding, mutilations, and disruption of body parts on account of GSW, missile, and blast injuries (BI) are increasing progressively all over the world, and India cannot remain untouched. Hence, it is time to address the issue substantively before it is too late.
BACKGROUND
The use of higher-order explosives and indigenous ways of weapon delivery has resulted in unusual and unconventional forms of injuries both in military and civil life. Hence, India needs a comprehensive policy to address the complex issues related to firearms injuries and those due to explosions. This is so that the military/paramilitary/ police and other members of the security establishments, as well as the civilian population caught in the crime scene/in the crossfire, who are usually unintended victims of collateral damage, are managed comprehensively and as medical, legal and criminal dimensions of the issue addressed.
The more common wounding agents in modern warfare are artillery, missiles, and bombs, and not GSW, whereas, in terrorist operations, it is the GSW injuries that predominate. In suicide attacks, it is an improvised explosive device that is the most commonly used agent. Hence, the pre-hospital care for the victims must be standardized and incorporated as part of the country’s medical/ paramedical/ nursing courses.
The echelons of care, the objectives and standard of initial care, measures to minimize blood loss and maintain oxygenation, the concept of the primary survey, secondary survey, and triage, followed by treatment, the standard of documentation, in maintaining clarity, brevity and consistency with a uniform protocol, needs to be implemented all over the country. If everybody can speak and interpret all relevant matters and communicate amongst the stakeholders along the same lines, it will eliminate the communication gap to a large extent. Similarly, the medico-legal aspect relevant to the problem has been addressed holistically in the white paper. This white paper will lead to a comprehensive understanding of the problem from the point of view of policy formulation and its implementation in India.
TERMS OF REFERENCE
To identify the current status of gunshot & BI.
Identify the deficiencies which need to be addressed.
To recommend measures for the management of gunshot & BI.
METHODOLOGY ADOPTED
The study was commissioned as a joint study by NAMS and the Armed Forces. The study findings are based on an extensive review of the literature using the databases of Pub Med, Cochrane Library, Google Scholar, various books, journals, and publications, as well as inputs from the manuals used by the Armed Forces. The fields chosen were title, keywords, abstracts, and MeSH (Medical Subject Headings). Extensive discussions and deliberations by team members and the various experts on the subject matter, both in person and in electronic mode, followed. Extensive inputs based on the experiences of various domain experts were used in critical analysis of the matter. The content and context were analyzed in as much detail as possible, and the inferences obtained were relevant to the current Indian scenario and its projection in the next 10 years. At that time, India is expected to become a recognized world power.
DETAILED STUDY OF THE SUBJECT MATTER
The matter is discussed under the following lines.
What is the realistic achievement in matters related to managing gunshot and BI that we should aim for the citizens of India in the next 10 years?
What is the current reality regarding our ability to manage gunshot and BI in India as a country, and how to address the gap in capabilities?
What measures are necessary for the management of gunshot & BI?
DESIRABLE OBJECTIVES FOR THE NEXT TEN YEARS
In the next 10 years, India as a whole should be able to become a country where citizens in any part of India should be able to avail facilities of high-quality trauma care, including care for bullet injuries and explosive-induced BI. The aim is to save a maximum number of lives, reduce disability amongst our compatriots, and properly rehabilitate victims so they can remain productive members of society and contribute to the national economy. This, if achieved, will become a symbol of the largest social security cover in the world where no family will go on to face poverty due to the loss of its bread earner.
To achieve this, all citizens must know enough about the actions to avoid injuries, reduce their impact on occurrence by taking simple measures, access immediate emergency care, and benefit from universal coverage.
To enable this to happen, the following should be aimed for
All citizens must be equipped with two specific abilities: how to stop bleeding and how to give cardiopulmonary resuscitation at the point of injury.
Ambulances with medics/paramedics should be able to reach the injured as fast as possible within the golden hour. Alternately, the victim should also be able to reach the nearest trauma care facilities, preferably once the emergency caregiver has controlled his/her bleeding and breathing using the fastest means.
Once the victim reaches the hospital, he should be attended to immediately by the attending doctor and his/her team without any reservation (without financial or legal hurdles). The hospitals should be protected from financial burdens by providing prompt reimbursement for the treatment.
A collective national effort, planned but time-bound at all levels, must improve the medical fraternity’s and common citizens’ abilities to manage GSW and BI.
The national trauma registry and archiving system, as well as all details regarding gunshot and BI available at the hospital, mortuary, forensic labs, cremation ground, cemeteries, police, etc., should be digitized, networked, and AI-enabled to generate a realistic database so that one can look for patterns and improve outcomes by suggesting action points.
The financial support to all hospitals should be based on a computer-based, server-secured, and AI-enabled network and from a deliberately and consciously developed national corpus, preferably the consolidated fund of India. It is suggested that all transactions in digital format in the country be charged @ 0.01% as ¯trauma care cess, from which the reimbursement to all the echelons giving robust trauma care is provided quickly. The absence of financial support to the hospital, most of which is in a private set-up, combined with the inability of the unknown’ victim to be in a position to pay until one of his family members could commit to the expected expenditure, is the universal impediment to good trauma care in India and this truth needs to be accepted as we move on as an emerging nation. This needs to change in favor of honest taxpaying citizens who should be automatically insured for treatment and below poverty line (BPL) families who should be covered under the Ayushman Bharat scheme.
THE CURRENT STATUS OF GSW AND BIs - ACTIONS WHICH ARE REQUIRED TO BE TAKEN
Current situation in the country
GSW and BI are steadily developing into a significant public health problem in India and seem to be following the trends seen in Western nations. This is consistent with the increasing prevalence of firearms and explosives (industrial as well as illegal) in both villages and the cities of India.1,2
The exact incidence of gunshot injuries in India cannot be ascertained due to a lack of reliable data, with only a few reliable studies being available from the Armed Forces and civil stream in India, which provide some insight into the nature of injuries and outcome.2
A study from Mumbai reflecting an urban setting found that the injured victim was rescued by a passerby in 43.5% of cases and helped by the police in 89.7% of instances, with the victim in most cases being transported by a taxi or a private car to a hospital without provision of any emergency medical aid on the site of injury. The ambulance was put to use only in 39.3% of cases. This constitutes a very significant limitation in the successful primary management of firearm injuries.3
Effectiveness of ambulance services
The Emergency Medical Service (EMS) in rural India is rudimentary despite significant leaps in this field in large metros and capital cities, with the second-tier cities fast catching up with the gradual development of robust emergency ambulance services. However, ambulance services usually take patients to a hospital based on the likely affordability of the patient based on first impression. In other words, a trauma victim with doubtful financial viability is usually directly taken by Ambulance services to the Accident & Emergency of a nearby tertiary care super specialty hospital (most are private entities) only when his life is under imminent threat when he usually gets attended with the immediate interventions required to save his life. However, once he is identified as constituting a financial burden, the victim is often transferred out to one of the second-rung nursing homes on the first available opportunity, usually to the detriment of his safety and health. The government needs to come up with a clear policy on financial compensation for all trauma victims. This is because this group constitutes the largest share of preventable deaths all over the world and occurs usually in a young earning population out on the road for work or leisure, and contributes to the nation’s economy. Unless this issue is addressed, victims of salvageable critical gunshot injuries in civilian life will, by and large, continue to become disabled or lose life.
Most state governments and municipalities in the last ten years have made substantial progress in developing their Ambulance services, e.g., 108 Ambulance’ which are integrated with call centers and work 24 x 7 x 365 days, and this service is slowly progressing towards even tier 2 towns, which is very encouraging. However, as a nation, we have a long way to go to make these ambulances capable of handling blast and gunshot injuries. As of now, these ambulances can only give oxygen and fluids, and although they have facilities to provide cardiopulmonary resuscitation (CPR) they are not fully geared up to treat GSW/BI. Thus, the lack of optimal ambulance/transport services constitutes an important limitation in handling GSW/BI, and the matter is deliberated below.
Gaps in ambulance services
It is a hurdle in India that needs an urgent solution. Many organizations, including the government, manage Ambulance Services and are supported and facilitated by police, fire brigades, hospitals, and private agencies. The controlling agencies and telephone numbers vary from state to state. This needs to become unitary, learned, and memorized by children from primary school across the country. GSW/BI requires specialized care when being evacuated. However, in a study, only 30 ambulances out of 94 could partially cater for the provision of ATLS. Another important component in the care of these sick patients is a protocol- based on treatment, but only 20% of district hospitals were found to have a documented emergency manual, with only 8% of district hospitals having documented policies and procedures for patient transfer.4
Ambulance staffing
Most privately managed ambulances lack an adequately trained workforce. Many are contractual staff on short stop-gap contracts, which is due to the absence of any clear regulation regarding the minimum qualification/ experience required to man an ambulance and the lack of regulations on the minimum number of professionals required for manning an ambulance service (medics/paramedics/telephone attendant/on-call roster, etc.). In the suburbs and hinterland, the situation is even more acute.5
Lack of adequate equipment in ambulances
Most ambulances are inadequately equipped and ineffective in providing life-saving trauma care interventions during transport.6 The impression that stretchers, oxygen, saline, and bandages are enough to run an ambulance service needs to be dispelled.
Misuse of ambulances
Many studies have reported misuse of ambulances. Another glaring fact is that a large majority of ambulances have been found to transport the dead sometimes or other, either due to an absence of hearse vans or organizational pressure, thus making them not available for a medical emergency should a situation arise. This should be made a punishable offense.
Lack of coordination between the ambulance services and nearby health facility
The impending arrival of patients transported to the nearest health facility is usually not communicated to the receiver due to inadequate communication systems and a lack of knowledge amongst bystanders regarding where to take the victim. Private ambulances constitute the majority share. Air ambulances are operational only in certain large cities, but affordability is a big drawback. Hovercrafts as ambulances in coastal areas are still in their infancy in India but are expected to be leveraged widely in the next decade. Transfer of patients by helicopter is picking up in rugged terrain, and that by drone is on the anvil as the load-carrying capacities of indigenous drones are now more than 80 kg. Hence, drones, as a viable means of patient transfer, especially of injuries by bullets/explosives, are likely to see the light of day as a mainstay in the next 5 years.
PRIMARY CARE
a) Role of primary care physician
Ideally, the primary care physician should become the sheet anchor in initiating the management of firearm-induced body disruption and massive blood loss once the first responder has brought the victim to the primary care facility since the fate of the victim is generally decided in the next 30-60 minutes.7 However, in India, the ability of a primary care physician to independently impart trauma care is often suboptimal, primarily due to inadequate attention given to training on aspects of trauma care during Bachelor of Medicine and Bachelor of Surgery (MBBS) and rotating internship training, due to which, although the doctor is reasonably equipped with the theoretical knowledge, he is unable to put the knowledge into practice.8-10 This severe limitation in skill level must be addressed by mandatory exposure to lifesaving measures in the ATLS trauma certification program as part of internship training before being granted an MBBS degree by the university or being registered for medical practice in the country by the National Medical Council (RMP status) and revalidation of the presence of this essential ability every five years.
b) Role of paramedics
A competent paramedic helping a casualty doctor meaningfully makes the job of a doctor so much easier. However, in India, paramedics are imparted a fundamental knowledge of trauma care but practically have no experience of it. This is a paradox since they usually are the first responders. However, they learned many aspects of it if they started working in a field related to trauma/emergency care, which is not common. Since paramedics are now attaining specialization directly after leaving school, e.g., in pharmacy, X-ray, health, recordkeeping, skin diseases, psychiatry, nursing, etc., directly without at any stage working in an emergency or a patient ward, they do not learn to handle a sick patient in a ward at all. Hence, the availability of paramedics who could handle the basic emergency requirements of bullet injury has dwindled further. Therefore, training in BLS and Basic Trauma Life Support (BTLS) courses should be made mandatory as part of the degree and diploma for nurses and paramedics.
c) Role of the common man
The common man is, by and large, unaware of the basics of trauma management and usually is not in a position to help his fellow citizens who have sustained GSW and BI and are in distress. This is unfortunately aggravated by a sense of apathy more visible in roadside injuries, especially roadside crimes, since victims are unknown, and fear of the consequences of getting involved overwhelms the sense of reason and brotherhood. The citizens have to be taught through various awareness programs to be more responsible for their helpless brothers and sisters in distress, and any disregard for reasonable help should be made punishable and implemented by the withdrawal of social benefits. Social scientists, anthropologists, and non government organizations (NGOs) need to help the government in this effort in a substantive way so that citizens become more responsible. The current approach taken by society, the medical fraternity, and the Government toward the problem of treating GSW and explosive BI need to change.
PARTS OF THE BODY DISRUPTED IN A BLAST INJURY
Bullet injuries form a subset of trauma care. It can affect any part/organ of the body from scalp to great toe, i.e. skull and brain, face (maxilla, orbital structures, naso-ethmoid, mandible, dental elements), neck (cervical spine, major vessels, pharynx, esophagus, trachea), chest (heart, lung, aorta, inferior vena cava (IVC), spine and spinal nerves), abdomen (gut, solid organs, vessels and spine/spinal nerves, retro- peritoneum), pelvis (gut, urinary bladder, uterus, prostate, pelvic bones, head and neck of femur), limbs (brachial plexus, vessels, muscles, tendons, bones, joints). Very few doctors can handle all regions of the body competently. The reason is the trade-off, i.e., compartmentalization of the sphere of general competence in the endeavor to achieve a very high level of special competence in particular aspects of a body. This is explained below.
LIMITATIONS IN COMPREHENSIVE TRAUMA CARE DUE TO SUPER SPECIALIZATION
Surgical super-specialty training is primarily organ/tissue-specific, e.g., neurosurgeons & neurophysician treating nerve and brain derangements, urologist & nephrologist treating kidney diseases, medical & surgical gastroenterologist treating gut, liver, and pancreas, cardiologists & cardiac surgeons treating heart, endocrinologists and endocrine surgeons treat gland disorders, ear, nose, and throat (ENT) specialists treat Ear, nose, and throat, eye specialists are limited to eyes, gynecologists to the uterus, cervix and ovaries and so on.11 By their inherent nature, some super specialty is required to explore all types of anatomical areas, e.g., vascular surgeons, surgical & medical oncologists, plastic surgeons, and trauma surgeons. They can handle problems in multiple areas better but still have limitations.12 Thus, the arrivals of so many super-specialties have no doubt enabled advanced Medicare but have robbed the general specialists of the opportunities to explore multiple fields of the body and acquire the confidence to handle difficult situations. On the other hand, super-specialists abilities have touched an extraordinary level of excellence compared to the best in the world in handling body parts in their core areas. However, making ATLS certification mandatory, along with the requirement of compulsory work in a recognized trauma center for 5 days every 2 years for all if made mandatory to maintain their license to practice, will increase the talented and accomplished pool of doctors in trauma care, which will be good for the nation in the long term in both war and peace.
IMPACT OF CONSUMER MOVEMENT ON TRAUMA CARE
Pressure by family members of trauma victims to be seen only by a super-specialist once the victim reaches the emergency department combined with misplaced consumer activism, interventions by consumer court, and the consequent fear of prolonged litigation have no doubt taken its toll. Nobody attempting to save a life with an honest effort would like to be labeled as incompetent due to limited available equipment or staff and another organizational resource crunch over which he has no control. The result is disinclination and, over some time, an inability of a general surgeon in general to handle a non-compressible trauma confidently. This has become a significant limitation in the management of trauma in general and has impacted the ability to handle GSW/explosive BI in the hinterland of India, from where a large number of patients are unable to reach well-equipped trauma care centers in time.
CHANGING PARADIGM IN TRAUMA CARE DUE TO WAR AND TERRORISM
GSW/BI in warzones/special operations differ from civilian injuries in many ways in terms of the severity of injuries. However, the number of terrorist attacks and suicide bombers detonating themselves in public have brought home the prospects of sustaining multi-organ trauma in various combinations and of various severity and complexity, a reality, even in civilian life. No one is immune to firearm injury, and it will strike without warning. The wars of the 21st century, especially the Armenia- Azerbaijan war and the Russia-Ukraine war, have also brought home the bitter fact that modern wars are likely to be prolonged affairs. Further deaths will now occur not only in the forward edge of battle area (FEBA) (borders), where the enemy is in eyeball-to-eyeball contact but equally in-depth, as the military targets are being hit by drones and Quadro/Hexi/Octa/Multi/Hybrid copters easily up to 100 km inside the border due to their progressively extended reach. Similarly, the reach of the modern missiles and various forms of guided munitions of our adversary now covers up to almost 1500 km, i.e., practically the whole of our country. Hence, theoretically, all parts of India will constitute part of an extended warzone in a full-scale war. Increased and determined efforts of the enemy to hit valuable strategic targets like parliament, oil refinery, and the stock market in an attempt to break the will of the adversary, especially in urban areas, is a reality and will, beyond any doubt, result in widespread collateral damage. The government has to take cognizance of this and act. Policymakers must carefully frame a comprehensive and realistic policy on this account by constituting a high-powered task force as soon as possible.
IMPACT OF SOCIAL CHANGE ON INCIDENCE OF CRIME
The instability of the social fabric due to the aspirational upwardly mobile population of India may increase the incidence of violent crimes. This may be further fueled by the easy availability of small firearms (indigenous as well as foreign-made), both legal as well as illegal. Hence, a progressive increase in the crime rate is inevitable unless urgent corrective action is initiated. Further, since nobody is insulated from firearm injury without predictability in time and space, social reformers have a big role to play.
HOW TO STRENGTHEN NETWORK AND ACCESS
Injuries will never fade, even if all diseases are conquered. Gunshot and BI will become more and more destructive as time passes with ¯scattered pellets, ¯clustered shrapnel, and many newer forms of destructive abilities. This requires India to become ready and develop a robust, workable competence-based region-wise chain of trauma care echelon, with information about its working widely disseminated and in real-time leveraged by all citizens using a widely available and free app mandatorily put in all the mobile phones sold in India with video of basic measures along with an interactive option to seek help at the location of the injured as well as to revise intervention measures. This should be combined with a robust network of emergency care ambulances so that victims can reach the appropriate center as quickly as possible, preferably within the golden first hour. Similarly, all public transport drivers and attendants must be given basic training to stop bleeding and maintain airways as part of a licensing exam. Besides this, by law, they should know the primary and alternate routes to reach the nearest trauma center in their permitted driving area so that no time is lost.
Multiple applications are available to geo-tag a person’s current location. One such application is to be identified/ created de novo and exclusively used for trauma care by incorporating this as a non-arrasable and mandatory feature for all mobile phones and smart watches sold in India. The application should be developed in multiple regional languages. It should be linked with a voice alert feature, “Help me,” in addition to the use of a key/ tap, which will activate a “first response “ and simultaneously show on the mobile screen the location and identity of the nearest trauma care facility along with access road to reach there as with Google map. The screen on the mobile should also pop up an Alarm button, which, when tapped, should initiate the “Second Response,” which does four actions. (a) Emits loud call for help by bystanders (b) Automatically sends an save our souls (SOS) message and a call to the nearest emergency response team along with its designated Ambulance team (c) Activate the camera of the mobile for visual inputs (d) Switch on the current location, so that the electronic medical record (EMR) team can track its location real-time if passer-by has moved him.
Similarly, the emergency response team should be able to respond quickly and, after a quick assessment, send a message to the higher-echelon trauma care facility so that it is forewarned and render continuous help while in transit. The emergency response team should be able to log on to the local police network for safety requirements and the traffic police for road clearance/diversion measures to avoid losing precious time. Adopting the above, the referral problem is dispensed with as the EMR team is the decider, followed by the trauma care centre.
IMPORTANCE OF COMPLIANCE WITH FIREARM REGULATIONS
The Indian Firearm Act is one of the strictest Firearm control provisions in the world. No citizen of India has a constitutional right to own a firearm, as is the case in the USA and some other countries. Criteria for approval of a firearms license may be made even more stringent. All weapons with the caliber of .22 and above should need a permit. Similarly, all air guns capable of delivering 20 joules or more of muzzle energy /with a caliber of more than 77 should require a license.
UP, Punjab, and the state of J&K have the most licenses and the maximum number of illegal firearms. Insurgents in states like Manipur, as well as Left Wing extremists in the state of Chhattisgarh, possess a large number of illegal firearms and improvised explosive device (IED). Mirzapur is considered the biggest hub of illegal weapons. Kodavas are permitted to carry firearms without a license because they are considered born warriors by the British Raj. If this is still in vogue, it needs to change.
In India, a license for non-prohibited bore weapons (NPBW) (bore refers to the diameter of the bullet) is issued by civil police/ DM/State Govt as applicable and, as per Arm Act 1959 and Arms rule 1962, one can carry it if there is a perceived threat to his life. Only two firearms can be issued on one license, whereas prohibited bore weapons (PBW) like pistol (9mm) and handguns (.38 and .455) are issued by the Ministry of Home Affairs, and only 50 cartridges can be legally issued per annum (max of 30 cartridges at a time). Further, the Indian Arms Act of 1959 prevents any citizen from carrying a self-ejecting pistol or gun. Also, sons/daughters are prohibited from carrying the father’s/ mother’s firearm. In India, it is not legal to carry firearms in public, although this is violated with impunity. Possession of unauthorized firearms is punishable by imprisonment of 7 to 14 years and a fine. Similarly, whenever the owner dies, his firearm is required to be either transferred or surrendered to local police. No firearms can have more than a 6-inch sharp edge on any end. Firing a gun in the air has been made illegal in some states like UP, and others should also follow suit.13 These licensing laws are, thus, sufficient but need to be implemented in letter and spirit. This will require immense political will and concerted effort towards law enforcement.
IMMEDIATE INDIVIDUAL RESPONSE TO BLAST INJURY
Some protective measures can be adopted by citizens in general to avoid injury in the event of a threat by bullet/blast. Citizens may be taught, as part of reflex behavior, to lie down flat on the ground with their head away from the direction of the sound of a bullet/blast (reduces target area and protects head and eyes). They should not panic, but on the first opportunity, they should take cover in the nearest safe location and contact the police using the emergency fast dial on the phone. If they notice any casualty in their vicinity, they should be able to act as per the situation’s needs and pull him to a safe zone. Thereafter, the measures to be adopted by the common man to prevent death within the golden hour (for bullet injuries) and within platinum minutes (for BI) are adherence to the simple and easily followed provisions of basic life support. The same is given below.
BASIC LIFE SUPPORT (BLS): STEPS
Quick initial assessment by the first responder is important. First, check to ascertain the scene’s safety and look for debris, shrapnel, and the presence of any malicious intent to harm.
If the scene is considered safe, tap on the shoulder and speak to the victim loudly to ascertain whether the individual is conscious and responsive.
Call for professional medical help and an ambulance.
Stop the bleeding: The first action should be to stop the bleeding by compressing the wound with a clean cloth available next to you and elevating the limb. If the leg is burst and bleeding, apply a cloth tightly proximal to the wound to reduce blood flow.
Look for a satisfactory chest rise and whether it is equal on both the right and left sides with breathing effort. If present but the patient is unconscious, clean the mouth with a dry handkerchief to reduce the chances of airway obstruction and put the individual in a coma position to reduce the chances of the tongue falling back to obstruct the airway and vomit being aspirated in the lung. An unequal rise in the chest indicates pneumothorax and constitutes an emergency requiring prioritization of the need to reach a nearby hospital.
Check for evidence of cervical spine injury. Keep a close watch on breathing effort. If the breathing has stopped, immediately initiate CPR after checking the carotid pulse as per the teaching of BLS. If a pulse is present, continue with rescue breathing only. If a pulse is absent, conduct high-quality chest compression (30 times) on the sternum, ensuring adequate chest recoil to fill the lung with air, followed by 02 rescue breaths. Continue the same for at least one hour/ placement on a ventilator, whichever is earlier, continuing to watch for and manage bleeding from the wound simultaneously.
-
This CPR is to be continued by a passer-by in rotation (too tiring for a single person) till an ambulance/equipped doctor/ paramedic reaches you.
Note: - Rescue breath is useless if the heart does not carry the blood (oxygen) across to other body parts. Hence, in effect, CPR is a delicate balance between forcing the heart to start from under the ribs while being gentle enough not to puncture it. Hence, this simple CPR+ BLS course is a must for the general public to know and must be incorporated into all First Aid courses properly to attain the status of 100% informed citizenry. Once inside a hospital, the trauma protocol action needs to be activated.
BASIC TRAUMA LIFE SUPPORT (BTLS)
BTLS differs from BLS in that it trains the learner to stop the bleeding, assess deformities (abnormalities in the shape of a body part or organ compared to the normal shape), contusions (bruising which in extreme cases may lead to significant blood loss with blood leaking into surrounding tissue), abrasions (may be simple or contaminated with IED debris), puncture/ penetrations (ability to opine that the object did not pass through), perforations (when searched consciously to find whether the object has passed through with an entry and exit wound), burns (extent and degree), lacerations (how deep below the skin and likely underlying structures it could have damaged), tenderness (may be muscle tear or a fracture, etc.), swelling (due to blood collection, expanding hematoma etc.) on a scientific and analytical manner with focus on what to suspect and act accordingly. This involves critical thinking and objective assessment of firearm injuries by looking for clinical presentations other than airway, breathing, circulation, disability & exposure (ABCDE) taught in BLS. The student is also taught to handle immediate post-traumatic shock episode, which occurs on seeing dead bodies and ghastly injuries strewn around in a major blast injury and is, at times, a cause of sudden death on account of a very intense adrenaline surge (Broken Heart Syndrome).14
Military surgeons are conversant with the correct approach to treating trauma through their training since the Armed Forces put a lot of effort into training their soldiers and paramedics in BTLS, Nurses in ATCN, and doctors in ATLS. In the last few years, the AIIMS JPN Apex Trauma Centre and some similar institutes have spearheaded the effort to disseminate trauma care knowledge in military and civilian centers. This effort needs to be sustained and expanded as much as possible.
Need for advanced training and teaching
Training (skill development) and teaching (achieving theoretical clarity of the subject matter) are integral to any progressive effort and must be sustained to maintain the gains achieved. The National Board of Examinations has recently begun registering courses in trauma care, although in a very limited manner. Similarly, paramedic training, although done at many institutions, lacks accreditation, a structured review program, or assessments for periodic updates of skills and knowledge in the field of trauma and bullet/BI. Hence, their actions, however well-meaning, get translated into widely varied and individualized treatment meted out by the first responders, including attending doctors unsystematically (although with good intentions), leading to preventable deaths. This is reflected in the glaring fact that in the Mumbai terror attacks, out of a total of 271 casualties encountered, 175 people (including 9 terrorists) died,108 were dead after admission (68 due to bullet injuries,30 due to BI, and 10 had both). Six postoperative deaths were all due to GSW. This indicated that the impact of severe bullet and BI could not be addressed adequately, and potentially salvageable patients could not be operated on within an acceptable time frame.
Role of civil defense volunteers in BLS/BTLS
The members are usually nationalist, motivated, and well-meaning citizens. However, the civil defense forces lack trained personnel to provide BLS or BTLS. This captive and easily identifiable group must be given organized training.
TRAUMA CARE ONCE IN HOSPITAL
The super-specialist doctors of the country are fully competent to tackle complex trauma concerning their field of expertise. However, only a minuscule proportion of trauma victims can reach well-equipped super-specialized care facilities since such super-specialty centers are all located and clustered in big cities where patients of all types of illness come from villages, rural districts, towns, and tier 2 cities.8,10,15,16
Those super-specialists who work in the suburbs of cities and smaller towns work by and large in a relatively modest private set-up, which often do not have the technical/ medical equipment and supporting facilities, including trained staff required to treat complex trauma like cardiovascular and lung injuries, complex pelvic or brain trauma, or major abdominal solid organ and large vessel tears, and hence are unable to utilize their available domain expertise fully which often results in preventable death.
However, general surgeons and orthopedic surgeons form the mainstay of medical professionals available in non-metros, and they are now imparting primary care and conducting definitive surgery in the field of GSW. On receipt of complex firearm-induced trauma, if definitive surgery is not feasible, they try their best and perform damage control surgery and can do a reasonable job provided they have acquired the expertise to treat trauma involving all areas of the body during their postgraduate training or have undergone a course focused on treating complex trauma. This is a critical point since this group of professionals forms the most important intervention echelon in the width and depth of the country and can save lives in a very significant way by successfully stopping a major bleed, combating shock, and, if required, helping/ transferring the patient to a proper trauma care facility. GSW and BI victims require intensive care unit (ICU) care both at admission and in post-operative care. A survey showed that only 47% of district hospitals (>300 beds) and only 5% of district hospitals (<300 beds) had an ICU of reasonable standard.17,18
TRAUMA CARE CENTERS IN INDIA
District hospitals in India were designated as level III Trauma Care Centers in the 12th five year plan, catering to an injured’s initial evaluation and stabilization. medical colleges & hospitals with bed strength of 300 to 500 were identified as Level II Trauma Centers committed to providing facilities to provide definitive care for severe trauma victims with in-house emergency physicians, surgeons, orthopedic surgeons, and anesthetists. The medical colleges and hospitals with more than 500 beds were planned to have a Level 1 Trauma Centre to provide the highest level of definitive and comprehensive care for patients with complex injuries. However, this has not been fully realized and highlighted in various reports. Police records give a fair indication of areas with a high number of gun violence. The recommendations of Niti Aayog’s report on emergency and injury care at secondary and tertiary level centers in India have, although focused on road accidents in a major way, should also be integrated into the trauma care framework. The local government, at least in urban areas, must be armed with a dynamic strategy whereby, from these areas, the victim of firearm injury can be shifted to a trauma care facility within 30 min.
As per a Times of India report published in 2017, in Maharashtra, out of 18 trauma care centers, only three were adequately staffed and functional; the rest were either non-functional or partially functional due to inadequate workforce or shortage of infrastructure.19 Other reports have also flagged the inadequacy of a trained workforce and lack of essential equipment and training.8-10,15
A report stated that only 33% of district hospitals (>300 beds) had emergency operative services for trauma patients.4 In such a scenario, the ability to manage injuries on account of explosive devices, IEDs, bullet injuries, and bomb blasts is a serious question.
BLOOD BANK FACILITIES
The blood bank is an essential component of trauma care. Out of 34 assessed district hospitals, 15 had no blood bank available 24/7, only 4 had an emergency blood transfusion protocol, and only 5 had a massive blood transfusion protocol. Blood banks in larger cities housed as corporate/ private entities are doing much better regarding availability and accreditation.
DISASTER MANAGEMENT DRILLS & POLICIES
Mass shootings and BI can easily overwhelm the resources of a normal emergency department, and the conduct of regular drills to face such disaster management provides the opportunity to plan, prepare, and, when needed, enable a rational response in the case of disasters/ mass casualty incidents. Disasters and mass casualties can cause great confusion and introduce inefficiency in the hospital. However, the capacity to cope with such scenarios exists in only about 35-50% of district hospitals. This capacity must be increased in collaboration and coordination with the district, state, and Indian disaster management agencies, railways, civil aviation, National disaster response force (NDRF), military, and paramilitary organizations.
VIEWS OF THE WORLD HEALTH ORGANIZATION ON TRAUMA CARE
International Society for Trauma Surgery and Intensive Care (IATSIC) is an integrated society within the broader International Society of Surgery and provides guidelines targeted at administrators, ministries, and policymakers under the umbrella of WHO and, from time to time, updates the guidelines for trauma quality improvements program. The report says that 5,800,000 people die of injury every year in this world, with the burden being excessive in low and middle-income countries.
The WHO guidelines bring out the core essentials of trauma care services, which every person in this world should realistically be able to receive, even in the lowest income setting, and encourage member states to improve their trauma care systems using an affordable and sustainable program, identifying problems especially related to system issues, developing reasonable corrective action plans, following through on implementing these plans and evaluating whether the corrective action plan has had its intended consequences. It has also suggested the creation of a death panel review to identify the factors of care that need to be strengthened and the adoption of a modern quality assurance program, especially focusing on patients who have died of low injury severity scores. WHO also has a designated Department of Violence and Injury Prevention and Disability (VIPD), which issues updates occasionally.
India needs to form a similar body and leverage its immense advancement in the field of Information technology, artificial intelligence (AI), and software development capabilities, and aim to create the most extensive database in the field of trauma in the world with GSW and BI being a subset, where records of various agencies, courts, cremation and burial ground, forensic science services, hospitals and medical colleges may be integrated. This will be a big step in improving the care of firearms injuries and forming a robust database, which will be beneficial in achieving a larger purpose of maintaining the country’s security.20-22
AVAILABILITY OF AFFORDABLE EQUIPMENT
Assured and timely availability of technologically and scientifically sound equipment and supplies of medicines and consumables are essential to trauma care. Studies have shown that overall mortality decreased by 15–20%, and preventable deaths were reduced by 50% with improvements in trauma care planning and organization. The development of high-quality and innovative home-grown technology will play a significant role in making trauma care affordable for the middle and lower sections of society.
Many medical devices used in trauma care, like oximeters and ventilators, need lower costs, more durability, and easier-to-repair versions. Indigenization can decrease costs and increase the availability of a range of equipment. Innovations using disruptive technology will be game changers. This is more important in GSWs and BI, where bleeding control is achievable with minimally invasive procedures.
In a study by medical colleges/ tertiary care centers, most of the Hi-Tech equipment was found to be mostly imported. Approximately 90–95% of ultrasonography (USG) and computerized tomography scans (CT), considered essential for the last 40 years, are still largely either imported or sold with minimal make-in-India components of key parts. This is very difficult to accept in a country with such a high electronics and computer technology talent pool. This needs to be addressed on a war footing. The import of foreign equipment also poses a challenge for repairs and maintenance. This leads to a significant downtime. Moreover, due to economic reasons and lack of training, cutting-edge technology fails to penetrate the Indian market, and phased-out and refurbished devices are more commonly marketed in the hinterland of India, which are the usually old models phased out from tertiary care hospitals in big cities of India and abroad. Hence, local production emphasizing Make in India is a necessity that can no longer be ignored to increase the availability of these important technologies and make the facilities available and affordable in middle-level towns and villages of India. Low-investment fields like trauma care in the private sector need low-cost equipment produced in India to succeed for poor people.
The availability of indigenous ventilators and other lab equipment was made possible during the COVID-19 pandemic with firm government policies. The market size of the medical devices sector in India was estimated to be $11 billion (approximately 1 90,000 Cr) in 2020, but its share in the global medical device market was estimated to be only 1.5%.21 This is expected to reach 100 billion USD in the next 10 years as more hospitals come up in the hinterland, causing a loss in foreign exchange. It is time for India to leap forward in the field of manufacture of medical equipment by increasing investment in research and development if we are to achieve a reasonable national aim of 100 billion USD (Rs. 8,500,000,000,000) industry in this sector simultaneously enabling a large number of medical equipment to reach the small towns and villages, thereby taking the level of care in villages much higher. This will be a remarkable feat towards affordable health for all.
REQUIREMENT OF POLICIES AND PROTOCOLS ON CONDUCT OF AUTOPSY
There is a national program for prevention & management of trauma & burn injuries (NPPMT&BI). However, exclusive standard policies and protocols for treating GSWs/BIs are lacking in their role. Most of these victims are treated by in- house protocols of the facilities and are guided by the expertise available in the hospitals. Similarly, there is no policy on the conduct of autopsy. The lack of national policy regarding autopsies has led to significant variations in the number and proportion of autopsies performed at dedicated centers. Autopsy rates seem to vary greatly across cities and regions, as do the proportions of autopsies involving firearms deaths. Imphal, the capital of Manipur, exhibits the highest rate of autopsies on gunshot victims; 42.5 percent of all autopsies were carried out on murder victims, while a lower yet still an impressive proportion involved firearms murder victims. It may be relevant that Manipur is home to the highest firearm murder rate in the country. Whereas Imphal stands out based on its uniquely high recourse to autopsy for victims of firearm murders, a large number of victims in other parts of the country do not undergo autopsy, as a result of which the correct pattern of injuries suffered by GSWs/BI is not reliably available. Hence, a policy needs to be implemented where all GSW/ BIs must be subjected to a ¯limited postmortem focused on the area of interest. If the postmortem is not done for any reason whatsoever, a whole-body CT scan must be made legally mandatory prior to burial/ cremation so that the broad nature of the injury and the likely cause of death can be reliably documented.
APPROACH TO THE MANAGEMENT OF GSW AND BI IN THE MILITARY ENVIRONMENT
In GSW, injuries among individuals using battle protection jackets (BPJs), 60% involve extremities. In other instances, 60-80% of injuries involve the chest and abdomen, which constitutes a vast and unprotected target area that cannot be compressed satisfactorily to stop hemorrhage.
Just as self-care (e.g., packing of shell dressing and use of self-applying tourniquet) and buddy care (like raising legs and applying pressure) are life-saving interventions in battle, informed medical assistance and first aid by passers-by and fellow citizens in civilian life can be of immense use in stopping bleeding due to GSW. Hence, citizens must be trained to use belts/ rope/scarf/pieces of cloth torn out from worn fabric for tourniquets & packing wounds with clean cloth to stop the bleeding. Similarly, wider availability of individual first aid kit (IFAK) in all motorized vehicles (@1 kit per passenger) may be made mandatory so that any vehicle owner can use it in an emergency while transferring a victim to the hospital.
COMBAT SCENARIOS
In the Korean War, which lasted over 3 years, out of 40 lakh casualties, 20 lakh were civilians, indicating the brutality of the war. In the ongoing Ukraine-Russia War, which has now touched 600 days and counting, the total number of casualties due to bullet injuries and explosive action has already crossed 3,50,000 with about 56,000 killed in action (KIA) and about 2,50,000 wounded in action (WIA) indicating a 15-17% KIA rate in the larger context, out of which about 20% were collateral damage i.e., civilian death (9444) which is noteworthy and since most of the death occurred in cities and towns (denser population), must be taken seriously. Only about 15% of soldiers could return to join the battle (RTD-returned to duty), causing a severe shortage of troops ready to fight again, one of the lowest rates of RTDs compared to previous wars. Further, about 85% were either maimed or were dead, which is one of the highest in modern warfare. This is alarming in a war showing no sign of stopping, with many more likely to be affected in the same proportion. This extraordinarily high rate is due to the large number of explosions due to higher generation weapons with much more destructive power, i.e., missile/rocket/drone/aircraft/tank actions conducted up to 300-400 km inside the border and in urban areas. India has a much higher urban population density than Ukraine or Russia. If we as a country have to face a similar situation, our death rate of the civilian population would be many times higher. This new normal will likely be reflected in any future conventional conflict between India and its adversaries. Hence, we must be prepared for it.
Firearms and explosives kill or maim the victims either intentionally or accidentally. The immediate concern is death, either due to blood loss due to the inability to breathe or due to the major disruption of organs in any of the three cavities of the body. i.e., cranial, chest, and abdominal cavity, when the extent of loss becomes incompatible with life. Associated bone, nerve, vessel, muscular, and maxillofacial disruptions may contribute to death in an immediate time frame, although by themselves, they may not be the cause of death. However, it may result in disability in the long term. Bala et al.23 (2008) reported in a study of 181 patients with abdominal trauma after a terrorist bombing attack amongst the civilian population in Israel who required laparotomy on admission to Hadassah Hospital Jerusalem, Israel, in the 5-yr period from 2000 – 2005, there were injuries to multiple body regions in 87.5% of cases, with shrapnel being the leading cause. In the same hospital, the pattern of thoracic injuries consequent to suicide bombing attacks resulted in 52.7% of the patents sustaining lung contusions and 45.5% of victims requiring tube thoracostomy, reemphasizing the requirement of all medics and paramedics to be trained to perform the relatively simple procedure of needle thoracostomy and tube thoracostomy on-site as part of BTLS.
The approach to the problem differs in battlefield, rural, and urban settings since the type of injuries and the availability of facilities to manage the trauma are variable. However, the basic principles of staging casualty care remain the same. These are explained in detail in the succeeding paragraphs.
It is paradoxical that, upon the least trained falls, the most important responsibility is saving lives and managing bullet injuries since the best position to become the first responder is usually the bystander. But suppose the first responder fails in his duty. In that case, the responsibility of the first response falls on the primary care doctor to whom the victim is taken, but after paying a heavy price, i.e., loss of precious time when a victim continues to bleed. Hence, correct decision-making by the bystander is the most important factor that impacts the survival of an individual facing severe blood loss and organ disruption within the golden hour and, at times, within the platinum 10- 30 minutes. Hence, it is necessary to form robust guidelines for casualty care at all levels in a large country with a diverse topography like India, where the barriers to timely care are different for plains, hills, deserts, jungles, islands, hinterlands, heartlands, and border areas due to different time taken to cover the same distances by road /foot/ boat. Similarly, the problems of managing battle casualties in war and conflict zones (both civilians and armed forces) and managing crime scene casualties (both police and civilians) are different and need to be addressed carefully.
TACTICAL COMBAT CASUALTY CARE (TCCC) PROTOCOL
TCCC covers three major aspects of the standard of care for modern battlefield/terrorist operations. These are:
Care Under Fire (CUF)
Tactical Field Care (TFC)
-
Tactical Evacuation Care (TACEVAC)
However, it must be appreciated that these guidelines are not a substitute for sound clinical judgment.
The medico-legal, forensic, and investigation angle to the issue is gaining importance, and it is time we put special attention to this aspect so that the culprits do not get away. Fear of getting caught/identified and punished is essential in reducing crime. Education & awareness programs from the school level & adoption of personal protective measures to minimize impact, e.g., lying down on the ground in civilian life on the sound of gunfights, and the adoption of special measures amongst police and armed forces will also reduce the injury rate. The broader use of surveillance cameras and an increased number of well-equipped forensic science laboratories in every district will become a deterrent to crime to some extent.
Future threats, advances in firearms and explosives, and newer and more ingenious methods to inflict damage need to be weighed closely and factored in a structured and sustained manner as a state policy. Corrective measures need to be instituted continuously with periodic up-gradation. Training and adoption of the Massive Hemorrhage Airway Resuscitation Circulation Hemorrhage and Head Injury Everything else (MARCHE) protocol, along with widening the training network in BLS/ATLS/ATCN as a mandatory component of life skill training from early schooling days is important.
A clear doctrine of optimal usage of casualty care resources is required for casualties occurring in remote areas. It is essential to move the life-saving elements to the point of incident’. Putting undue emphasis on quickly shifting to nearby hospitals to save a life over that of securing vital elements, i.e., respiration, bleeding, and spinal stability, is to be discouraged. Hence, there is a need to invest heavily in Far Forward’s casualty care if preventable death is to be reduced & specific action is initiated towards this before evacuation by road/air. This is essential to prevent delayed medical intervention and improve survival.
Once a patient reaches a primary care echelon, doctors and nurses must possess higher-order skills in 10 areas, and all items required to achieve this must be available on the ground. This applies to both civilian and military environments.
Ability to intubate a patient
Ability to place intra venous (IV) drips & central line & manage shock
Ability to place a thoracostomy needle and chest tube
Ability to pack the abdomen and place a binder to stop an ongoing bleed
Ability to pack an open bleeding wound by hemostatic dressing and apply a tourniquet correctly
Ability to stabilize spine and limb
Ability to do percutaneous tracheostomy and cricothyroidotomy in maxillofacial injuries with flail jaw and tongue fallback
Ability to catheterize/do suprapubic percutaneous cystostomy
Ability to relieve pain without undue sedation.
Ability to safely transfer the victim to the next trauma care echelon
The structure and quantum of medical support must be flexible and pegged with population concentration, limitations of reach due to terrain constraints, and the anticipated intensity of combat/ terrorist damage. Further, once given, the evacuation request should materialize by a clear algorithmic approach to a non-threatening sector/ area with a better trauma care facility. This facility may be a military/civilian hospital (private/public) and must be integrated into the war planning. The Nation fights modern wars as a whole approach with armed forces, paramilitary, airlines, ship industry, industrial complexes, Indian Space Research Organisation (ISRO), National Technical Research Organisation (NTRO), and Defence Research and Development Organisation (DRDO), and the role of more than Indian 1,00,000 doctors, nurses, and the citizenry must be clearly defined to fight the threats faced by an emerging power who aims to redefine the world order.
Interaction between civilian Medicare set-ups and military organizations in peacetime as part of the national effort needs to be expanded and the capabilities of each other leveraged. These organizations, which form the sheet anchor of medical care in India, must integrate in a major way and incorporate the private sector in the effort.
MANAGEMENT OF GSW AND BI
Basic features of explosion and BI
Higher order explosives (HOE) like Tri Nitro Toluene (TNT), C-4, Semtex, Nitroglycerine, Dynamite, and ammonium nitrate fuel oil (ANFO) produce supersonic blast waves that cause direct damage, e.g., Lung rupture, Gastrointestinal (GI) perforation and hemorrhage, ear damage by rupture of tympanic membrane, disruption of the middle ear, rupture of the globe of eye as primary’ damage due to direct impact of blast wave. Secondary injuries may occur due to the effects of projectiles, i.e., damage may occur due to flying debris and fragments, which can lead to penetrating/blunt injuries and fractures in any part of the body, and tertiary’ injuries as the individual gets thrown by the blast wind, leading to head injury, visceral injuries, fracture, and traumatic amputations. All of the above and also the impact of other mechanisms/circumstances can lead to asphyxia/crush injuries/burns/sudden aggravation of existing medical conditions termed as quaternary injury. low impact explosions (LOIE’s), e.g., pipe bombs, Molotov cocktails, and gunpowder, have a much lesser blast effect.
Primary injuries
Blast lung: It is diagnosed by a clinical triad of apnea, bradycardia, and hypotension and confirmed by the characteristic butterfly pattern on Chest X-ray. It may also present as dyspnea, cough, hemoptysis, and chest pain. A chest tube is recommended to be placed prophylactically before transfer by air or before general anesthesia.
Blast ear: - It may present as sudden tinnitus deafness or ear bleeding due to Tympanic membrane perforation, as vertigo or otalgia, or a different combination of the above. Sudden deafness may occur, requiring the written mode of communication in an otherwise normal individual.
Abdominal injury: - A containing bowl may perforate, and solid organs may rupture, e.g., liver/spleen/testes. Acute presentation may be as severe pain in the abdomen of sudden onset or unexplained hypotension/ hypovolemia and, after 24 hours, may present with signs of peritonitis and, after another few days, with signs of sepsis. Hence, an element of suspicion must be there to diagnose this in an otherwise normal bystander near a blast injury reporting to a doctor.
Brain injury: - Mild traumatic brain injury (MTBI) (concussion) without any direct blow to the head may present as headache, fatigue, poor concentration, lethargy, depression, anxiety, insomnia, and other symptoms of post traumatic stress disorder (PTSD). This must be kept in mind since there are no overt injuries.
Non-primary injuries
Any organ/tissue may be injured. Hence, the clinical presentation may be of an unconventional pattern. This may be
-
-
As visible in a penetrating trauma,
-
-
As features of blunt trauma with or without inspection findings
-
-
As air embolism presenting clinically as stroke, MI, acute abdomen, blindness, deafness, spinal cord dysfunction or claudication
-
-
As burn injuries
-
-
As acute renal failure
-
-
As compartment syndrome with tense, painful/anesthetic/pulseless limb
-
-
As features of carbon monoxide (inadequately burnt coal)/cyanide (burning plastic) poisoning if the incident occurs near ammunition storage points and presents as confusion, headache, difficulty in breathing, cyanosis, etc.
-
Important points in management
All medics and paramedics should be mandatorily trained in trauma life support courses as part of their Degree/Diploma/Certificate program and learn the MARCHE protocol.
Recognizing a gurgling sound in the throat as an impending airway obstruction and the importance of placement in a coma position (recovery position) as a reflex behavior amongst citizens cannot be overemphasized. The ability of students in schools to demonstrate BLS capability should be rewarded with additional marks from Class VIII onwards as recognition of a very important skill level.
Ability to stop the bleeding, insert I-Gel, secure IV lines, give fluids, splint fracture, tie a pelvic binder, and insert a needle (in second intercostal space) to decompress a pneumothorax does not require a great amount of training in an aware, intelligent, confident and the rising Indian population. This can become part of Class Xth, XIth, and XIIth curriculum and be practiced on interactive mannequins available as a Make in India product. This has been validated to be an achievable skill among interested non- Medics with no formal training in medicine.
MARCHE PROTOCOL
All doctors, nurses, and paramedics must become competent in resuscitation techniques and follow a standard protocol to minimize omissions of vital steps in caring for the injured. This may be combined with a checklist to ensure and reduce unintended errors.
M (Massive Hemorrhage): Stop the bleeding by application of hemostatic dressing (chitosan/kaolin based dressings) and tourniquet and Inj Tranexamic Acid 1gm IV over 10 minutes in the event of massive bleeding and, if required, repeated hourly to a maximum of 8 hours.
An (Airway): Perform head tilt, chin lift, and jaw thrust maneuver to open the airway, insert the Naso-Pharyngeal airway, suck out the oral cavity clear of secretions to prevent aspiration, exclude spine or pelvic injuries, and place the victim in the recovery position. In extensive maxillofacial disruptions, using naso-pharyngeal airway (NPA)/innovative gel (IGe)/endotracheal tube (ETT) is not usually feasible. Hence, training in cricothyroidotomy in manikins/simulators is important so a person can replicate it in real life.
R (Resuscitation): Needle decompression by 18G or 16G intricate or BT needle in the triangle of safety [with the arm abducted, anterior axillary fold (lateral edge of pectoralis major) & posterior axillary fold (lateral edge of latissimus dorsi) diverges as it descends from the apex of the axilla. Its intersection with a horizontal line at the level 5th ICS (level of nipple in males)] forms a triangle. A needle introduced at the upper border of ribs within this triangle saves the life of a tension pneumothorax patient exposed to GSW/nearby explosion by converting it technically into an open pneumothorax. Similarly, the insertion of a chest tube (ICD) to treat hemothorax (3rd leading cause of death) should be a mandatorily acquired ability for medics, nurses, and paramedics.
The ability to perform this simple procedure along with CPR and stoppage of bleeding should be validated every 5 years and linked with the renewal of a license to practice. Suppose the victim does not have a good breathing effort. In that case, inserting a supraglottic airway like i-Gel is uncomplicated. It is life-saving when combined with ventilation by a self-inflating bag with oxygen and an peripheral oxygen saturation (SPO2) monitor. Any doctor who cannot do this simple action should not have the right to do clinical practice.
C (Circulation): Rising pulse and falling blood pressure (BP) are signs of impending shock, especially if accompanied by intense sweating. They indicate the need to infuse IV fluids to maintain BP at 70 - 90 mmHg systolic (permissible hypotension) until bleeding is controlled. Attempting to elevate the BP beyond 90 mm Hg by infusion of extra fluids may restart a bleed and hence should be avoided in a field situation. A blood transfusion may be required if blood loss is assessed to exceed 1 liter.
H (Hypothermia/Head Injury): Keep the hypothermic patient warm to reduce the chances of coagulopathy and hypothermia. Treat hypothermia energetically to avoid the lethal triad of hypothermia, coagulopathy, and acidosis in polytrauma by the use of thermal blankets and warm air. In a patient with a head injury, instead of Glasgow Coma Scale (GCS), the Alert Verbal Pain Unresponsive score is easy to comprehend for a common population, i.e.
A: Alert
V: Response to verbal commands
P: Response to pain
U: Unresponsive
Head Injury patients should be maintained at a 30o head-up position using blankets and pillows or by lifting the head end of the stretcher. This reduces venous pressure and ensures good venous drainage.
E [Everything else (M-PHAAT-D)]:
M: Monitoring: - Pulse, BP & SPO2
P: Pain Management: - Using Paracetamol/ Tramadol/Morphine
H: Head to Toe examination: - To confirm/exclude additional injuries
A: Address all wounds
A: Antibiotics: - Broad-spectrum antibiotics + Metronidazole
T: Tactical evacuation preparation: - To reduce the time from injury to surgery.
D: Documentation of the care given: - Provide the subsequent treating team with useful information.
GENERAL CONSIDERATION IN PRE-HOSPITALAND REMOTE FIELD SETTING
A normally breathing and fully conscious patient of GSW/BI with a pulse of less than 110/ min and BP of more than 90 mm Hg systolic, and absence of diaphoresis (who is not sweating profusely) needs only the bleeding to be controlled as an immediate measure. Clear mentation + systolic BP > 70mmHg indicates ≤30% blood loss, and here, IV fluid should be withheld in field conditions as it may lead to re-bleed/hypothermia. Hence, only once the person reaches a hospital, a normal BP should be achieved by giving 1 to 1.5 liters of hydroxyethyl starch (HES) or Ringer’s Lactate in an adult to achieve a systolic BP of 90 mmHg and conduct surgery planned.
Application of a tourniquet to control a bleeding wound is generally done 3 inches (10 cm) above the bleeding site, preferably on a single bone, and if it is inadequate to control bleeding, tie another one above it. The junctional tourniquet is of immense value when bleeding from the axilla or inguinal area occurs. Similarly, hemostatic dressing applications are always to be accompanied by adequate pressure to be effective and, if inadequate, may either be topped with a second compression dressing or replaced with a larger one. Inflatable Target Compression Devices are a new addition to the armamentarium to stop bleeding and should be available in all trauma centers. Explosion-induced Traumatic amputations are often associated with multiple and multi-organ injuries. They, hence, are usually accompanied by hemorrhagic shock due to massive blood loss, needing fluid and blood replacement at the earliest, in addition to all the measures given above.
Pure head injury with intracranial bleed presents with bradycardia (slow pulse) and hypertension (high BP). If there is altered mental status with evidence of head injury, but the radial pulse is found to be fast (tachycardia) but weak (hypotension), it should be assumed that there is a second site of bleeding (chest/abdomen/limb) which needs to be searched for. Hemostatic dressing can be either Celox Gauze, Chito Gauze, or quick clot (there is no clear evidence of one being better or worse than the other). Mark all tourniquets at the time of application with a permanent marker. Limb bleed is compressible bleed & torso bleed is noncompressible, which must be kept in mind. A tourniquet can be applied to arms and thigh (single bones) at 250 mm Hg or 50 mm Hg over systolic BP, whichever is higher, for up to 2 hours safely. It must be emphasized that pressure above venous pressure and below systolic arterial pressure increases the bleeding rate from torn veins/venules, and hence, raising the pressure above systolic pressure is very important.
Some important points are:
Bandage may mask bleeding due to capillary wick action and hence to be applied only when bleeding has been controlled by applying direct pressure & splint application.
Do not remove bullet/shrapnel unless confirmed to be away from critical vascular structures on X-ray/ USG, lest it leads to restart of an earlier controlled bleed. It is better addressed in the operation theater.
Limb elevation stops pure venous ooze.
Compress the artery proximal to bleed for 10 minutes until it stops bleeding, and gently clamp a vessel if it is visible. There should be no temptation to explore a wound in a state of hemostasis.
Explosion-induced fracture to be splinted to reduce bleeding and pain
Once the patient is stabilized, wash wounds gently and dress them to reduce contamination
Avoid wound debridement in field conditions to reduce the chances of uncontrolled bleeding.
Respiratory distress in an upper torso trauma merits needle thoracostomy and, if confirmatory, needs to be followed up with a chest tube. Any open/sucking chest wound should be treated by applying a vented chest seal immediately and, if not available, a non-vented chest seal with one side open keeping a close watch.
If possible, insert a urinary catheter and seek transfer to a higher facility. Hypothermia is avoided by removing wet clothes and covering them with blankets and warmers. The explosion may have led to penetrative eye injury. Do not put a pressure patch here; instead, cover it with a rigid eye shield and transfer it to a higher center. Explosion-induced burn injuries are common and are to be treated along standard guidelines, as are fractures due to the off effect. Keep in mind the possibilities of chemical/thermal injuries to the airways of the lung, especially when an explosion is sustained in a closed room since this patient is likely to have chemical pneumonitis and may have to be intubated early.
-
Safe Intubation can be ensured by adhering to the presence of essential items using a simple checklist, as per SOAP ME, in the ambulance and emergency department.
S: Suction machine with preferably a Yan Kauer tip
O: Oxygen cylinder, Bull Nose fitting, Bains Circuit, Ambu Bag
A: Assortment of NPA. oropharyngeal airway, supraglottic airway (laryngeal mask airway, IGel), ETT Masks, bougie and Stylites
P: Neutral Position, especially if spine injury is suspected
M: Medication: Ketamine/Etomidate, succinylcholine/ Rocuronium, Phenylephrine, Atropine, Adrenaline
E: Equipment: Video Laryngoscope, Multiparameter Monitor, preferably with EtCO2, Cricothyroidotomy set, percutaneous tracheostomy set, Standard Tracheostomy set, and Endotracheal tubes are mandatory items in an emergency department.
Once resuscitated, as far as possible, use fresh whole blood to replace blood lost since it has sufficient levels of 2-3 diphosphoglycerate (2,3-DPG) & does not have the problems of hypothermia, acidosis, hyperthermia, and high cytokine levels. The inotrope of choice to treat hypotension in combat trauma is noradrenaline, except in high spinal injury with Bradycardia where dopamine is preferred. If a second Inotrope is required, Vasopressin should be added. Use dextra ethyl starch solution as an interim measure if blood is not available to treat shock.
Urine output is a good marker of organ perfusion. When arterial blood gas analysis (ABG) is used, base deficit & lactate level are the markers of adequacy of resuscitation. Serial hemoglobin is required to assess the need for blood transfusion to reach 8-10 gm %, and once this is achieved, scale back the fluid/blood to avoid pulmonary edema/adult respiratory distress syndrome (ARDS).
-
Thus, the ten main essentials for saving lives are:
Triage
Management of difficult airway (MODA)
Avoidance of the lethal triad of Hypothermia Coagulopathy & Acidosis (HCA Syndrome)
Prevent ACoTS – Acute Coagulopathy of trauma shock
Damage control resuscitation (DCR)
Damage control surgery (DCS)
Excellent Pre-hospital Care & resuscitations
Robust Transfer facility
Excellent post- operative Critical care management
Rehabilitation of injured
In injuries sustained in remote areas, the severity and lethality factors are much. The evacuation to even a basic trauma care center is usually delayed due to administrative constraints, rugged terrain, hostile environment, snowbound/jungle/desert/marshy areas, and facilities to treat surgical trauma being located far off, necessitating provision of house’ & On site’ management within the golden hour. The positive aspects are that the injured soldiers are generally young, healthy, and have a good physiological reserve; hence, if proper intervention is done within the golden hour, chances of survival increase substantively. Therefore, all efforts should be made to plan timely interventions.
If any evacuation is expected to take a long time, it is better to stage it with periodic re-assessment and corrective actions. Communication (telephonic/Internet-based App) helps guide interim treatment and plan safe casualty evacuation (CASEVAC). Decide who will accompany the wounded casualty based on competency requirements. If the time to transfer to the nearest hospital is more than 1 hour, administer Inj TXA (Tranexamic Acid) 1gm (100 mg/ml) intra venous/intra osseous over 10 minutes repeated hourly for up to the next 8 hrs. It works by stopping blood clots from being broken down.
Special points for Ships: Care for merchant ships under pirate attack at high seas has to be given closest to the site of the operation/ incidence, including damage control surgery at sea before evacuation to a unit/ hospital with bigger holding capacities and better capabilities. In ships with closed compartments, explosions lead to shrapnel injuries. In the absence of safe zones in the sea, the possibility of casualties being carried out is limited. Hence, moderately advanced life-saving facilities must be provided, considering replenishment is impossible at high sea. Therefore, self-aid buddy care (SABC) has special importance, emphasizing 15 minutes of direct pressure, tourniquet, suction, IV access, and needle chest decompression until doctors can attend to the victim.
GENERAL CONSIDERATION IN HOSPITAL MANAGEMENT OF BULLET AND BI
A hospital where a bullet/ blast injury patient has arrived must always be in a state of readiness to receive them. The hospital’s critical care team on call must be on the premises when the patient arrives. Hence, it will be of great value if the information on impending arrival is transmitted to the nearest trauma hospital well before by a centralized web-based helpdesk. The various actions expected are as given below
Confirm readiness for combat trauma anesthesia using a carefully prepared checklist.
The ATLS/MARCHE protocol is to be followed as given above. The main points for consideration are
Wide bore IV access + Hb level + Grouping and cross matching
Extended Focused Abdominal Sonography in Trauma (FAST):
Check for Fluid/Blood in
Peritoneum
Pericardium
Pleural cavity
Start broad spectrum Antibiotic cover, e.g., by triple drug-Cefotaxime+ Amikacin+Metronidazole
Relieve pain and anxiety with Opioid + Non steroidal anti inflamatory drug (NSAID) combination
Regional anesthesia/blocks for targeted pain relief
Vasopressors & fluid resuscitation to treat hemorrhagic shock
Inj TT 0.5ml if immunization status is not known
Prioritize in the event of a mass casualty and decide
Who has more chances of survival
Who will give some more time for intervention
Who will eat away more time at the cost of more lives
Who can be evacuated only by critical care team & who can go by standard ambulance or a passenger vehicle with citizen paramedics?
If early total care (ETC) is planned: Intervene on day 1 (Silver Day) only if the patient is stable hemodynamically and has normal respiratory rate, temperature, urine output, coagulation profile, and lactate levels.
If DCS is contemplated, ensure that a backup primary critical care facility is available to transfer patients out by patient transfer unit (PTU)/critical care air transfer team (CCATT) quickly if necessary.
DAMAGE CONTROL RESUSCITATION
Effective hemorrhage control with restricted volume replacement strategy, enough to ensure critical organ perfusion, indicated by a permissive hypotensive state of systolic BP of 70-90 mmHg (MAP 50-60 mmHg) till major bleeding due to gunshot/explosives has stopped, ensures clot integrity and obviates dilutional coagulopathy, hypothermia, and acidosis. However, in traumatic brain injury, MAP of >80 mmHg is recommended. Tranexamic acid loading dose of 1gm over 10 minutes followed by maintenance infusion of 1gm over the next 8 hours is recommended whenever bleeding cannot be controlled.
-
Anesthetic considerations: Maintain a neutral position by removing only the front half of the Philadelphia collar while intubating when performing RSI. In field situations, the patient should not be paralyzed unless ventilation with a bag and mask is possible. Avoid drugs like Propofol & Thiopentone for induction since they can cause hypotension in a bleeding patient. Hence, Ketamine and Etomidate remain the drugs of choice for induction, and succinylcholine to induce muscle paralysis.
Algorithm for damage control resuscitation is as given in Figure 1.
Remember to secure the ETT/Tracheostomy well against dislodgement during transport and watch for a drop in BP following intubation.
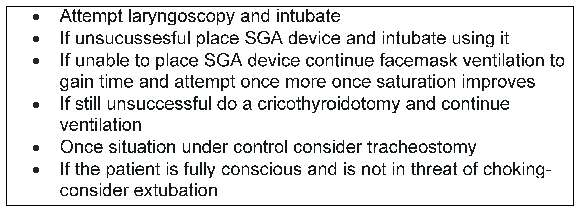
- Algorithm for damage control resuccitation. SGA: Supraglottic airway
DAMAGE CONTROL SURGERY (DCS)
Indicated ongoing bleeding in a severely injured victim who is progressing to hemorrhagic shock. Damage control intervention in compressible areas (limbs) may be done if ischemia is imminent. e.g., to restore femoral/brachial blood flow. Similarly, one may be required to intervene in inaccessible major organ injury needing interim intervention to buy time for a definitive surgery once the patient stabilizes.
Ketamine remains the mainstay for induction, and thereafter, a volatile anesthetic agent can be used for the continuation of anesthesia.
Rapid sequence intubation with readiness for cardiac arrest and resuscitation is a key element.
Stop the bleeding: If direct pressure for 5 minutes fails to stop rapid hemorrhage, it indicates an arterial injury or large venous rent.
Once the bleeding is under control, aim to achieve permissible normotension (systolic BP of <100 mm Hg)
Monitor volume status by maintaining urine output at 0.5 ml per kg body weight
Do not attempt extubation after DCS for 24-48 h until the decision to conduct or not conduct a relook surgery is taken if the patient is in a definitive care set-up. If the care required is beyond the hospital’s capability, transfer the patient to an intubated state.
Keep patients warm by using fluid warmer ‘and forced air warming system’
While evacuating, ensure the correct complement of medics/ paramedics, emphasizing maintaining a lung-protective ventilatory strategy.
Scalp bleed is best stopped by running and locking vertical mattress suture guided by everting the skin edge with a hemostat.
In the case of open head injury with skull fractures, the loose fracture fragments of the skull should never be pushed into the brain by compression and should be removed. Place petroleum medicated gauze, with a wide dressing over it, with gentle pressure, till the patient reaches the neurosurgical center in a 15° head position.
In all major injuries, a self-retaining Foley catheter is placed to monitor urine output once the patient’s vitals are stabilized.
Pelvic injuries are to be managed by placing a pelvic binder/ bed sheet/large towel at the level of the greater trochanter and securing it with tight knots/pin/ stitch
Pain relief reduces systemic response and preserves victims’ morale. This can be achieved by Injecting Paracetamol 1 gm, Tramadol 100 mg, and Morphine 3 mg, repeated for 6-8 hours. Nerve blocks are very useful for pain relief and must be used whenever feasible to help reduce the requirement for opioids and other sedatives.
Limit DCS’s aims only to control bleeding to save lives and salvage limbs. Stabilize after that and transfer. Defer repair of anatomical lesions. Aim to restore physiology instead.
Amputate nonviable limb with vascular injury. Use temporary shunts for emergency vascular repair.
Laparotomy, if done, pack to stop bleeding with the safe application of clips and use a vessel sealing device, with no attempts to attempt ETC, which should be left for the higher center.
Special attention is required if
Age greater than 70 years (higher risk due to age and co-morbidity)
Systolic BP less than 90mm Hg (impending shock)
Base deficit ≥ 6 (Acidosis)
PTT > 40 sec or INR> 1.4 (Coagulopathy)
GCS ≤ 8 (severe functional/anatomical brain compromise)
Timeline to intervene
Day 1: Only DCS to restore physiology.
Day 2-4: Only a second look procedure since the body is Hyper-inflamed.
Day 5-10: Definitive procedure (window of opportunity)
Day 10-20: State of immune suppression, no intervention
Day 20 onwards: Secondary reconstructive surgery.
After surgery, keep the patient warm, restore volume deficit, prevent coagulopathy, give ventilatory support (if required), and monitor well.
As a thumb rule, do not remove the abdominal pack for 48 hours unless compartment syndrome sets in. DCS is unsatisfactory and is a cause of concern due to insufficient initial control of spillage from the gut or if signs of infection set in. In such circumstances, it is prudent to re-examine under controlled settings, change packs, achieve hemostasis, decontaminate, and make a feeding jejunostomy/gut diversion. A check X-ray is necessary to confirm the removal of the old abdominal pack.
Desperate’ re-exploration in coagulopathic, acidotic unstable patients is to be attempted only in higher centers and never in mass casualty situations, where it is better to concentrate on the salvageable.
DCS for chest injury
Thoracic Injuries due to blasts and firearms need quick interventions
If voice is normal, any chest injury with difficulty in breathing is a candidate for needle decompression followed by chest tube insertion.
Distended neck veins in the presence of hypotension and clear breath sounds indicate cardiac tamponade and merit an emergency pericardiocentesis (preferably USG /FAST guided), followed by transfer to a higher center.
Hemothorax merits tube thoracostomy. Blood >1500 ml or flow rate of > 300 ml per hour merits thoracotomy and non-anatomic stapling of lung & blood transfusion to save life.
Open pneumothorax needs a one-way flap seal on the wound, followed by tube thoracostomy at another site on the same side, after which the original wound may be closed by a tight suture followed by planned transfer.
-
Flail chest: - Assume co-existing underlying pulmonary contusion.
Control pain by non-narcotic drug or by block (intercostal/paravertebral) and even epidural analgesia if feasible. Signs of desaturation merit intubation and evacuation.
DCS for thoraco-abdominal injuries
Any bullet injury below T4 (nipple level) merits evaluation for abdominal injuries.
Abdominal trauma
The most important decision is whether to operate in a remote area or a forward surgical center. This is done by balancing one’s ability with the limitations of the facility and the possibilities of a safe evacuation. The decision should be based on appreciating the limitations of the facility’s diagnostics, the limitations of the facility for supportive care, and the probability of safely transferring a patient within a specified time limit to a higher center.
Bullet/ penetrating injury between the nipple and pubic symphysis in front and from the tip of the scapula to the sacrum behind indicate retroperitoneal/intraperitoneal injury.
Focused Assessment with Sonography in Trauma (FAST) is very beneficial in the absence of which diagnostic peritoneal aspiration (DPA), i.e., Four Quadrant Tap ‘should be done in field conditions and, drawl of 10 ml or more Frank’ blood from any one quadrant constitutes an indication for early laparotomy. If the facility is unavailable, it merits transfer by the fastest means to a higher center.
FAST indicating a lodged bullet outside the peritoneal layer can be extracted, avoiding a full laparotomy provided DPA is negative and no free gas under the diaphragm and hemoperitoneum is excluded.
Laparotomy
In Laparotomy for trauma, the general guidelines are: -
Midline full incision under broad-spectrum antibiotic cover.
Pack all four quadrants while searching for injuries.
Stop the bleeding: Clamp/staple/stitch on sighting the fresh bleed under direct vision.
Reassess an unstable patient continuously and consult senior colleagues whenever possible.
Visualize all solid organs and hollow viscus.
Right/left medial visceral rotation, to expose retro-peritoneal injuries, to be attempted only if the experienced surgeon is present and avoided as far as possible in a field condition.
Complete surgery within 1 hour (patient is usually unstable).
If necessary, avoid post-operative abdominal compartment syndrome by temporarily closing the abdomen with a mesh or plastic bag (Bogota bag) and placing an NG Tube and urinary catheter to reduce intra-abdominal pressure.
Retro-peritoneal gas indicates duodenal or colonic injury and may be sutured/drained/diverted based on competence level.
Pancreatic injury – Don’t disturb unless bleeding actively.
Rectal bullet injury may be associated with pelvic fracture fragments. Packing in a field situation is safer. Later, it can undergo primary repair with a proximal loop colostomy.
During DCS for abdominal injury, the steps are:
control hemorrhage
check the extent of the injury
control contamination (resection/washing)
do therapeutic packing and close temporarily
Liver injuries
Once confirmed by FAST, operate only if unstable; otherwise, transfer to a higher center. If compelled to open as part of DCS, pack the liver, spray hemostatic fluids on the bleeding surface, plus give Tranexamic Acid (TXA) (intravenous). Transfer blood if the situation permits. Definitive surgery should be done only in higher centers.
Splenic injuries
Once confirmed by FAST, splenectomy is only if there is ongoing bleeding—no role of splenic conservation in GSW injuries.
Head injuries
Gunshot penetration may be accompanied by bleeding from multiple orifices (ear, nose, and mouth). In contrast, the blast effect on the brain may present subtly as cognitive dysfunction, inattention, loss of concentration, reaction time delay, and posture imbalance. The important points are
Look for mentation and diaphoresis; the presence of hypotension indicates a second injury other than the brain since isolated closed head injury presents as hypertension.
Assume cervical spine injury and apply a Philadelphia-type collar. Examine the scalp for entry/exit wound.
Intubate to correct hypoxia, infuse to correct hypovolemia
Gently examine the scalp for loose fracture fragments, and after gently washing with saline, place a sterile drape.
Do not pack ear/nose/throat in an ongoing bleed to prevent intracranial collection of blood. Take an AP and Lateral X-ray, including Cervical Spine
Quickly conduct CASEVAC except in life-threatening extradural haematoma (EDH)/subdural haematoma (SDH). Do emergency craniotomy to avoid a decorticate/ decerebrate state.
While planning evacuation, the general principles are:
Unconscious – intubate and transfer thereafter.
Wide decompressive craniectomy, before transfer in desperate situations, enables survival and enables the opportunity for definitive treatment in a higher center later. Preserve the loose cranial segment in the saline/ abdominal pocket.
Critical care team must accompany evacuation.
Pelvic injuries
Check for entry/exit of the bullet’s path and make a calculative guess.
Make only one careful attempt to assess the mechanical stability of the pelvis by compression and distraction. If unstable, apply a pelvic splint.
Watch for leg length discrepancy, scrotal/labial swelling, ecchymosis, and abrasion, suggesting pelvic ring injury
Per rectal/Genito, the urinary exam rules out/confirms the presence of a compound fracture. X-ray (AP view) + FAST confirms blood/gas in the peritoneum.
If blood in meatus/urine - FAST guided suprapubic cystostomy is a simple option
Possibilities of retroperitoneal hemorrhage and coagulopathy to be kept in mind and may require transfusion of blood and blood products.
Pelvic binder/bed sheet tied tightly at the trochanter level/placing sandbag/bean bag at the trochanter level/lying in lateral decubitus with injured side down & ankles tied (internally rotated femur) helps reduce bleeding. An external pelvic fixator may be applied on transfer to a higher center. In desperate uncontrolled arterial bleeding, stop the bleeding by the retroperitoneal pack with a suprapubic incision.
On laparotomy, if you see a controlled retroperitoneal hematoma, never open it. Just do a diversion colostomy if necessary.
FRACTURE AND ASSOCIATED SOFT TISSUE INJURIES
Dictum is delayed primary closure of the contaminated wound
Bullet-induced open fractures in field condition should only be splinted, with a close watch for neurovascular deficit and onset of compartment syndrome
Blast injury-induced fracture needs irrigation and debridement and the application of cast/slab with a window/external fixator.
Pain on passive extension, tense edematous limb, and loss of sensation in the first webspace in the foot are signs of impending compartment syndrome and merits fasciotomy.
Mangled extremities due to rip-off limbs (when at least three out of the four, amongst soft tissues, bones, nerves, and vessels, are damaged) with ongoing hemorrhage merits consideration for amputation as a part of DCS & DCA
Warm ischemia time of more than 6 hours merits consideration for amputation of limb at an appropriate level as a life-saving measure.
The guiding principle is Always saving a life over limbs whenever possible.
Use of loupe magnification, good lighting, and tourniquets helps visualize tissue better
Whenever in doubt, excise muscles, fascia, and loose bones but conserve skin.
Since collaterals may maintain distal perfusion, it does not exclude major vascular injury in the limb but gives some more time to respond. One must watch out for an expanding hematoma, which may be addressed by a temporary shunt using plastic IV tubing/drain tubes/reversed vein graft interposed if expertise exists. Heparinize only if there is no other threat of uncontrolled bleeding.
Nerve transactions should be marked by colored, non-absorbable sutures for easier identification by the surgeon later.
Dressing of wounds should be done with sufficient pressure to stop the bleeding. However, toes and fingertips should remain exposed whenever uninjured to continuously assess the vascularity.
Amputation: - Clinically reddish-brown urine in a dead limb ‘indicates Myoglobinuria with impending ARF and weighs in favor of a decision towards amputations.
SURGICAL CONTROL OF VESSEL BLEED
Temporary shunt should always be attempted in major vessel injuries, failing which quick ligation and control of bleed become necessary to save a life. Advanced training to approach proximal subclavian vessels through midline sternotomy/anterolateral thoracotomy/clavicle head resection is uncommon, but if present, it is very valuable in a remote location where an endovascular facility is unlikely.
To save a life, the vessels which may be ligated without a major deficit in a GSW & BI are:
Vein: - External Jugular (both sides), Internal Jugular (one side), Brachiocephalic, Infrarenal IVC, left renal, Internal Iliac, subclavian, mesenteric, Tibialis anterior/Tibialis Posterior/Peroneal.
Arteries: - Digital, radial/Ulnar (one of two), external carotid, Brachial distal to profound brachii, internal iliac, profounda Femoris, hepatic artery.
LABORATORY AND IMAGING SUPPORT
Complete blood count (CBC), serum electrolytes, blood sugar, renal function test (RFT), liver function test (LFT), creatinine phospho kinase (CPK), and blood lactate are desirable tests that require making available. Prescreened blood and blood products are preferable, but if not feasible, fresh whole blood is to be used after testing for Human Immunodeficiency Virus (HIV)/Hepatitis B Virus (HBV)/Hepatitis C Virus (HCV), syphilis, and malaria (preferably by card-based test) as per National Aids Control Organisation (NACO) guidelines along with blood grouping and cross-matching. Temperature criteria for the preservation of kits must be carefully maintained.
Hand-held X-ray and USG with convex sector/curvilinear transducer is a valuable tool for detecting bullet fragments/splinters, pneumothorax, hemothorax, fractures, hemoperitoneum, and torn/damaged solid organs.
FAST: Uses 3 to 7.5 MHz curvilinear/sector transducer. USG performed within 5 minutes of arrival in the presence of an overwhelming number of casualties due to bullet/explosion/BI is an extremely beneficial test to diagnose the problem of hemothorax/pneumothorax/haemo-haemo-pneumoperitoneum in an unstable patient. The standard views to be taken care
Longitudinal right upper quadrant - To look for fluids in perihepatic/subphrenic/Morrison’s pouch
Longitudinal left upper quadrant - To look for fluids in peri-splenic, splenorenal, and subphrenic areas
Suprapubic view- To look at the pouch of Douglas
Transverse Subxiphoid view- To look at Mediastinum and pleural space for hemothorax)
Right and left lateral view – To look for fluid at right and left paracolic gutters
General view- To detect solid organ injuries
During an ultrasound examination, assuming the Trendelenburg position helps transfer fluids to the upper Quadrant and the Anti-Trendelenburg position to the pelvis gives a better diagnosis window.
E- FAST: - Higher frequency linear transducers used with dual probes of 3 - 3.5 Hz and 7-12 MHz are now available in the market and used to diagnose Pneumothorax better by detecting
Absent pleural sliding
A line more numerous than normal and placed unevenly
Absence of B lines
Signs on M-mode ultrasound barcode or stratosphere sign.
IVC diameter evaluation to access hypovolemia: Using a subxiphoid approach with a transducer in sagittal orientation, the IVC diameter 2 cm below the Cavo Atrial junction is measured. IVC collapsibility >12 to 15% indicates volume depletion levels and the requirement to step up fluid/blood.
Solid organ injury: - Look for
Subcapsular collection in the Liver/Spleen
Heterogeneous appearance of liver/spleen parenchyma – indicates bleeding/injury/ damage
Echogenic area within the liver/spleen parenchyma suggests laceration.
MEDICO-LEGAL ASPECT OF GSW AND BI
GSW/BI in a combat scenario are treated with implied consent for emergency care in a combat zone. However, legally valid consent is important for elective interventions.
Identification of death in war zones should be carefully done ethically and morally.
Even a bullet-infected patient has the legal right to autonomy and self-determination enshrined within Article 21 of the Indian Constitution and can refuse treatment unless the intervention is labeled emergency.
Informed refusal also forms an important part of informed concern, and a patient may choose for intervention only in a higher center. Hence, legally valid consent is important. However, in a tactical combat scenario, only implied consent is sufficient, provided an imminent threat to life or limb exists.
When GSW/explosive blast injury gives you some time for a second opinion, it may be taken if required.
Death in combat zone/terrorist operations/civilian life merits clinical autopsy/Medico-legal autopsy after clearance by military/ police/UN observers, and records of it are required to be kept in safe custody
Victim of bullet injury may wish to make a dying declaration. In such circumstances, the magistrate of the enemy country is intimated. When he cannot come, the MO may record the Dying declaration’ after certifying the soundness of mind in the presence of 2 witnesses whose signatures are affixed to the document. A video of the dying declaration may be recorded if in a hospital.
The personal effects of the victim should be disposed of correctly.
Radiographs, Fingerprints, and basic dental data must be recorded and matched to establish identity.
In war injuries, the international code of medical ethics, laws of armed conflict, and the International Convention on Human Rights (Geneva Convention) should be followed, and matters of conflicting loyalty should be addressed.
RECOMMENDATIONS OF TASK FORCE GROUP
The key recommendation of the white paper is as given below:
Policy formulations, facility improvement training, education, and awareness programs on medical aspects should be targeted
-
To address the issues related to lack of the lack of data about gunshot & BI:
Problem: How many cases of gunshot or BI are treated in civil and armed forces hospitals in a year? No data is available since there is no trauma, gunshot, or blast injury registry.
Recommendations: Eminent institutes may be entrusted with establishing a well-funded, well-staffed independent department. There is a need to develop countrywide Trauma registries to know the exact number of gunshot injuries and BI, age group, occupation, gender, causes, circumstances, nature of firearm/explosives used, part of the body affected, high-risk areas, high-risk groups, and so on. Only then will the pattern and likelihood become apparent.
-
To address the issue of insufficient knowledge amongst citizenry about the ‘First response’ to gunshot & BI
Problem: Action taken within the first 30 minutes to stop bleeding and maintain respiration usually decides whether the victim will live. However, most of the victims do not reach the nearest trauma centers within this time. Often, patients are taken by bystanders/ good Samaritans without any measures to stop the bleeding or secure the airway due to a lack of knowledge about how to do it. Every year, a large number of precious lives are lost unnecessarily.
Recommendations: All children from the school level be taught how to stop bleeding from a wound and how to give CPR by the periodic practice of First Aid from class VIII onwards, teaching them the basics of Life Support (BLS) in class VIII and IX, and making BTLS a compulsory part of Class Xth exam. Unskilled and untrained citizens could easily perform this in a trial setting. Hence, all citizens of India should know this and should not be left to medics and paramedics to whom a victim does not reach soon enough
-
To address the issues related to the quality of Patient management:
Problem: There is no fixed protocol followed in managing patients with gunshot wounds or BI in the majority of hospitals. In most tertiary care level hospitals in civil setup, super-specialists work on contracts and are available only on calls. In many hospitals, patients are managed locally according to the system in vogue. The surgeon managing thoracic injury may not be comfortable managing an abdominal or vascular injury. There is a scarcity of trained and experienced surgeons who are capable of analyzing the patient as a whole and who can understand the deranged physiology of the patient due to simultaneous injury to the multiple anatomical regions of the body, be it thoracic, abdominal, vascular injury or head injury and take a quick decision when to operate and when not to operate.
Recommendations: We need to shift patient management from a based to a holistic approach by ensuring that all diploma holders, graduates, postgraduates, and post-doctoral medics and paramedics must be trained in BTLS and ATLS, which needs to be incorporated as part of their educational qualification and validated by an independent agency. Once in a hospital, trauma management should be based on an established protocol and checklists, which, when followed, should provide reasonable protection from litigations. Further, all surgeons (including superspecialists) must conduct a minimum of 10 life/limb surgeries in a trauma center every 2 years as part of renewing their licenses. The specific issues about educational standards, certification, continuing education, and evaluation requirements for doctors involved in trauma care are yet to be fully addressed, and the time has come for a high-powered team of experts cum policy makers to deliberate on it and evolve a National Policy on the matter linked to license to practice.
-
To address the issues related to lack of Rehabilitative services
Problem: There is a lack of knowledge on the socio-psychological impact of gunshot injury and blast injury on the survivor and their families. PTSD (Post-traumatic stress disorder) is characterized as failure to recover after experiencing a terrifying event. This brings back memories of the trauma accompanied by intense emotional (flashbacks) and physical (pain, trembling) reactions due to heightened reactivity to stimuli, anxiety, or depressed mood and has a long-term impact on the psyche of the victim. They need expert counseling but are currently counseled by amateurs in the field.
Recommendations: The apex medical institutes must initiate focused research in the field and train a subset of psychiatrists and Clinical Psychologists in the field of PTSD. GoI may consider the establishment of Rehabilitation Centers focused on rehabilitating Trauma Victims with a broad mandate to interact with intergovernmental agencies.
-
To address the issue of financial compensation for the trauma care providers
Problem: Trauma victims, on many occasions, reach the emergency department as unknown’ and hence not in a position to pay for the services on arrival. However, the hospital is required to commit his resources immediately
Recommendations: The government has to develop a financial compensation policy for all trauma victims. This is because they constitute the largest share of preventable deaths all over the world and in a young earning population out on the road for work and leisure, thereby contributing to the nation’s economy. Unless this issue is addressed, victims of critical firearm injuries in civilian life will continue to die by and large.
-
To aim for a modern, well-equipped, well-networked ambulance service manned by ATLS-trained staff in all parts of India.
Problem: Most state governments and Municipalities in the last 10 years have made substantial progress in developing their Ambulance services, e.g., 108 Ambulance’ which are integrated with call centers and work 24 X 7 X 365 days, and this service is slowly progressing towards even Tier 2 towns, which is very encouraging. However, as a nation, we have a long way to go to make these ambulances capable of handling Blast and GSW injuries; as of now, these ambulances can, by and large, give oxygen and fluids and have facilities to provide CPR.
Recommendations: Most of the ambulance services are not geared up to treat bullet/BI. The emergency ambulance services are required to be fully equipped with a certified staff proficient in BLS and ATCN/ATLS. Similarly, the ambulances are required to be equipped with trauma care products like a tourniquets, hemostatic dressing, resuscitation equipment, needle thoracostomy, tube thoracostomy, spine stabilizers, volume expanders, modern splints, along with AI-based interactive help modules, and GPS enabled patient-friendly modern vehicle.
-
To introduce robust training in trauma care as part of the Medical, Nursing, and paramedical curriculum.
Problem: Medical, Nursing, or Paramedical curriculums do not provide structured training in Trauma care. Hence, doctors, nurses, and paramedics’ ability to manage bullet injuries is generally inadequate.
Recommendations: Basic management of bullet/ blast injury should become a compulsory element of all certificate programs, degrees, and diplomas in medicine, paramedical, and nursing education, with regular mandatory refresher training to maintain currency (online or offline or both in combination). ATLS for doctors and ATCN for Nurses and paramedics should become compulsory parts of the license to practice.
-
All out efforts to be made to reduce the availability of illegal firearms
Problem: Illegal manufacture of weapons, possession of illegal weapons as well as illegal usage of legal weapons is common in India, instilling fear and hesitancy in the mind of the general public. Whenever a citizen is forced to hold himself from his honest contribution towards his nation due to fear of certain elements of the society and those working covertly to weaken a nation’s will, that nation can never rise to its true potential. All policymakers must give very high importance to this matter and address it.
Recommendations: All-around efforts should be made to reduce the availability of illegal firearms. A license should only be given when one has attained age 25, provided one clears a well-organized psychological test assessed by an experienced psychologist and can provide a valid reason for its requirement. This should be a mandatory prerequisite in even applying for a license for firearms, with legal provisions to monitor the owner’s conduct in a continuum.
-
All trauma centers should be well-staffed with competent medics
Problem: Trauma centers should be managed by doctors, nurses, and paramedics with special trauma competence. This has been primarily diluted in most cancers due to the non-availability of an adequate number of fully qualified certified staff.
Recommendations: Formal education and specialty training in emergency medicine, trauma surgery, and critical care are desirable (but not mandatory) attributes for personnel involved in trauma care, but is a mandatory requirement to expertly handle the disruption of the body due to bullet/explosive since it involves a different dimension of anatomical and physiological avalanche where time is in premium, i.e., quality of intervention in the platinum 10 – 30 min decides the fate of 50% of victims. However, such training is unavailable at most Medical/Paramedical training institutes. This needs to be addressed using advanced trauma simulators in training and a one-year internship in a higher-level center.
-
Records held by all stakeholders in crime management must be integrated into a shared database
Problem: In India, various stakeholders concerned with bullet and BI, which constitute the maximum mode of crime, are not integrated.
Recommendations: It is suggested that all Police Stations, Medical Colleges, and District Hospitals where medico-legal postmortems are held and the associated Forensic lab, as well as the criminal courts, be integrated and a centralized database formed so that accurate, valid, and reliable data can be recorded. This may be considered a very critical repository of databases. All planning and policies can be made accurately if the integration is done correctly.
Acknowledgement
The contributions of all domain experts in trauma, surgery, medicine, and forensic medicine and the members of the Armed Forces of India are acknowledged. The support from the National Academy of Medical Sciences of India is also acknowledged. This document was made possible due to the collective effort of all stakeholders and their hard work over the last three months. I am sure this document will go a long way toward enhancing our nation’s capabilities in managing gunshot and BI.
-Sd-
Air Vice Marshal
Tanmoy Roy VSM
Chairman, NAMS-AFMS Joint Task Force
References
- Emerging trends of intentional firearm injuries in northern India: A Study. J Clin Diagn Res. 2016;10:HC01−HC04.
- [Google Scholar]
- Evaluation of complete profile and outcome of gunshot injuries in the tertiary care center. Int Surg J. 2019;6:397-402.
- [Google Scholar]
- There are no emergency medical services or prehospital care for the injured in Mumbai, India. Prehospital Disaster Med. 2010;25:45−151.
- [Google Scholar]
- Emergency and Injury Care at District Hospitals in India: A report on the current status of country-level assessment. A study conducted by Department of Emergency Medicine, JPNATC, AIIMS. 2020.
- Quality of services provided by public funded ambulance program: Experience from a northern state in India. CEGH. 2020;8:962−6.
- [CrossRef] [Google Scholar]
- Trauma care in India: current scenario. World J Surg. 2008;32:1613−7.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency medical services in India: the present and future. Prehosp Disaster Med. 2014;29:307−10.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma care in India and Japan: Current situation and future prospects. ERIA Research Project Report 2021
- [Google Scholar]
- Training in trauma management. Med J Armed Forces India. 2010;66:354−6.
- [CrossRef] [PubMed] [Google Scholar]
- Regulating the private health care sector: The case of the Indian Consumer Protection Act. Health Policy Plan. 1996;11:265−79.
- [CrossRef] [PubMed] [Google Scholar]
- Menon C, DH Web Desk. 2022. Available from: https://www.deccanherald.com/india/a-guide-to-indias-stringent-gun-laws-1102061.html [Last accessed 23 Jul 2024].
- Surgical response to the 2008 Mumbai terror attack. Br J Surg. 2012;99:368−72.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of the availability of technology for trauma care in India. World J Surg. 2015;39:363−72.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma care systems in healthcare facilities of an Indian district: Assessment and future directions. J Family Med Prim Care. 2023;12:567−75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Learning from 2523 trauma deaths in India- opportunities to prevent in-hospital deaths. BMC Health Serv Res. 2017;17:142.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trauma Care Programme. National Programme for Prevention and Management of Trauma and Burn Injuries (NPPMTBI). Available from: https://main.mohfw.gov.in/sites/default/files/Prog%20brief%20Trauma%20component%20.pdf [Last accessed 03 Aug 2023]
- Trauma care centers in Maharashtra deficient: CAG. Times of India. 2017. Available from: https://timesofindia.indiatimes.com/city/mumbai/trauma-care-centres-in-maharashtra-deficient-cag/articleshow/60022093.cms [Last accessed 03 Aug 2023].
- Guidelines for trauma quality improvement programmes (2009). World Health Organization, International Society of Surgery, International Association for the Surgery of Trauma and Surgical Intensive Care, editors. Available from: https://iris.who.int/bitstream/handle/10665/44061/9789241597746_eng.pdf?sequence=1 [Last accessed 23 Jul 2024].
- Cabinet approves the Policy for the Medical Devices Sector. Ministry of Chemicals and Fertilizers. 2023. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1919984 [Last accessed 23 Jul 2024].
- Mapping Murder (The Geography of Indian Firearm Fatalities). Small Arms Survey. 2011. Available from: https://www.files.ethz.ch/isn/143581/IAVA-IB2-mapping-murder.pdf [Last accessed 23 Jul 2024].
- Abdominal trauma after terrorist bombing attacks exhibits a unique pattern of injury. Annals of Surgery.. 2008;248:303-309.
- [CrossRef] [PubMed] [Google Scholar]




