Translate this page into:
NAMS task force report on Organ donation and transplantation
*Corresponding author: Dr. Y.K. Chawla: Chairperson, Former Director PGIMER, Chandigarh, Professor Emeritus Kalinga Institute of Medical Sciences, KIIT University, Bhubaneswar, India. Email: ykchawla@gmail.com; nams_aca@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: National Academy of Medical Sciences (India). NAMS task force report on Organ donation and transplantation. Ann Natl Acad Med Sci (India). 2024;60:71–87. doi: 10.25259/ANAMS_TFR_02_2024
INTRODUCTION
Organ transplantation gives a new lease of life to patients with end stage Organ failure. While in India, over the years living donors had been the primary source of kidneys for transplantation, the last decade and a half has seen live donors being the main source of livers also. However, there is a need to reverse this trend.
Almost 160,000 fatal road traffic accidental (RTA) deaths happen in India, and almost 60% have associated head injury (almost 90 per million possible brain deaths from RTA). Similarly, Cerebro Vascular Accident (CVA) is another common cause of BSD in India (prevalence rate of CVA ranging from 44.54 to 150 per 100,000 population) and 30 days case fatality rate ranging from 18% to 46.3%,1,2 and these are also part of deceased donor pool in our country. A large number of Organs from these patients could be harvested for transplantation.
The number of persons donating Organs after death in India is less than one per million population, which is almost similar to some Asian countries like Japan but far less than most Western countries. [In 2020, the United States and Spain had the highest rates of deceased Organ donors in select Organisation for Economic Co-operation and Development (OECD) countries, with almost 38 people per million population, whereas Greece (4.6), Russia (3.9), and Turkey (3) had the least donation rate].3
Surprisingly, according to an Ipsos survey in 2018 about people’s willingness to donate organs after death, Colombia and India, with 75% and 74%, respectively, had the highest percentage of willing people to donate organs after death, ahead of Spain (72%), UK (67%), and Germany (53%).4 This may be due to the campaigns undertaken by non-government organizations in the country. Mass media, religious, and political leaders may be involved to maximize awareness about Organ donation. Thirty-two percent of the study participants believe that there is a danger that donated Organs could be misused, abused, or misappropriated.5
Organ transplantation represents the final choice for life, as without a transplant, the patient will die. Thus, Organ transplantation is a field of medicine with extremely huge stakes. In this huge stake area, the transplant community should be constantly looking at mechanisms to boost the Organ supply. This also includes maximizing the utilization of brain deaths, diminishing the missed opportunities for donation, and also considering expanded criteria of donor Organ.
Barriers to donation: While the need for Organ donors is high in the Indian population, the actual number of donors remain low to help the number of recipients on the waiting list. Reluctance to donate Organs is not only within Indian borders but also extends to the Indian population in the UK and Canada.6
Societal issues: In certain regions of the country, there is less reluctance when it comes to donation in comparison to other regions. A study in north India found that the majority of individuals who were suffering from renal failure and on dialysis were unlikely to be an Organ donor since their families had not initiated any conversation on Organ donation. Such conversations play an important role in decision-making during consent. Many have been unaware of how to register, which means campaigns for Organ donation registration should be improved. Fear and mistrust are also the main roadblocks due to media news items appearing of illegal Organ donation and transplant practices. Body disfigurement was the least reason for Organ donation. Though no religion is against Organ donation, many donors use this as a reason for not giving consent. It was also found that nuclear families agreed more rapidly for Organ donation.7 In a survey from South India involving 300 participants to a questionnaire on Organ donation, less than half of the study participants were knowledgeable about the definition of brain death and the existence of organ donation law. Although they were in favor of organ donation, there were still some doubts related to family support.8
Hospital issues: A recently published study showed a lack of knowledge on clinical criteria for brain death and legal issues pre-intervention, which improved post-intervention, after they participated in an interactive educational module. This intervention significantly improved the tendency of doctors and nurses to promote Organ donation, pledging their Organs, and for counseling patients/attendants on this cause.9 There is no magic bullet to increase the Organ donation rates. Addressing donor shortages requires a multipronged strategy considering barriers to Organ donation as they manifest across a society.
Spain’s achievements of a high Organ donation rate are attributed to its systems in place and wide government support. It has a vast transplant coordination network of doctors and nurses specially trained in reporting and approaching family members for Organ donation. They also stress education/health care infrastructure and human resources, forming a multipronged approach that is tailored to develop transplants in that country.10
As part of a national network, the National Organ & Tissue Transplant Organization (NOTTO) and five regional organizations, namely Regional Organ & Tissue Transplant Organization (ROTTO) at Mumbai, Kolkata, Chandigarh, Chennai, and Guwahati cover Western, Eastern, Northern, Southern, and North-Eastern regions of the country, respectively, were established. It was envisaged to set up one State Organ & Tissue Transplant Organization (SOTTO) in each state, with 14 SOTTOS already sanctioned so far. These organizations integrate efforts of the states, institutions, healthcare professionals, non-government organization, and members of the community.
The National Organ Transplant Program was first conceived in 2011–2012 and its detailed guidelines entitled “Highlights of National Organ and Tissue Transplant Programme & Operational Guidelines for its implementation” were first published in 2015. After the inception of the program, the total number of Organ transplants in the country increased from 4990 in the year 2013 to 12,746 in the year 2019 and Organ donation rate (no. of deceased donors per million populations) increased from 0.16 in the year 2012 to 0.65 in the year 2018.
TERMS OF REFERENCE (TORS) FOR THE TASK FORCE
The Executive Council of the National Academy of Medical Sciences (India) assigned the following terms of reference for the Task Force on Organ donation and transplantation in April 2022.
To identify the current status of Organ donation and transplantation in India.
Identify the exact deficiencies.
To suggest and recommend ways of improvement in the area of Organ transplantation.
METHODOLOGY
The Task Force conducted meetings using a virtual platform and Focused Group Discussions were held. In addition, the Chairperson co-opted expert members as and when required to facilitate the discussions. The relevant technical documents, published papers, reports, like NOTP Guidelines and various State Guidelines, were used as background materials.
The key recommendations were arrived at by consensus of the members based on their expertise and experience.
BACKGROUND: HOW MANY TRANSPLANTS ARE CONDUCTED IN INDIA PER MILLION?
The current status of Organ donation and transplantation in India is shown in Figure 1–7:
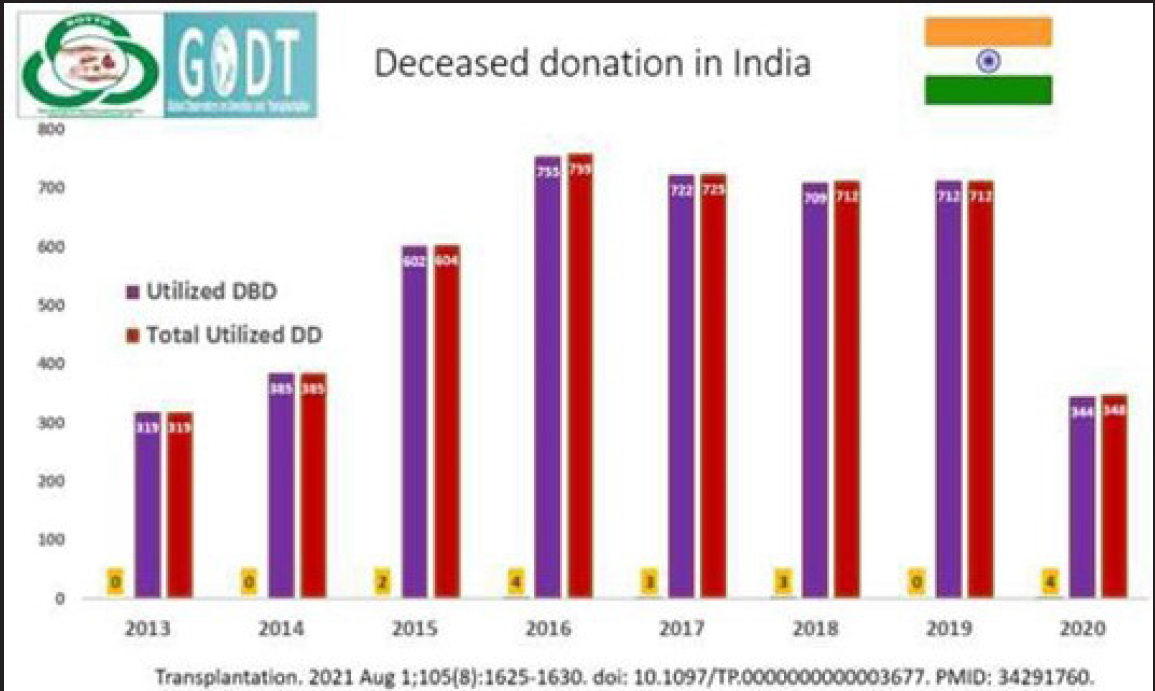
- DD: Deceased donor; DBD: Donation after Brain Death.
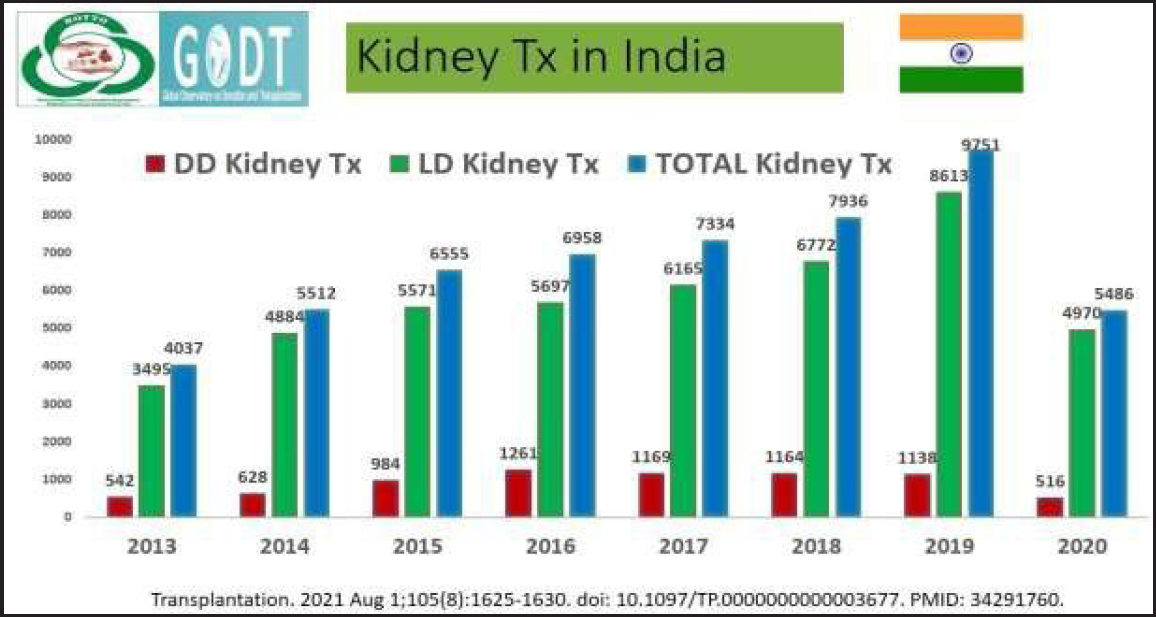
- DD: Deceased Donor; LD: Live Donor; Kidney Tx: Kidney transplant.

- DD: Deceased Donor; LD: Live Donor; Liver Tx: Liver transplant.

- Transplantations done from 2013 to 2020 of Heart, Lungs, Pancreas & small bowel.
- Tx: Transplant
Organ Deceased Donor Organ Donation & Transplantation (DDOT)
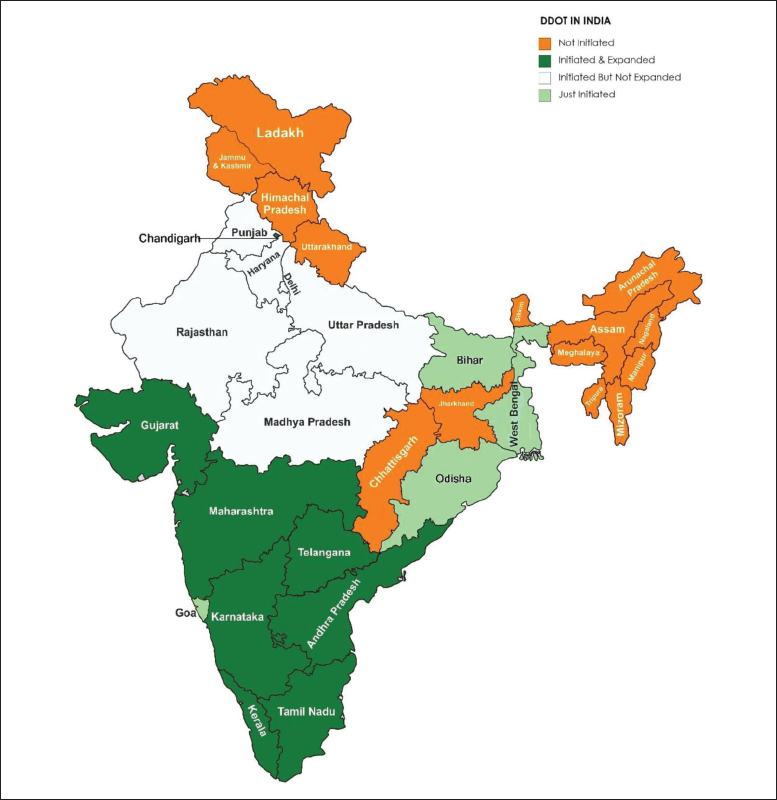
- States shown in green have well-established Deceased Organ Donation programs (dark green states) to expand DDOT in emerging states (light green, orange states).
Total Transplants in India (2020)
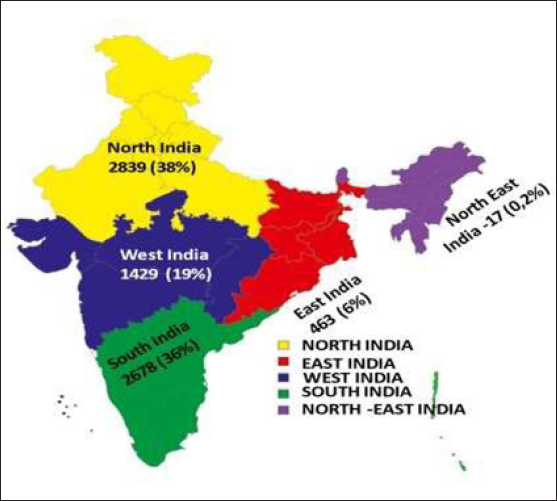
- Distribution of total transplantation in Different Regions of India 2020
Total Transplants in India (2021)

- Distribution of total transplantation in Different Regions of India
*2021 data is tentative (before submission to WHO-GODT 2021) as some of the states may make minor changes in their data.
Organ Donation Statistics
| Organ donation statistics | ||||
|---|---|---|---|---|
| 2020* | 2021** | |||
| Public | Private | Public | Private | |
| Deceased | 118 | 458 | 171 | 521 |
| Living | 492 | 4152 | 827 | 6029 |
| Total | 610 | 4610 | 998 | 6550 |
Data shared by NOTP
Note: Public facilities include Autonomous Hospitals and Private facilities include Trust Managed Hospitals.
**Data as per the survey conducted in January 2022 for 618 hospitals that are the part of National Registry.
OBSERVATION
Current situation in the country
About 160,000 deaths happen annually due to road traffic accidents in India – even if 10% (16,000) of these are converted as Organ donors, that will generate an average of 3 Organs per donor (as per Zonal Transplant Coordination Centre (ZTCC) Mumbai data), resulting in 45,000 Organ transplantations (livers, kidneys, hearts, lungs, pancreas, and small bowel).
CVA is another common cause of BSD in India, and these could also add to the deceased donor pool in our country (ZTCC Mumbai donor data).
The Organ donation rate (the number of deceased donors per million population) in the country increased from 0.27 in the year 2013 to 0.65 in 2018, however, it dipped to 0.52 in 2019. And are far less than compared to a maximum of around 48 in Spain.
There is an estimated need for 175,000 kidney and 50,000 each liver, heart, and lung transplants in India. 80% of kidney and liver transplants and 95% of heart, lung, and pancreas transplant services are in private hospitals where the cost is prohibitive for the common man with end-stage Organ failure.
Currently, it is estimated that only 10% of kidney failure patients get some form of renal replacement therapy (dialysis or transplant) due to the problems of access to tertiary care and financial constraints. However, the growth of healthcare and provision of dialysis facilities in all the 773 districts in the country by GoI, would mean a spurt in the patients requiring access to transplants.
India is the third country in the world after the USA and China, in terms of the total number of transplants done in a year.
The total number of transplants done in the country has increased from 4990 in 2013 to 12,666 in 2019, indicating a marked improvement in infrastructure for undertaking transplants in the country and this was mostly due to the growth of private healthcare.
Organ transplantation in India to date relies predominantly (80.3%) on living donor procedures for kidney and liver transplantation. Heart, lung, pancreas, and small bowel transplants are therefore less frequent.
Current infrastructure, facilities, technologies, policies, programs, etc. in the country in context of the problem/health issue
A total of 618 hospitals undertaking transplantation or retrieval in the country are now registered with NOTTO for networking and National Registry. This indicates significant progress in the establishment of an organized system in the country for Organ procurement from deceased donors and their distribution and transplantation to the needy citizens of the country. However, the data entry by the hospitals in the National Registry remains incomplete.
The number of persons who have pledged for Organ and/or tissue donation with NOTTO is now more than 1.4 million, out of which more than 300,000 have been registered online. This indicates a significant improvement in awareness about Organ donation.
Capacity for undertaking rare transplants, e.g., pancreas, intestine, hand, limbs, lung, and uterus has developed within the country, besides a significant enhancement in capacities for undertaking relatively common transplants of kidney, liver, and heart.
Some transplant centers, including PGIMER Chandigarh, have also developed capacities for undertaking donation after cardiac death.
Current budget
The following is the grant in aid under the National Organ Transplantation Program (NOTP) available for the promotion of Organ transplantation.

- ROTTO: Regional Organ & Tissue Transplant Organization; SOTTO: State Organ & Tissue Transplant Organization; TC: Transplant Coordinator
Summary of total budget for Organ donation and transplantation
(Tentative year-wise distribution for 2021–2022 to 2025–2026 as per proposed outlay in lakhs of rupees)
| S.No. | Component |
(2021–2022) Proposed outlay |
(2022–2023) Proposed outlay |
(2023–2024) Proposed outlay |
(2024–2025) Proposed outlay |
(2025–2026) Proposed outlay |
Total in Rs. (Lakh) |
|---|---|---|---|---|---|---|---|
| 1 | IEC Activities | 129 | 129 | 114 | 114 | 114 | 600 |
| 2 | National THOA and NOTP Cell | 25 | 40 | 45 | 45 | 45 | 200 |
| 3 | NOTTO including National Biomaterial Centee | 300 | 325 | 325 | 375 | 400 | 1725 |
| 4 | ROTTO and SOTTO (5) | 109 | 114.25 | 119.76 | 125.55 | 131.63 | 600.19 |
| 5 | SOTTO (20) | 450 | 480 | 534 | 588 | 600 | 2652 |
| 6 |
Bio-material Centers -3 at ROTTOs/SOTTOs |
100 | - | 100 | - | 100 | 300 |
| States at 100 lakh per center | |||||||
| 7 | Govt. supported online system of networking | 150 | 50 | 50 | 25 | 25 | 300 |
| 8 | Training | 50 | 75 | 75 | 100 | 100 | 400 |
| 9 | Skill center(s) | 50 | 50 | 50 | 50 | - | 200 |
| 10 | Support for immune-suppressants | 75 | 75 | 100 | 125 | 125 | 500 |
| 11 | Coordination with trauma centers | 10 | 10 | 10 | 10 | 10 | 50 |
| 12 | Coordination with govermentmedical colleges and good performing private centers | 50 | 50 | 50 | 75 | 75 | 300 |
| 13 | New retrieval/transplant facility and strengthening old transplant facility in government medical colleges/institutions | 200 | 300 | 200 | 200 | 200 | 1100 |
| 14 | Support for maintenance of Cadaversin retrieval centers at Rs. 100,000 per cadaver for 5 cadavers per year | 5 | 5 | 5 | 5 | 5 | 25 |
| 15 | Support for Organ transportation through ROTTO and NOTTO at 1 crore per year | 10 | 10 | 10 | 10 | 10 | 50 |
| 16 | Grant to cover expenses for dignified funeral of deceased donor (support of Rs. 10,000 to each donor family) | 40 | 50 | 60 | 70 | 80 | 300 |
| 17 | Outcome monitoring | 2 | 2 | 2 | 2 | 2 | 10 |
| 18 | International cooperation | 30 | 30 | 30 | 30 | 30 | 150 |
| 19 | Evaluation | 0 | 0 | 0 | 0 | 30 | 30 |
| Grand total | 1785 | 1795.25 | 1879.76 | 1949.55 | 2082.63 | 9492.19 |
Total Proposal for 5 years = 9492.19 Lakh = 94.92 Crore; data given by NOTTO.
THOA: Transplantation of Human Organs and Tissues Act 1994; NOTP: National Organ Transplantation Program; ROTTO: Regional Organ & Tissue Transplant Organization; SOTTO: State Organ & Tissue Transplant Organization; NOTTO: National Organ & Tissue Transplant Organization
KEY ISSUES/GAPS IDENTIFIED IN THE CURRENT SITUATION IN THE COUNTRY IN THE CONTEXT OF THE PROBLEM/HEALTH ISSUE
Deficiencies in the program
Lack of brain stem death identification, certification and maintenance of Organs for donation
Shortage of manpower in government as well as private hospitals.
Lack of infrastructure/suboptimal utilization of infrastructure in the government sector.
The provision of Non-Transplant Organ Retrieval Centers (NTORC) in the law has also not been optimally utilized.
Guidelines related to donation after circulatory death are lacking.
Non-utilization of the grant under various heads of the National Program.
There is a regional imbalance. The Organ donation should happen in all the regions and should not remain concentrated in any geographical region. This creates problems with equity and the allocation of Organs.
Manpower working in SOTTO/ROTTO is having additional charge of SOTTO/ROTTO so adequate time cannot be devoted to Organ donation-related activities. It would be better to have such posts on full-time basis to devote more time to Organ donation rather than just giving additional charge of SOTTO/ROTTO posts.
Recommendations made to bridge the critical gaps/deficiencies in this aspect
Brain death
There should be a uniform declaration of death with a mode of death being brain stem death (BSD)/cardiopulmonary death (circulatory death).
The declaration of “Brain Stem Death” should be made mandatory for all hospitals, both private and government. The THOTA Rules provide for the same, however, the rule is not being followed in letter and spirit.
The hospital staff in medical colleges, district hospitals, and other retrieval centers that have ICU and ventilator facilities should be trained in the concept of BSD. There should be regular training programs on BSD for staff from medical colleges, district hospitals, and major corporate hospitals.
All BSD certifying specialists should be registered with local authorities.
The procedure for the donation of Organs in Medico Legal Case (MLC) should be streamlined and nation/state wise SOPs to be made.
Monthly audit of BSD must be done regularly by the concerned SOTTOs. The data pertaining to the declaration of BSD should be online as well as re-certification process should have a mandatory review of the number of brain deaths identified and audit reports of such activities from the ICU.
Training of ICU staff in family conversation for end-of-life care should be regularly conducted. The number of trained staff in the ICU for end-of-life conversations should be introduced in a phased manner. SOP for donation procedure within the hospital should be a mandatory requirement for certification
Regulatory bodies
There are around 618 registered transplant centers and only 140 non-transplant retrieval centers. The retrieval centers must proportionally be increased by incentivizing them.
Registration of Non-Transplant Organ Retrieval Centers (NTORC): The process for registration of NTORCs should be simplified. The hub and spoke model can be followed with big hospitals as hubs and NTORCs as spokes. Registered transplant hospitals can be tied up with trauma centers. In fact, all the trauma centers in the country should be registered.
All the medical colleges and hospitals can be identified as NTORCs.
Written SOPs with clear guidelines regarding manpower and equipment requirements should be shared with these NTORCs.
Apex National Body: Empowered and robust NOTTO with more financial powers should be there to work in the field of Organ donation and transplantation.
The Appropriate Authority should be a designated senior official only handling Organ donation and transplant on a full-time basis.
Independent oversight committee with representation of Appropriate Authority (AA) & Apex National Body.
Monthly activities of NOTTO, SOTTO, and ROTTO should be notified on the website including future workshops.
The performance of SOTTOs should be assessed on a regular basis with a possibility of transfer if found unsatisfactory.
-
Hospitals and ICU:
Death audits
Monthly audits of death, including BSD must be done on a regular basis by the concerned SOTTOs to find out the missed opportunities and possible solutions. The data pertaining to the declaration of BSD should be reported online on a central NOTTO interface.
Training of ICU staff in family conversation for end-of-life care should be regularly conducted and made mandatory.
SOP for donation procedure within the hospital should be a mandatory requirement for certification.
-
Re-certification process for a transplant license should have a mandatory review of
-
○
Number of brain deaths identified and audit reports of such activities from ICU.
-
○
SOPs for Organ donation pathways.
-
○
Family conversation for end-of-life care workshops conducted.
-
○
The number of trained staff in ICUs for end-of-life conversations should be introduced in a phased manner. Re-certification should consider the performance in this aspect.
-
Grief counselors/Transplant coordinators
At least four existing staff in the hospitals can be identified, trained, and designated as transplant coordinators.
The transplant coordinators for deceased donor family counseling should be different from those handling transplant recipients.
Role of police
The police must designate nodal officers to coordinate Organ donation-related activities.
The investigating officers/station house officer of the police station under which the hospital falls should be directed to assist in Organ procurement as mandated in the THOTA Act.
The respective governments must be directed to instruct police chiefs to hold regular awareness meetings for all investigating officers/station house officers.
The police also need to be sensitized about the importance of Organ donation and medico-legal issues should be eased.
Education and training
Organ transplant units should be there in all medical colleges and All India Institute of Medical Sciences (AIIMS) institutions. Such units should have faculty with expertise in the field of Organ transplantation and at least should become Organ retrieval centers in the first phase and have a brain death certification committee wherever possible. Multi-organ retrieval teams should be available in all major hospitals.
State governments should identify one medical college in their state that can become a center for excellence as a multi-organ transplantation hospital to help with the training of manpower and growth of the program.
Advanced transplant centers should be there in all INIs with individual Organ subdivisions. These centers should have a common ICU so that it could be managed with less logistics and manpower. Specialized departments for cardiac, lung, and Hepato Pancreato Biliary (HPB) surgery, and liver transplants should be created in all INIs to enhance the seriousness of multi-organ transplants. Stress must be laid on the recruitment of people with passion in the field of Organ transplantation to give a fillip to the program.
Training related to Organ transplant and prospective donors after the declaration of BSD should be given to all concerned physicians/surgeons.
All postgraduates should be trained in BSD like they are being trained in BLS and ALTS regularly. It would increase awareness and strengthen the concept of BSD, and make the foundation strong.
More consultants should be systematically trained in the field of Organ transplantation.
Transplant Societies and non-government organizations could help in the training of ICU professionals and surgeons in multi-Organ transplants. The competence of the transplant surgeons and the team should be objectively assessed.
A letter from the Secretary of Health, Director General of Health Services (DGHS), or National Medical Commission (NMC) may go to different states and medical colleges to start donor action programs.
Trauma centers should be better equipped to handle brain deaths (ventilators, Arterial Blood Gas (ABG) machines, and other equipment). This would help in both saving lives and early identification of brain deaths.
Fellowships as well as short-term attachments should be available/started at transplant centers.
A pool of certified transplant surgeons must be created for capacity building in the field of Organ donation and transplantation.
The curriculum/training on BSD should be imparted to all residents, faculty, and nurse staff. Organ donation chapters should be included in the curriculum. Besides, public awareness should be increased.
Infrastructure
All medical colleges, district hospitals, and trauma centers should be actively involved in transplant-related fields.
INIs should have transplant departments for multi-organ transplants and have permission for fellowships training in transplant.
A dedicated Department of Intensive Care Medicine should be created in all medical colleges and major government hospitals.
Dedicated infrastructure must be created in the Public Sector for Organ Transplantation on lines of IKRDC-ITS Ahmedabad, ILBS New Delhi, and PGIMER: Chandigarh. Few ICU beds can be dedicated for Organ donation in government hospitals. In all INIs dedicated ICUs and HDUs should be made as per standard protocol. This will strengthen the infrastructure for Organ transplantation from the beginning and new AIIMS will have accountability for Organ transplantation.
To maximize the utilization of deceased Organs, particularly extended criteria Organs, a provision should be made to do machine perfusion of Organs and for that, a clause should be added in THOTA Rules 2014 or a circular should be issued by GoI.
Organ transplant units should be formed in all medical colleges and AIIMS-like institutions. At least they should become Organ retrieval centers in the first phase and have a brain death certification committee. Such units should have faculty with expertise in the field of Organ transplantation and plan to have multi-organ retrieval team in all major hospitals.
Separate departments for multi-organ transplantation need to be created in one medical college of each state to promote Organ donation and transplantation. Advanced transplant centers should be there in all INIs with individual Organ subdivisions. These centers should have a common ICU so that it could be managed with less logistics and manpower. Departments of HPB Surgery & Liver Transplant and Department of Hepatology should be created in all INIs to enhance the seriousness towards liver transplant. The same should be adopted for other Organs as well. Stress must be laid on the recruitment of people with passion in the field of Organ transplantation.
| Challenges | Solutions for Deceased Donor Organ Transplantation (DDOT) in India |
|---|---|
| Awareness |
|
| Grief counseling |
|
| Brain Stem Death (BSD) declaration |
|
| ICU Team |
|
| Registry, Allocation, Transplant Team |
|
| Nonfinancial incentives |
|
| Collaboration, Advisory Committees |
|
| Expand DDOT in Public Sector Hospitals |
|
| Training, Capacity building |
|
| Audit |
|
| Future |
|
DDOT: Deceased Donor Organ Donation & Transplantation; NOTTO: National Organ & Tissue Transplant Organization; ROTTO: Regional Organ & Tissue Transplant Organization; SOTTO: State Organ & Tissue Transplant Organization.
NOTTO and financial aspect
The Government of India has earmarked funds for setting up a transplant center but this needs to be widely publicized and centers pushed to accept these funds with financial accountability. The fund utilization in this field is sub-optimal.
The grant allocated for various components should be visible at the level of NOTTO, ROTTO, and SOTTO. There should be a separate finance officer at the national or regional level for the grant and processing of the payments.
NOTTO could be made more robust by recruiting new officers with varied backgrounds like finance, etc. and SOPs should be made for the use of grants allocated for various components under NOTTO.
A full-time designated official in top positions (at NOTTO, ROTTO, and SOTTO) with a keen interest in Organ transplantation and donation should be appointed. Lateral entry for suitable candidates with experience in the field should be allowed with no age bar.
Audit should be conducted at the level of NOTTO to evaluate the work done by ROTTO and SOTTO and they should be made accountable.
There is an urgent need to make Organ donation and transplantation affordable. Drugs like immuno-suppressants, preservative solutions for Organ transportation, and other consumables required for Organ transplantation should be made tax-free.
The inclusion of Organ transplantation under Ayushman Bharat PMJAY by GOI is a good step and financial support from corporates through Corporate Social Responsibility and Crowd Funding should be encouraged for poor patients. The post-transplantation expenditure should also be taken into account.
States that have not adopted Transplantation of Human Organs and Tissues Act 1994 (THOA) should be requested to do so. Letters from Director Genertal of Health Services (DGHS) enumerating all funds should be sent to all state Directorate of Health Services (DHS) for setting up SOTTO in their states and registering all licensed transplant centers and retrieval centers. Enhancement and improvement of the National Registry into computerized data collection and automatic computerized allocation to have a transparent allocation.
Incentives to hospitals – who provide complete data to health authorities such as SOTTO/NOTTO.
·Regular meetings by AA for reviewing the progress from time to time of SOTTO/ROTTO and NOTTO.
Regional Directors of the Government of India Health and Family Welfare should be involved in facilitating the operationalization and implementation of various schemes of NOTP.
Greater involvement of the neuro critical care team of hospitals to enhance donor identification and Organ donation. They may be the preferred nodal officers of the hospital for all Organ donations and transplant-related matters.
Conferences of these specialties should have a session on Organ donation and transplantation.
Annual conferences should be organized by NOTTO/ROTTO/SOTTO and widely published.
National THOTA and NOTP Cell
It has the role of representing and renewal of all Organ and tissue transplant centers and monitoring transplants and retrieval in respective states and UTs.
Give consultancy on transplant law and program-related matters.
Facilitating National Organ Donation/World Organ Donation Day.
Looking after technical, administrative, and financial matters of NOTP, implementation and monitoring of its various components.
Organ transportation
Organ transportation by air can be taken up as a Corporate Social Responsibility (CSR) by corporates, the Indian Airforce can be involved in addition to the Ministry of Civil Aviation. Organ transportation by drones can also be considered.
Facilities for Organ transportation by road/air ambulances should be available at subsidized rates.
Tissue donation
Tissue donation has to be promoted. The tissue donation needs to be looked at by an independent Apex Technical Committee constituted for this purpose.
Best practices
Best practices from state Government Orders (G.O.) to facilitate deceased organ donation may be compiled and evaluated, and later adopted based on merit.
A modified The United Network for Organ Sharing (UNOS) model has been in practice in Maharashtra for over 20 years should be looked into and implemented.
Recommendations made to bridge the critical gaps/deficiencies in this aspect in THOTA rules of 2014
Current problem in Form 13: The requirements for infrastructure and manpower are almost similar to those for registration of a transplant center. There is no need to change Form 13 for recognition of NTORC. There is a need to simplify the process and a MoU can be signed.
All BSD certifying specialists should be registered with local authorities.
If there is a deceased donor in a non-registered hospital and the family is willing to donation of Organs and or tissues, then “In such non-registered hospital the death will be certified by two certified specialists from the registered transplant hospital or NTORC and retrieval of Organs and tissues can be done at the same hospital by teams from registered transplant hospital or shifted to a registered NTORC or transplant hospital”. In such cases, donor-specific/time-specific permission by Appropriate Authority may be granted when the family comes forward to donate the Organs.
Alternatives/Ancillary tests to Apnea test. BSD certification in a person where either:
Apnoea test cannot be done due to hemodynamic instability or
Cranial nerve reflexes cannot be tested due to eye/facial injuries, where actions to be taken.
Use ancillary tests to document the absence of cerebral blood flow as per international practices: BSD certifying specialist to decide the tests to be performed e.g., 4-vessel cerebral angio/CT cerebral Angio/MR angio/Trans Cranial Doppler/Isotope scan, depending on availability of facilities.
Any other
In all cardiac deaths, the option of tissue donation should be offered.
Role of digitization: the digitization of the Organ Donation Registry to avoid man-made errors.
24-hour call center at NOTTO.
Tree plantation drives in the name of donors and other ways to honor their families.
Awareness in schools and colleges on Organ donation.
National Health Insurance for Organ Transplantation.
Orientation and sensitization of various stakeholders like judges, legal experts, police, and traffic personnel, etc. on Organ donation and transplant centers.
WAY FORWARD
It is a well-known fact that Non Governmental Organisation (NGO) in the past have played a pivotal role in the promotion of eye and blood donation. An inclusive working group is required to be created from all regions to include all the stakeholders from both public and private bodies including medical societies such as Indian Society of Organ Transplantation (ISOT) and NGOs.
Increasing awareness:
More full-time manpower and budget should be allocated to NOTTO and NOTP.
Creation of modified UNOS model of Organ Procurement and Transplantation Network (OPTN) and Organ Procurement Organisations (OPOS) as being practiced in Maharashtra (ZTCCs) having financial self-sufficiency to be looked into.
There is a need to increase awareness about Organ transplantation among medical professionals.
Awareness posters about Organ donation should be installed at all hospitals (trauma center and ICU) and prominent places (such as shopping malls, railway stations, government offices, and banks). The “Ang Daan Jeevan Daan” posters having toll-free numbers should be installed at important places in all hospitals.
If any Organ donation and transplantation is being performed, such an event may be displayed on LED or as a blinking light on dashboards at NOTTO, ROTTO, SOTTO offices, and other prominent places to sensitize the public at large.
There should be a provision in the driving license about willingness to donate Organs in all states.
Smart cards should be issued to Organ donors.
Key actions
Adoption of THOTA by states who have not accepted as yet.
Establish SOTTO in each state to develop an effective and organized system of Organ procurement.
Govt institutions – augment infrastructure for Organ donation and transplant (identify medical colleges without infrastructure).
Register all trauma centers as Organ retrieval centers.
Have transplant coordinators in each hospital.
Make intensivists and critical care doctors as Nodal officers.
Creation of independent AA in each state.
Reporting of long-term transplant recipient and donor outcomes to NOTTO should be mandated.
Organ transplantation from deceased donors after cardiac death is underutilized in India and should be promoted.
ACKNOWLEDGMENTS
The contributions made by various domain experts in the field of “Organ” donation and transplantation, NOTTO, Ministry of Health & Family Welfare Government of India (GOI), and the support provided by the National Academy of Medical Sciences (India) and MOHAN Foundation are acknowledged.
OPERATIONAL DEFINITION OF TERMS USED IN THE REPORT
Brain stem death: Transplantation of Human Organs and Tissues Act (THOTA) defines brain stem death (BSD) as “the stage at which all functions of the brain stem have permanently and irreversibly ceased” and is so certified under Section 3 (6) of the Act. The BSD can be certified only by a board of Medical experts nominated from the panel of names approved by the Appropriate Authority (AA).
Circulatory death or cardiac death: Irreversible cessation of circulatory and respiratory functions.
Deceased donation: Organ donation by an individual who has been certified as deceased either due to brain stem or cardiac death.
Living donation: Organ donation by a living donor is generally limited to renal and hepatic donation.
Organ transplantation: This involves a surgical procedure to implant Organs or composite tissue from the donor into a recipient. Not all donations result in actual transplantation.
Organ procurement process: This involves:
Identification of potential BSD patient in ICU, family counseling about the criticality of the clinical situation by treating clinicians and intensivist, followed by confirmation of BSD by the expert clinical team as per the THOTA, discussion with family about Organ donation by clinicians and transplant coordinator and seeking consent for Organ donation from the family of a deceased individual. Communication with local Organ Distribution Organizations in the state for organ allocation to recipients as per the organ-specific allocation guidelines.
Organ retrieval, preservation, and transportation: This involves a surgical procedure of retrieving various Organs, their cold preservation, and transportation to transplant centers.
LIST OF ABBREVIATIONS
THOTA: Transplantation of Human Organs and Tissues Act, 1994
NOTP: National Organ Transplant Program
NOTTO: National Organ & Tissue Transplant Organization
ROTTO: Regional Organ & Tissue Transplant Organization
SOTTO: State Organ & Tissue Transplant Organization
DDOT: Deceased Donor Organ Donation & Transplantation
WHO-GODT: WHO Global Observatory on Donation and Transplantation
TC: Transplant Coordinator
NTORC: Non-Transplant Organ Retrieval Centers
BSD: Brain Stem Death
MLC: Medico Legal Case
AA: Appropriate Authority
IKDRC-ITS: Smt. G.R. Doshi and Smt. K.M. Mehta Institute of Kidney Diseases and Research Center and Dr. H.L. Trivedi Institute of Transplantation Sciences (IKDRC-ITS), Ahmedabad
PMJAY: Pradhan Mantri Jan Arogya Yojana
CSR: Corporate Social Responsibility
INI: Institute of National Importance
UNOS: The United Network for Organ Sharing
ZTCC: Zonal Transplant Coordination Centre
DCD: donation after circulatory death
ILBS: Institute of Liver and Biliary Sciences, New Delhi
PGIMER: Postgraduate Institute of Medical Education & Research, Chandigarh
GOI: Government of India
REFERENCES
- Barriers towards deceased organ donation among Indians living globally: An integrative systematic review using narrative synthesis. BMJ Open. 2022;12:e056094.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Burden of stroke in India during 1960 to 2018: A systematic review and meta-analysis of community based surveys. Neurol India [serial online]. 2021;69:547-559. [accessed 2022 Aug 2]. Available from: https://www.neurologyindia.com/text.asp?2021/69/3/547/317240
- [CrossRef] [PubMed] [Google Scholar]
- Organ transplantation number worldwide 2020 – Available from: Statista https://www.statista.com, State of Health
- Organ Donation: Where are the Most People Willing? HEALTH by Martin Armstrong, Sep 6, 2018. Available from: https://www.statista.com, State of Health
- Deceased Organ donor rate in selected countries 2020; Health, Pharma & Medtech, State of Health Published by John Elflein, Oct 4, 2021.
- Registration for deceased organ and tissue donation among Ontario immigrants: A population-based cross-sectional study. CMAJ Open. 2016;4:E551-E561.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Awareness and beliefs towards organ donation in chronic kidney disease patients in western India. J Nephropharmacol. 2015;4:57-60.
- [PubMed] [PubMed Central] [Google Scholar]
- Knowledge attitude & perception on organ donation among undergraduate, medical & nursing students at a tertiary care center hospital in some other part of India: A cross sectional study. J Educ Health Promo. 2019;9:161.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of international strategies in modulating knowledge & attitude of health care professionals for promoting organ donation. A study in a tertiary care hospital in North India. Ann Neursui. 2020;27:242-58.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- How Spain reached 40 deceased organ donation per million population. Am J Transpl. 2017;17:1447-54.
- [CrossRef] [PubMed] [Google Scholar]




