Translate this page into:
A review of the adverse impacts of allergic rhinitis on health-related quality of life and its evaluation
*Corresponding author: Sheetal Ajit Patil, Department of Homeopathic Materia Medica, Bharati Vidyapeeth (Deemed to be University) Homeopathic Medical College and Hospital,Pune-Satara Road, India-411043. Email: sheetal.patil@bharatividyapeeth.edu
-
Received: ,
Accepted: ,
How to cite this article: Srivastava P, Patil SA. A review of the adverse impacts of allergic rhinitis on health-related quality of life and its evaluation. Ann Natl Acad Med Sci (India). 2024;60:131–8. doi: 10.25259/ANAMS-2023-9-2-(1024)
Abstract
It has been proven that successfully treating allergic rhinitis (AR) with non-sedating antihistamines, intranasal corticosteroids, and other widely used, approved treatments results in improvements in health-related quality of-life questionnaires by incorporating health-related quality of life measures in clinical trials. Analyze therapeutic modalities that provide reliable and practical solutions to minimize the effects of this illness. The effects of AR on people’s health and quality of life should be examined by doctors. Better patient-provider communication and a deeper comprehension of AR may help with the treatment of this illness.
Keywords
Allergic rhinitis
Burden of illness
Impact on life
Quality of life
INTRODUCTION
Respiratory allergies are a common chronic issue that affects children’s breathing in the United States. Today, respiratory allergies are fairly frequent, yet they were not even recognized a century ago. At that time, the term “allergy” did not exist. Only one in seven Americans in 1950 were allergic to their respiratory system.1 In 1871, a Scottish physician by the name of C.H. Blackley made the initial discovery that plant pollen-induced hay fever; nevertheless, he is not well known in the medical field.2 Grant L. Selfridge, another physician, practiced homeopathy, or the use of natural treatments for illness. He was one of the American Academy of Allergy’s founders. In the west of the United States, he was the first to examine flora and pollen.3 According to homeopaths, using a substance that produces the same symptoms as the sickness is the best approach to treat it. Although some modern allergy medications function in a similar way, mainstream medicine does not give homeopathy enough credit.4 Allergic rhinitis (AR) has become more common in the United States and across the world.5 The Allergies in America, Allergies in Latin America, and Allergies in Asia-Pacific surveys, as well as the Pediatric Allergies in American questionnaires, were developed by physician experts in the field of AR in collaboration with Abt Schulman, Ronca, and Bucuvalas, a national public opinion research organization. The survey in the United States was performed entirely by random digit dialing, whereas the survey outside the United States was conducted through either a telephone interview or an in-person interview.6 Over the last three to four decades, high-income nations have experienced an allergy epidemic, with roughly one in every four children diagnosed with AR. The Indian subcontinent is additionally experiencing a rise in AR and asthma in the last 2 decades. India has one of the greatest concentrations of air pollution in the world due to biomass, fossil fuels, and automotive exhausts, and the usage of mosquito coils, incense, and dhoop sticks is a major source of interior pollution.7
Allergic rhinitis
Allergic rhinitis is a problem that makes the nose react to things in the air that some people are allergic to. It can affect many people around the world. It happens when some cells in the nose get inflamed because of the immune system. AR is caused by a mix of genes and environment.8,9 Some of the signs of AR are runny nose, stuffy nose, sneezing, and itching. AR can also cause other issues, such as asthma, sinus infections, and eye allergies. It can make people’s lives more difficult by interfering with their social lives, learning, employment, and sleep.9,10 AR is classified into two types: seasonal and permanent. Plants emit pollen at specific periods of the year, resulting in seasonal AR. Persistent AR occurs when people are allergic to objects in the environment, such as animals, dust, mold, or chemicals.11
Epidemiology
Prevalence
To accurately quantify the prevalence of AR, it is necessary to differentiate it from other types of rhinitis caused by different factors, such as infections or non-allergic triggers. Between 1990 and 2010, the European Community Health Survey (ECRHS) and the International Study of Asthma and Allergy in Childhood (ISAAC) conducted two large-scale international surveys that investigated the prevalence of allergic diseases among adults and children in various parts of the world. According to the Phase III International Study of Asthma and Allergies in Childhood (ISAAC), the prevalence of AR ranged from 0.8% to 14.9% in children aged 6–7 years and from 1.4% to 39.7% in children aged 13–14 years.12 According to one Indian study, the incidence of AR was 11.3% in children aged 6–7 years and 24.4% in children aged 13–14 years. In contrast to the high incidence of rhinitis, asthma, and eczema found in the ISAAC research, food allergy was shown to be low at 0.14% among Indian children aged 6–11 years.13 In India, common aeroallergens associated with AR and asthma include home dust mites, cockroaches, pollen, and mold spores. In India, there are two pollen seasons: tree pollen (February–April) and grass pollen (September–December).14 Almost 77% of the Indian population is exposed to PM25 levels that exceed the 40 g/m3 limit established by the National Air Quality Standards in India (the WHO standard is 10 g/m3).15 According to the third wave of the US National Health and Nutrition Examination Survey, which was conducted from 1988 to 1994, nasal symptoms were most common (30%) among people aged 17 to 29, and least common (10%) among people over 60. Since the 1960s, the global trends of atopy (the predisposition to develop allergies due to IgE antibodies produced by environmental or hereditary factors) and AR have shown a considerable increase.16,17 While the global prevalence of allergy illnesses is claimed to be 20%–30%, statistics for the general population and working people in Hong Kong, Malaysia, the Philippines, Singapore, Thailand, and Vietnam (together referred to as Asia) are sparse. According to the World Allergy Association, the total prevalence rate of AR, the most prevalent allergy illness in Asia Pacific (APAC), is 10%–30%, which is similar to the global average.18 This condition affects a vast number of people in Asia, ranging from 27% in South Korea to 32% in the United Arab Emirates.19
Pathophysiology
How rhinitis happens
Rhinitis is a problem that makes the nose inflamed and irritated. It can be caused by different things, such as allergies or other factors, or a combination of both. Depending on what causes rhinitis, the nose can have different symptoms. Each type of rhinitis has its own way of making the nose react. Allergic rhinitis only happens to people who have a genetic tendency to be allergic to some things.20 When these people are exposed to things they are allergic to, such as dust or pollen, their immune system makes special cells called B cells and plasma cells. These cells produce specific IgE antibodies that can recognize the allergens. IgE antibodies attach to some receptors on other cells called basophils and mast cells. When the allergens come in contact with the IgE antibodies, they trigger the basophils and mast cells to release or make chemical substances that cause allergy symptoms.8,12,20,21
Early-phase reaction
The early-phase reaction is what happens when the mast cells break down and release a lot of substances after the IgE antibodies that are specific to an allergen, are made and linked together on the surface of the mast cells. One of these substances is histamine, which is the main cause of AR. Histamine activates some nerve endings in a nerve called the trigeminal nerve, which is part of the fifth cranial nerve. This makes the person sneeze a lot. Also, histamine and other substances make the blood vessels in the nose expand and leak fluid, which causes nasal congestion and runny nose.22
Late-phase reaction
The late-phase reaction is another thing that can happen after the person is exposed to the allergen. It usually starts 4–6 h later and can last for a whole day. It often comes after the early-phase reaction, but it can also happen by itself. The late-phase reaction makes the person have more symptoms, such as a long-lasting runny nose, sneezing, and stuffy nose. The late-phase reaction is mainly caused by inflammation, which is when the body tries to fight off the allergen. Inflammation brings more cells to the nose, such as basophils, eosinophils, and T lymphocytes. These are cells that are part of the immune system and help with allergies. Mast cells also make and release more substances, such as IL-4 and IL-13, which are types of cytokines and chemokines. These are molecules that help communicate between cells and coordinate the late-phase reaction [Figure 1 and Table 1].23,24
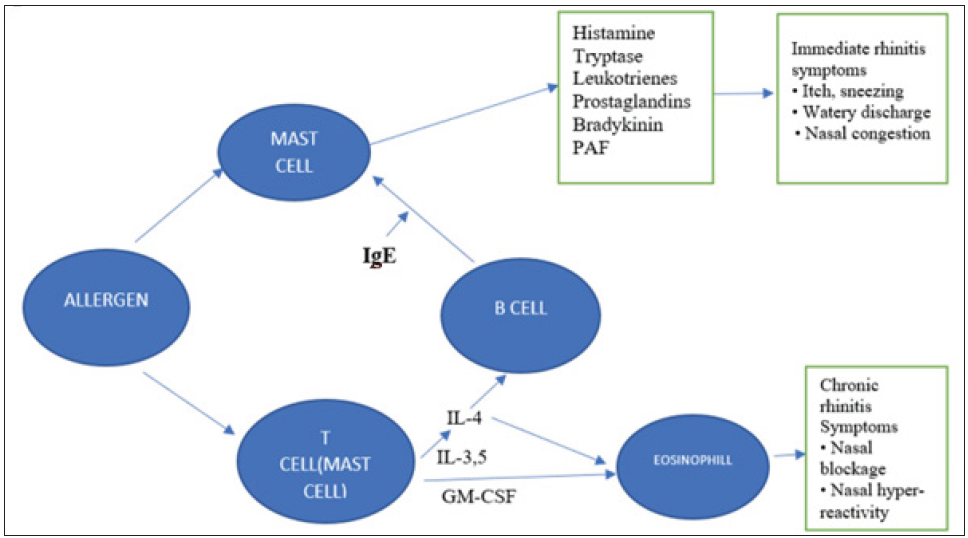
- Mechanism of AR. PAF: Platelet Activating Factor, IgE: Immunoglobulin E, GM-CSF: Granulocytic-macrophage colony-stimulating factor, IL: Interleukins.
| Trigger types | Origin/specific example of trigger | Type of rhinitis caused |
|---|---|---|
| Mites | House Dust Mite, Storage Mites, Allergen in Mite Fecal Pellets | Major Causes of Perennial Rhinitis |
| Pollens | Trees, Grasses, Shrubs, Weeds | Main Causes of Seasonal Rhinitis; Cross-Reactivity Among Pollens |
| Animals | Cats, Dogs, Horses, Mice Rats and Saliva |
• Allergen In Sebaceous Glands • Allergen Mainly in Urine |
| Fungi | Altemaria, Cladosporium, Aspergillus |
Seasonal And/or Perennial Symptoms • Reversible With Early Diagnosis and Avoidance but Becomes Chronic and Irreversible If Exposure Is Prolonged. |
| Occupational Induced | Flour, Latex, Laboratory Animals, Wood Dust, Enzymes, Other Airborne Proteins | • May Progress to Asthma.Diagnosis Based on Symptom Diary Cards and Provocation Tests. |
| Occupation Aggravated | Smoke, Cold Air, Formaldehyde, Sulphur Dioxide, Ammonia, Glues, Solvents, etc. | Pre-Existing Rhinitis Can Be Aggravated by Work-Place Irritants |
Impact of allergic rhinitis on health-related quality of life
When a person has AR, it can affect their quality of life. This means how they feel about their health and happiness in different areas of their life.25 Quality of life is not just about physical health but also about mental and emotional health and how the person interacts with others. The World Health Organization defines quality of life as “the way people perceive their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns”. Both good and bad things that happen to a person’s health might have an impact on their quality of life.26,27 A person’s quality of life may vary if they have an illness like AR. The term “health-related quality of life” (HRQOL) refers to this. It refers to how the patient believes their illness and its treatment impact their daily lives, well-being, and physical, mental, and social well-being. According to Settipane, AR might worsen a person’s HRQOL if it is not adequately treated. Not getting enough sleep, feeling exhausted during the day, struggling to study, having difficulties thinking properly, and performing poorly at work or school are some of the symptoms that can cause this.28 In a study of 3052 patients, the intensity and duration of AR were analyzed, and it was determined that 11%, 8%, 35%, and 46% of the patients, respectively, had intermittent mild forms, persistent mild forms, intermittent moderate-to-severe forms, and persistent moderate-to-severe forms. More than 80% of patients with more severe forms reported impairment in their activities as a result of the condition, compared to just 40% of those with moderate forms.19
Measurements of health-related quality of life
Utilizing questionnaires that probe the respondent on several facets of their health and well-being is one technique to gauge quality of life.29 These questions can assist in determining how a person’s social environment and way of life influence their daily activities. The questionnaires may include questions regarding the respondent’s performance at work or school, their level of productivity, their self-esteem, and their health. When a person has rhinitis and receives therapy for it, some of these things may change. A variety of questionnaires are available for measuring HRQL. They range from being general to being specialized.30,31 For various illnesses and health issues, general questionnaires might be employed. They can assist in comparing how various illnesses impact a person’s quality of life. They can also assist in identifying the primary health problems in a community and providing solutions.30 The Short-Form Health Survey (SF-36) is one of the most well-liked and trustworthy general questionnaires. It was created by a team of scientists known as the Medical Outcomes Study. A total of 36 questions are included, and they cover three crucial aspects of health: how the individual feels, how they function, and how they handle their medical issue. Numerous disorders, including AR, have been studied using it [Table 2].26,30,31
| Standard | Count of things | Explanation |
|---|---|---|
| Functional Status | ||
| 1. Physical Functioning | 10 | Extent To Which Health Interferes with A Variety of Activities (E.G., Sports, Carrying Groceries, Climbing of Stairs, and Walking) |
| 2. Social Functioning | 2 | Extent To Which Health Interferes with Normal Social Activities (E.G., Visiting with Friends During Past Month) |
| 3. Role Limitations Attributed To Physical Problems | 4 | Extent To Which Health Interferes with Usual Daily Activities (E.G., Accomplished Less Than Would Like) |
| 4. Role Limitations Attributed To Emotional Problems | 3 | Extent To Which Health Interferes with Usual Daily Social Activities (E.G., Accomplished Less Than Would Like) |
| Wellbeing | ||
| 5. Mental Health | 5 | General Mood or Affect, Including Depression, Anxiety, and Psychologic Well-Being During the Past Month |
| 6. Energy/Fatigue | 4 | Tiredness, Energy Level |
| 7. Pain | 2 | Extent Of Bodily Pain in Past 4 Weeks |
| Overall evaluation of Health | ||
| 8. General Perception of Health | 5 | Overall Rating of Current Health in General |
| 9. Change in Health | 1 | Evolution Of General Protection of Health |
Specific questionnaires are created to assess a specific patient population (such as children), a specific function, or a specific condition, and they may be more sensitive because they include questions that are only applicable to certain diseases [Table 3].32
| Instrument | Type | Patient |
|---|---|---|
| SF-36 Health Survey | Generic | Adults |
| Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ) | Disease-specific | Adults |
| Rhinitis Quality of Life Questionnaire | Disease-specific | Adults |
| Adolescent Rhinoconjunctivitis Quality of Life Questionnaire (ARQLQ) | Disease-specific | 12-17 Y |
| Paediatric Rhinoconjunctivitis Quality of Life Questionnaire (PRQLQ) | Disease-specific | 12-17 Y |
| Rhino sinusitis Disability Index | Disease-specific | Adults |
| PAR-ENT Quality of Life Questionnaire | Disease-specific | Adults |
Burden of physical symptoms
In 2006, a big research project called Allergies in America was completed. It was the first time that a large group of people with nasal allergy symptoms were studied in detail. It was also the biggest study of its kind ever done.33 The results of the Allergies in America research showed new things about how AR affects the way people think and act. They also showed that AR is not a minor problem but a serious one. Most of the people who had nasal allergies (two out of three) said that AR made their daily lives harder in some way. And four out of 10 people said that AR had a big or medium impact on their lives [Figure 2].33
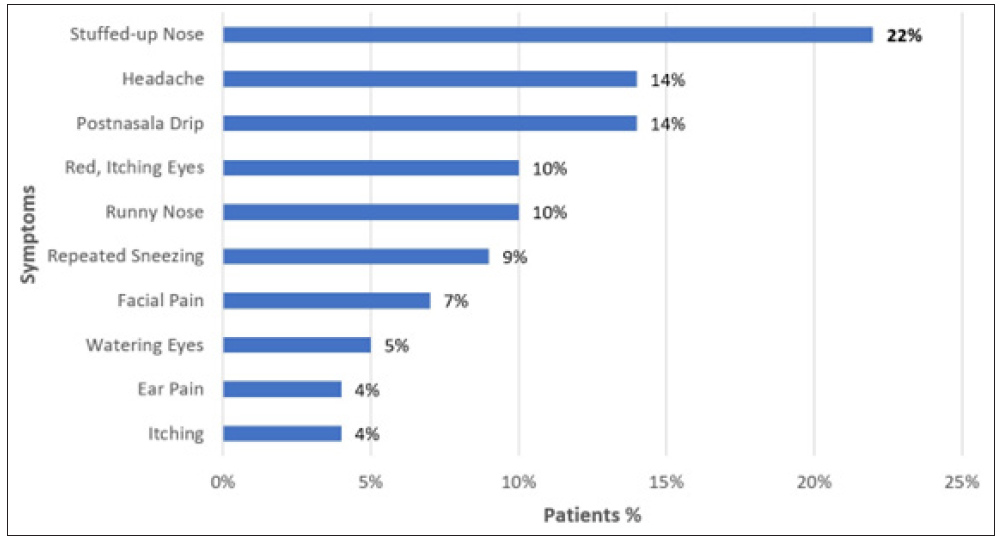
- The most bothersome symptoms of nasal allergies.
Burden on patient emotions
People with AR were questioned how they felt about their quality of life during allergy season as part of the Allergies in America study. They might respond with words that express their feelings.33 Other research 34, 35 also investigated how AR impacts the mental health of those who have it. They discovered that adolescents with AR (aged 11 to 13) experienced higher emotional difficulties than those without AR. Additionally, they discovered that adolescents with AR were more likely to experience physical discomfort, worry, despair, and rage. They also struggled more with remaining calm under pressure, restraint, and impulse control. These negative feelings were stronger in young people than in adults who had AR.35
Burden on work activities
A person’s performance at work or in school might also be impacted by AR.26 People with AR are less able to work than they would be if they did not have it. Due to their symptoms, they can also skip work or school more frequently. The degree to which AR impairs academic or professional performance can be accessed via a questionnaire, which is named as Job Productivity and Activity Impairment-Allergy Specific Questionnaire. The individual is questioned about how their allergies impair their participation in job or school activities. Estimating the financial costs associated with AR and the types of therapies required can also be helpful.26,36 Professional activities have been observed to be impaired in up to 60% of seasonal AR patients and 40% of permanent AR patients [Allergic rhinitis: indicators of quality of life*]. It has been estimated that 50% of people who use first-generation antihistamines (sedatives) to treat the condition operate at just 75% of their complete capacity for 14 days each year.37
Sleep impairment
Sleeping issues are one of the issues that persons with AR may experience. They may experience breathing difficulties as a result of a plugged nose.38 Numerous studies have demonstrated that those who have AR do not sleep as well as those who have not. They could struggle more to get to sleep, stay asleep, or feel relaxed. According to the Burden of Allergic Rhinitis study, those with AR had higher scores on the scales measuring sleep issues and adequate sleep than those without the condition. These are indicators of the quality of the sleep, either excellent or terrible. Microarousals during sleep may also be more frequent in those with AR. These are the fleeting moments when someone is somewhat startled out of sleep by anything. These disruptions may be brought on by breathing issues, increased nasal discharge, or increased upper airway resistance in persons with AR. In other circumstances, these microarousals might occur up to 10 times more frequently.38,39 A person’s thoughts and feelings may change if they are not getting enough sleep. They may be less able to focus, recall information, or come up with solutions as a result. Additionally, it may increase their risk of developing mental health issues, including despair, anxiety, or alcohol abuse. In an AR survey, 68% of people with perennial AR and 48% of those with seasonal AR said that the condition interfered with their sleep.37
Burden of medication
The adverse effects of the medications AR patients use to treat their symptoms can also be an issue. In order to feel better, persons with AR occasionally need to take multiple medications at once. According to the Allergies in America survey, OTC treatments are used by people with AR more frequently than prescription drugs. You can purchase over-the-counter (OTC) drugs without a prescription. The drugs that require a prescription can only be purchased with a doctor’s authorization. Intranasal corticosteroids are more effective than antihistamines for treating AR symptoms such as nasal obstruction, discharge, itching, and postnasal drip, according to clinical research. You spray intranasal corticosteroids into your nose to take them. Antihistamines are drugs that can be administered intravenously or orally. The individuals who take the prescription may get negative effects from both types of drugs, though. People with AR report that they feel dry (34%), have liquid leak down their throat (33%), feel tired (33%), experience headaches (25%), have a poor taste (22%), and feel burning (18%) are some of the side effects that they find extremely or very irritating. People with AR sometimes discontinue taking prescription drugs because they do not work as effectively (37%), work less over time (35%), do not last long enough (32%), or have bothersome side effects (25%).33,38
Burden of comorbidity
A person with AR may be dealing with other issues concurrently. Sinusitis, upper respiratory infections, otitis media with effusion (OME), and nasal polyposis are a few of these issues. When the sinuses swell up, it is called sinusitis. Allergy has also been considered a “contributing factor” in 40%–80% of the cases of chronic sinusitis.37 When the nose, throat, or lungs become infected, it is known as an upper respiratory infection. When there is fluid in the middle ear, it is known as otitis media with effusion (OME). Nasal polyposis is a condition where the nose has growths. According to population studies, 38% of all AR patients also have asthma, and 78% of all asthma patients have rhinitis.37 When the airways become constricted and difficult to breathe, it is called asthma. Numerous cases of chronic sinusitis can also be brought on by allergens. Allergens are things that make people allergic, like pollen or dust.38
Methodology
We searched for publications that were authored in English to conduct our investigation. We made use of certain websites with a large number of documents. These websites include Google Scholar, PubMed, ScienceDirect, the Directory of Open Access Journals, and Web of Science. We looked for documents that had certain words. These words were “Review OR Pathology” OR/AND “Allergic Rhinitis OR Hay Fever.” To locate more publications, we combined these words in various ways. The articles in which the papers we found cited were also examined. In this manner, we tried to find other papers that deal with our subject. For this study, 30 publications were used.
DISCUSSION
Allergic rhinitis is a growing concern as it increasingly impacts a larger population. One of the most detrimental aspects of AR is its propensity to induce nasal congestion. This might potentially impede the quality of sleep. When individuals experience inadequate sleep, they may encounter a multitude of other issues. Individuals may experience sensations of drowsiness, fatigue, irritability, or cognitive disorientation during the day. Individuals may experience difficulties in cognitive processes such as thinking, memory, and learning. These issues have the potential to impact individuals of all ages, including both adults and children, albeit in distinct manners. Adult individuals may experience a decline in their work performance compared to their potential capacity. Additionally, it is plausible that they may have a higher incidence of workplace accidents or injuries. Children have the potential to exhibit increased levels of shyness or sadness. Individuals may also experience heightened levels of concern or fear. The efficacy of medications utilized for the treatment of AR may be insufficient for certain individuals. The duration of their efficacy may be insufficient to alleviate symptoms throughout the entire day. There is a demand for pharmaceutical interventions that provide extended relief from symptoms and enhance overall well-being.
Healthcare practitioners may occasionally lack a comprehensive understanding of the experiences and perspectives of individuals with AR. There is a possibility that individuals may have the belief that individuals are content with their treatment despite the presence of underlying dissatisfaction. This phenomenon has the potential to erode the faith individuals place in their healthcare providers, including physicians and nurses. Noncompliance with medication recommendations is a common occurrence among individuals. Individuals may consume either more or less than the recommended amount. This has the potential to exacerbate their symptoms related to AR or give rise to other complications. Healthcare practitioners have access to several technologies that enable them to assess the impact of AR on individuals’ health and overall well-being. The aforementioned tools are commonly referred to as health profile instruments. Individuals are queried on their emotional state and functional capabilities in relation to their AR experiences. Multiple researches have demonstrated that the utilization of these methods can facilitate the assessment of various therapies’ efficacy in enhancing individuals’ health and overall well-being. Several therapeutic interventions have been identified as potentially efficacious in managing AR, including non-sedating antihistamines, intranasal corticosteroids, and other pharmacological agents that have received approval for the treatment of this condition. Non-sedating antihistamines refer to pharmaceutical substances that do not induce drowsiness in individuals. Intranasal corticosteroids refer to pharmaceutical substances that individuals administer by nasal spraying. Healthcare practitioners have to employ these strategies and interventions in order to assist individuals suffering from AR. It is important to engage in more communication with individuals and actively attend to their apprehensions. In this manner, individuals may enhance their comprehension of augmented reality and effectively administer its use.
Current barriers
Education and training
There are significant gaps in allergy training and practice in India. In India, Allergy and Immunology (A&I) is not a recognized specialty. The Medical Council of India does not provide any postgraduate training courses in A&I. It has, however, provided a diploma program in A&I and established the objectives, skill sets, competencies, complete curriculum, training, and evaluation procedures, for which there have been few applicants.
A scarcity of India-specific scientific data and recommendations
Current Indian management methods are mostly based on guidelines taken from data gathered in Western nations, which might not be “suitable for purpose” in Indian medical practice. There are a few substantial and real-world research to back up these principles’ applicability to the Indian populace.
CONCLUSION
Allergic diseases are a global health problem, and India is no exception. There is a necessity for raising awareness of this expanding disease within the medical community, in addition to among national policymakers and the general public.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The American Academy of Allergy: An historical review. I. Forward. J Allergy Clin Immunol. 1979;64:332-3.
- [CrossRef] [PubMed] [Google Scholar]
- Homeopathy and allergology–from the beginnings until today. Allgemeine Homöopathische Zeitung. 2017;262:DF02-03.
- [PubMed] [Google Scholar]
- Homeopathy, immunology, and allergy: Other considerations. A century of homeopaths: Their influence on medicine and health. Homoeopaths. 2014;22:118.
- [Google Scholar]
- A review of homeopathic research in the treatment of respiratory allergies. Altern Med Rev. 2010;15:48.
- [PubMed] [Google Scholar]
- Prevalence of aeroallergens in patients of bronchial asthma and/or allergic rhinitis in India based on skin prick test reactivity. Indian J Allergy Asthma Immunol. 2017;31:45-55.
- [Google Scholar]
- Burden of allergic rhinitis: Allergies in America, Latin America, and Asia-Pacific adult surveys. Allergy Asthma Proc. 2012;33:S113-41.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of allergic diseases in the Indian subcontinent: Barriers and challenges. Lancet Glob Health. 2020;8:e478-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of allergic rhinitis: A review for the community pharmacist. Clin Ther. 2017;39:2410-19.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of allergic rhinitis and allergic rhinoconjunctivitis on adolescents: A literature review. Ann Allergy Asthma Immunol. 2018;121:43-52.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic rhinitis: Epidemiology and natural history. Allergy Asthma Proc. 2000;21:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of allergic rhinitis and associated risk factors in Asia. World Allergy Organ J. 2018;11:17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global asthma network phase I, India: Results for allergic rhinitis and eczema in 127,309 children and adults. J Allergy Clin Immunol Glob. 2022;1:51-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An appraisal of allergic disorders in India and an urgent call for action. World Allergy Organ J. 2020;13:100446.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of air pollution on allergic rhinitis and asthma: Consensus statement by Indian Academy of Pediatrics. Indian Pediatr. 2021;58:765-70.
- [PubMed] [Google Scholar]
- Prevalence of allergic rhinitis, related comorbidities and risk factors in schoolchildren. Allergy Asthma Clin Immunol. 2020;16:98.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global map of the prevalence of symptoms of rhinoconjunctivitis in children: The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three. Allergy. 2009;64:123-48.
- [CrossRef] [PubMed] [Google Scholar]
- Economic burden of the inadequate management of allergic rhinitis and urticaria in Asian countries based on the GA2LEN model. Allergy Asthma Clin Immunol. 2018;10:370-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of allergic rhinitis and associated risk factors in Asia. World Allergy Organ J. 2018;11:17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Allergic rhinitis and treatment modalities: A review of literature. Cureus. 2022;14:e28501.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- BSACI guidelines for the management of allergic and non‐allergic rhinitis. Clin Exp Allergy. 2008;38:19-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Immunolocalization of cytokines in the nasal mucosa of normal and perennial rhinitic subjects. The mast cell as a source of IL-4, IL-5, and IL-6 in human allergic mucosal inflammation. J Immunol. 1993;151:3853-65.
- [PubMed] [Google Scholar]
- Interleukin-13 expression in the nasal mucosa of perennial allergic rhinitis. Am J Respir Crit Care Med. 1995;152:2059-67.
- [CrossRef] [PubMed] [Google Scholar]
- Zonula occludens and nasal epithelial barrier integrity in allergic rhinitis. Peer J. 2020;8:e9834.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Symptom severity assessment of allergic rhinitis: Part 1. Ann Allergy Asthma Immunol. 2003;91:105-14.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in allergic rhinitis. Ther Adv Respir Dis. 2012;6:25-39.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life assessments in clinical trials. In: Spiker B, ed. Definitions and conceptual issues. New York: Spilker, Bert; 1990. p. :11-24.
- [Google Scholar]
- Economic impact and quality-of-life burden of allergic rhinitis. Curr Med Res Opin. 2004;20:305-17.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in adults and children with allergic rhinitis. J Allergy Clin Immunol. 2001;108:S45-53.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of quality of life in patients with perennial allergic rhinitis with the French version of the SF-36 Health Status Questionnaire. J Allergy Clin Immunol. 1994;94:182-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in adults and children with asthma and rhinitis. Allergy. 1997;52:971-7.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring quality of life in children with rhinoconjunctivitis. J Allergy Clin Immunol. 1998;101:163-70.
- [CrossRef] [PubMed] [Google Scholar]
- Allergies in America: A landmark survey of nasal allergy sufferers. Health STAR Communications, Inc. Sponsored by Altana Pharma US; 2006.
- Psycho-emotional characteristics of the adolescents with allergic rhinitis. Georgian Med News. 2015;243:38-42.
- [PubMed] [Google Scholar]
- Prevalence of allergic rhinitis among elementary and middle school students in Changsha city and its impact on quality of life. J Laryngol Otol. 2015;129:1108-14.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126:466-76.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic rhinitis: Indicators of quality of life. J Bras Pneumol. 2010;36:124-33.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of allergic rhinitis. Allergy Asthma Proc. 2007;28:3-9.
- [CrossRef] [PubMed] [Google Scholar]
- Breathing disorders in sleep associated with “microarousals” in patients with allergic rhinitis. Acta Otolaryngol. 1981;92:529-33.
- [CrossRef] [PubMed] [Google Scholar]





