Translate this page into:
Celiacomesenteric trunk – A not so common variation
*Corresponding author: Rajeev Panwar, Department of Anatomy, ESIC Medical College & hospital, Chennai, Tamil Nadu, India. rajeevpanwar96@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Panwar R, Nair AS, Athindranath T, Adibatti M, Krishnamurthy A, Celiacomesenteric trunk – A not so common variation. Ann Natl Acad Med Sci (India) 2024;60:282-5. doi: 10.25259/ANAMS-2023-4-8-(899)
Abstract
The Coeliac trunk is the first ventral branch of the abdominal aorta and is the artery of the foregut, which supplies the derivatives of the foregut i.e., oesophagus, stomach, liver, gallbladder, pancreas, and the second part of the duodenum, up to the level of the opening of the major duodenal papilla. The superior mesenteric artery is the next branch of the abdominal aorta, which arises most commonly at the level of the first lumbar vertebra and supplies embryonic derivatives of the midgut i.e., from the second part of the duodenum (below the level of major duodenal papilla) to the proximal two-thirds of the transverse colon. Sometimes coeliac trunk and superior mesenteric artery arise as a common celiacomesenteric trunk. The embryological basis of celiacomesenteric trunk is discussed in the current case report. Also, the clinical significance of celiacomesenteric trunk in various conditions is described. During complex interventional procedures, this type of variation must be looked at carefully in radiological images to reduce the chances of postoperative complications.
Keywords
Celiac trunk
Celiacomesenteric trunk
Foregut
Midgut
Superior mesenteric artery
INTRODUCTION
Coeliac trunk (CT) is the first branch of the descending aorta after its passage via diaphragm at the level of 12th thoracic vertebra and supply the derivatives of the foregut. Following its origin at the junction between T12 and L1 vertebrae, CT runs a quick course and gives three branches, i.e., the left gastric artery (LGA), common hepatic artery (CHA), and splenic artery (SA). CT supplies Gastro Intestinal Tract (GIT) from the oesophagus to second part of duodenum (up to the level of major duodenal papilla), apart from liver, gallbladder, and pancreas.1
Superior mesenteric artery (SMA) is the next branch of abdominal aorta, given at the level of first the lumbar vertebra. SMA passes forwards and inferiorly after its origin, posterior to the body of pancreas, and anterior to uncinate procedure to enter the root of mesentery of small intestine and supplies embryonic derivatives of midgut i.e., from the second one part of the duodenum (below the level of major duodenal papilla) to proximal two-thirds of the transverse colon.1
GIT is supplied by the arteries derived from the primitive dorsal aorta as four splanchnic roots which are connected through a longitudinal ventral anastomosis. During the development, following obliteration within the anastomosis results in CT, SMA, and inferior mesenteric artery (IMA).2 Incomplete obliteration of the anastomosis leads to variation in origin of CT, SMA, and IMA or their next branches.3 Information about variations in origin and course of these branches is very important to evade any injury or bleeding during any intra-abdominal surgery.
In the current case report, a common celiacomesenteric trunk (CMT) has been reported which was found in a female cadaver, where CT and SMA had common origin but normal course and branching pattern, thereafter.
CASE REPORT
During cadaveric dissection of the abdomen region of a female body for first years medical undergraduate (UG) students, a CMT was found, which originated from abdominal aorta at first lumbar vertebra level and then bifurcated into CT and SMA [Figure 1]. Further, these two arteries followed a typical course anatomically, had standard branching pattern and the lumen of both arteries was of almost same size [Figure 2].

- Showing orientation of arteries as observed in the cadaver 1 – Abdominal aorta, 2 – Superior mesenteric artery, 3 – Coeliac trunk, 4 – Common hepatic artery, 5 – Gastroduodenal artery, 6 – Proper hepatic artery, 7 – Splenic artery.
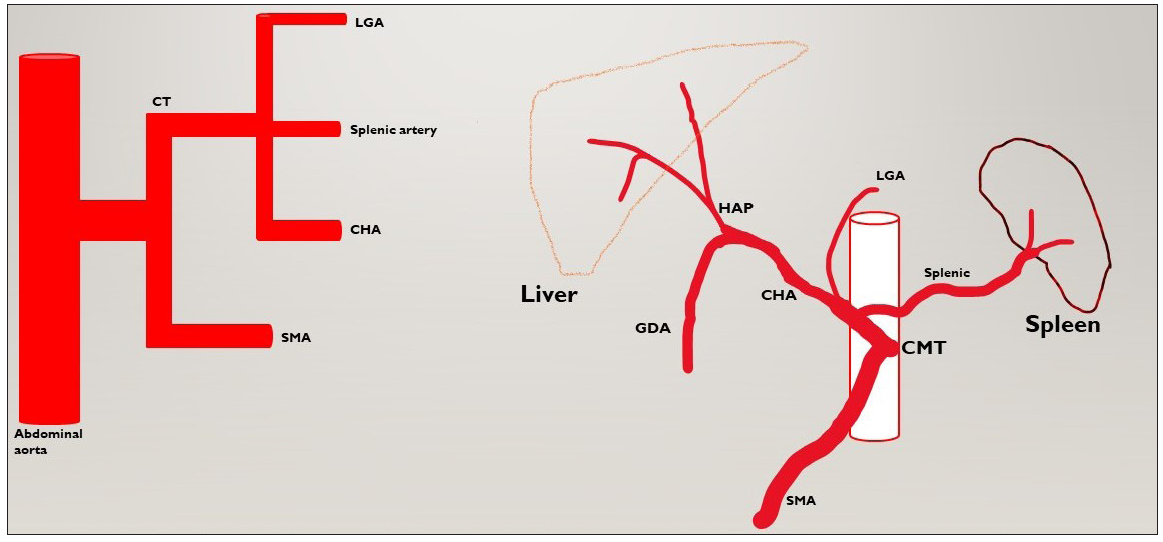
- Depicting the common origin of coeliacomesenteric trunk. CT: Coeliac trunk, LGA: Left gastric artery, CHA: Common hepatic artery, SMA: Superior mesenteric artery, GDA: Gastroduodenal artery, HAP: Hepatic artery proper, CMT: celiacomesenteric trunk
DISCUSSION
Initially, the growing embryo is supplied by a longitudinally located pair of dorsal aortae. As the growth progresses, ventral splanchnic arteries (paired segmental branches to the digestive tube), dorsal somatic arteries (intersegmental branches to the body wall), lateral splanchnic arteries (paired segmental branches to the urogenital system) are given via each primitive dorsal aorta and progress caudally to the body stalk as umbilical arteries.
Distribution to the capillary plexus of the yolk sac is furnished by paired ventral splanchnic arteries. On fusion of the dorsal aortae, the pair of ventral arteries merge to shape unpaired trunks which supply the primitive digestive tube – linked dorsally and ventrally by longitudinal anastomotic channels (dorsal and ventral splanchnic anastomosis). This anastomosis reduces the ventral splanchnic trunk to three major arteries: CT, SMA, and IMA. These arteries migrate from their initial place of origin as the viscera descend downwards in the following manner:
-
a.
CT from C7 to T12
-
b.
SMA from T12 to L1
-
c.
IMA from T12 to L3
Tandler described origin of visceral arteries from the primitive dorsal abdominal aorta as four splanchnic roots (LGA, CHA, SA, and SMA) which are connected through a longitudinal ventral anastomosis.2 The anastomosis is commonly obliterated above SMA, during the development, resulting in continuation of visceral arteries as CT, its three visceral branches – SA, LGA, CHA, and SMA. Further, SMA provides – the inferior pancreaticoduodenal artery, right colic artery, middle colic artery, ileocolic artery, and jejunal and ileal branches [Figure 3].
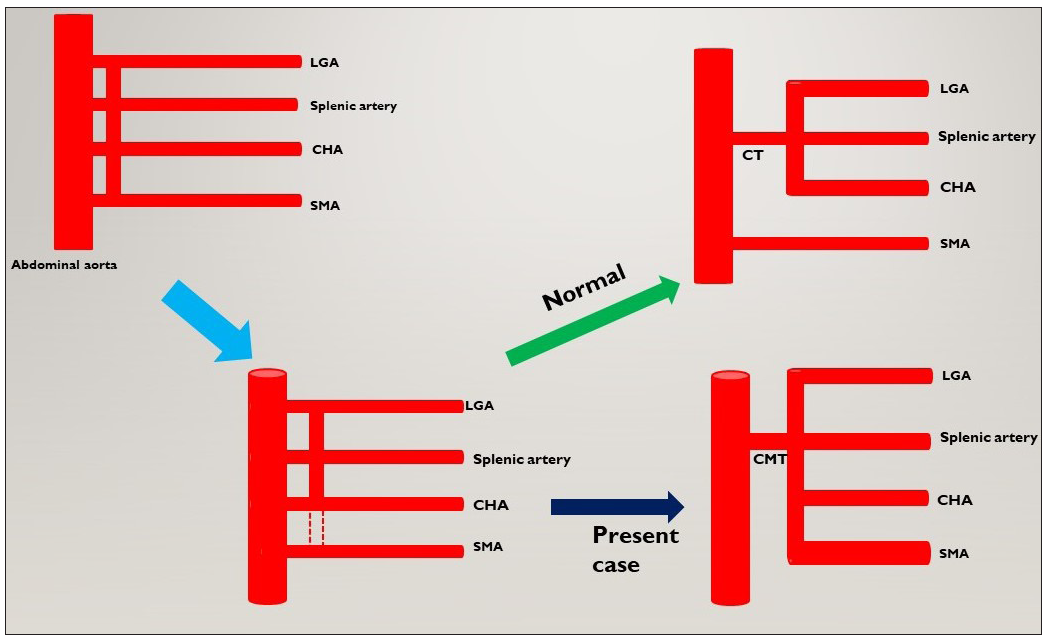
- Depicting short-type coeliacomesenteric trunk. CT: Coeliac trunk, LGA: Left gastric artery, CHA: Common hepatic artery, SMA: Superior mesenteric artery, GDA: Gastroduodenal artery, HAP: Hepatic artery proper, CMT: celiacomesenteric trunk
The current case report describes presence of a CMT on the anterior surface of the aorta due to incomplete obliteration of the longitudinal ventral anastomosis and giving CT and SMA. The prevalence of variation was found to be 1%–2.7%.3 Similar types of variation had been mentioned in the past.4,5 Rusu et al. (2021) have described the frequencies of occurrences of the different vertebral level origins of the CT and SMA.6 Vidya CS et al. (2021) have discussed the anatomical variations in the course of CT and its branching pattern with subsequent surgical implications in an urban population.7 Panagouli E et al. (2013) have reported the distinctive kinds of anatomical variations of CT along with the probable effect of genetic factors and the incidence which was found to be 0.76%. Also, as per Panagouli’s Classification, CMT belonged to type IV of Celiac Trunk.8 Wang, Y. et al. (2010) described a case of saccular aneurysm at the bifurcation of a CMT using celiac digital subtraction angiography (DSA), which was surgically removed to avoid the risk of a rupture of the aneurysm.9 These various types of variations were accidentally found during aneurysms rupture, sometimes, presented with lower limb ischemia and were treated by aortic bypass surgeries or reimplantation, and transplantations.10
Nutcracker syndrome is a rare clinical scenario due to entrapment of the left renal vein between the aorta and SMA, mostly due to presence of CMT or an unusual origin of SMA from the aorta resulting in renal venous hypertension. The signs and symptoms of Nutcracker syndrome range from asymptomatic haematuria to excessive pelvic congestion. Al-Zoubi et al. (2017) have reported the association between CMT and Nutcracker syndrome.11 Peterson J et al., (2017) described presence of CMT, associated with left renal vein compression manifesting as dilatation and engorgement, thus indicating association between CMT and Nutcracker syndrome.12 A rare variety of CMT along with retro-aortic left renal vein was reported in a young male cadaver in 2018, which had features suggestive of posterior nutcracker syndrome.13 Nutcracker syndrome has comparable pathophysiology with SMA syndrome which is due to reduced angle between the origin of SMA and the abdominal aorta leading to reduction in lumen of the third part of duodenum and culminating in bowel obstruction. Thus, coexistent SMA and Nutcracker syndrome have been reported in past, but, isolated Nutcracker syndrome causing narrowing or compression of the third part of duodenum have not been reported.14-17
A new classification for the CMT was proposed by Tang W et al. (2019) using multi-detector computed tomography (MDCT) angiography to identify types and prevalence in a large study population.18 A newborn was found to have CMT along with a massive omphalocele but the association among the two could not be established. No case of CMT has been reported in association with malrotation of intestine.19
CONCLUSION
Identification of the possible variations of the arteries supplying the foregut and midgut along with radiological studies helps to reduce the risk of surgical iatrogenic injuries. Careful observation of these variations in radiological images should be of utmost importance prior to complex surgical interventional procedures to reduce the risks of postoperative complications. Arterial variation should be correctly identified along with the dimensions before surgeries such as transplantation, tumor resection or chemoembolization of gastrointestinal malignancy, and abdominal laparoscopic surgeries. Hence, the variation found in this case report is of surgical and therapeutic significance.
Authors’ contributions
RP: Conceptualization; AN, TA: First draft; RP, MA, AK: Critical review.
Acknowledgements
We would like to express our gratitude to staff of the Department of Anatomy for their continued support and help during the dissection. We would like to thank our Head of the Department for giving permission to use the cadaver for dissection.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Standring S, ed. Gray’s Anatomy: the anatomical basis of clinical practice (Forty-first edition). New York: Elsevier Limited; 2016. p. :1088, 1117, 1126, 1169.
- Über die varietäten der arteria coeliaca und deren Entwicklung. Anat Embryol. 1904;25:473-500.
- [Google Scholar]
- Atlas of normal and variant angiographic anatomy. Philadelphia, PA: Saunders; 1991. p. :297-364.
- Anatomical variations of the celiac trunk: A systematic review. Arq Bras Cir Dig. 2018;31:e1403.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Aortic origins of the celiac trunk and superior mesenteric artery. Diagnostics (Basel). 2021;11:1111.
- [CrossRef] [PubMed] [Google Scholar]
- have discussed the anatomical variations of celiac trunk and its branching pattern with special reference to surgical implications in Mysore based population. J Evolution Med Dent Sci. 2021;10:3225-30.
- [Google Scholar]
- Variations in the anatomy of the celiac trunk: A systematic review and clinical implications. Ann Anat. 2013;195:501-11.
- [CrossRef] [PubMed] [Google Scholar]
- Celiomesenteric trunk with concurrent aneurysm: Report of a case. Surg Today. 2010;40:477-81.
- [CrossRef] [PubMed] [Google Scholar]
- Celiacomesenteric trunk: A variation that must be known before aortic surgery. Clin Pract. 2011;1:e69.
- [CrossRef] [PubMed] [Google Scholar]
- Nutcracker syndrome associated with celiacomesentric trunk anomaly: Case report. Int J Nephrol Renovasc Dis. 2017;10:285-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Incidental anatomic finding of celiacomesenteric trunk associated with ‘nutcracker phenomenon,’ or compression of the left renal vein. Am J Case Rep. 2017;18:1334-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A rare combined variation of the coeliac trunk, renal and testicular vasculature. Anat Cell Biol. 2018;51:62-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Coexistence of superior mesenteric artery syndrome and nutcracker phenomenon. Radiol Case Rep. 2022;17:1927-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Superior mesenteric artery syndrome combined with renal nutcracker syndrome in a young male: A case report. Korean J Gastroenterol. 2017;70:312.
- [CrossRef] [PubMed] [Google Scholar]
- A model example: Coexisting superior mesenteric artery syndrome and the nutcracker phenomenon. Case Rep Surg. 2015;2015:649469.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Superior mesenteric artery syndrome and the ‘nutcracker phenomenon’. BMJ Case Rep. 2013;2013:bcr2013008734.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Celiomesenteric trunk: New classification based on multidetector computed tomography angiographic findings and probable embryological mechanisms. World J Clin Cases. 2019;7:3980-89.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Celio-mesenteric trunk associated with giant omphalocele: Surgical consequences. Int J Morphol. 2017;35:938-41.
- [CrossRef] [Google Scholar]






