Translate this page into:
Effect of modifiable lifestyle risk factors on the incidence and prevention of cancer in modern society: A review
*Corresponding author: Dr. Tania Sarkar, Department of Zoology, Rishi Bankim Chandra College, Naihati, India. Email: taniasarkar0102@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhattacharjee N, Sarkar T. Effect of modifiable lifestyle risk factors on the incidence and prevention of cancer in modern society: A review. Ann Natl Acad Med Sci (India). 2024;60:3-13. doi: 10.25259/ANAMS-2022-10-5-(757)
Abstract
Human society has been influenced by modernization, which has altered our pattern of living. It is believed that several environmental and lifestyle factors, including urbanization, employment linked to socioeconomic transition, increased affluence, and altered social and family structures, are partially to be blamed for cancer. Lifestyle changes associated with urbanization such as smoking, alcohol consumption, excessive body weight, and being physically inactive are well-known risk factors for cancer. Anxiety due to stressful events can increase the production of free radicals, which in turn causes oxidative damage and the emergence of cancer. Economic liberty provides more leisure time and inclination toward ready-to-eat food, more screen time, and sedentary habits to some extent. All these factors have a positive impact on cancer initiation and development. Hence, a healthy lifestyle, together with nutritious food and regular exercise should be prioritized for cancer prevention. A healthy lifestyle has been associated with a decreased risk of different types of cancer, involving the lungs, liver, colon, breast, endometrium, and kidney. To outline this review, searches were performed with PubMed and Scopus databases up to August 2022. The lifestyle risk factors for cancer have been described in this review, along with recommendations for improving lifestyle choices for human welfare.
Keywords
Cancer
Lifestyle
Physical Activity
Stress
INTRODUCTION
Over the past few decades, a trend has been observed wherein there is an increase in the incidence of noncommunicable diseases than infectious diseases and the prevalence of noncommunicable diseases such as cardiovascular diseases and cancer has been on the rise mostly in developing countries1–3 In modern world, our way of living has changed as a result of globalization, increased wealth, altered social and family structures, a lack of physical activity, and anxiety brought on by stressful events.4 The incidence of cancer has increased greatly due to these lifestyle factors, but it can be prevented by major lifestyle changes.5 It has been reported that these lifestyle risk factors are related to various types of cancer involving breast, lung, prostate, colon, and stomach.6
When the world’s population reaches 8.3 billion in 2030, there are likely to be 21.4 million cases and 13.2 million deaths due to cancer.7 The increased incidence of cancer has been documented in various studies.8 Lung cancer is a prominent cause of mortality in males,9 and breast cancer is prevalent among females.8 Other common causes of death in males are colorectal cancer (CRC) and prostate cancer.8 Hepatocellular carcinoma (HCC), affecting all age groups in both males and females is in the sixth position after breast, lung, prostate, colon, and stomach cancer.8,10 Smoking, alcohol consumption, unhealthy eating habits, and excess body weight are lifestyle risk factors and are responsible for 35% of cancer deaths worldwide.11 In 2021, Friedenreich et al. documented that obesity and sedentary behavior are associated with cancer.12 While these aspects of lifestyle are not inherently unique to contemporary culture, they have become more prevalent in many societies due to the effect of globalization. Healthy lifestyles may reduce the incidence of cancer morbidity and mortality to a great extent and for cancer prevention, priority should be given to these factors.13 Among many modifiable risk factors, the most notable are alcohol consumption, smoking, obesity (high BMI, measured in kg/m2), and insufficient physical activity (sufficient physical activity 3 30 min/five times/week or minimum 1,600–2,400 calories/day burnt for adult women and 2,000–3,000 calories/day burnt for adult men)14,15 and 30–40% of cancers are preventable by the transformation of modifiable lifestyle risk factors.16 A healthy lifestyle combined with proper diet and exercise should be prioritized for cancer prevention as it negatively impacts lymphoma, myeloma, lung, colon, breast, endometrial, and kidney cancer incidence.
However, it is important to understand that cancer is a complicated illness, and a number of circumstances might lead to its occurrence. Lifestyle factors are just one piece of the puzzle, and it is often difficult to isolate their effects from other factors such as genetics, environmental exposures, and medical history.
REVIEW METHODOLOGY
For this review, searches were conducted in databases such as PubMed, Scopus, and Web of Sciences for all full-text articles up to August 2022 using combinations of various key terms such as “cancer”, “lifestyle”, “modifiable risk factors”, “lung cancer”, “liver cancer” or “hepatocellular carcinoma”, “melatonin”, “sleep deprivation”, and “tobacco smoking/adverse effects”. The lifestyle factors mainly included tobacco smoking, alcohol consumption, sedentary behavior, overweight/obesity, and diet, while some studies also included green tea consumption, fruit and vegetable consumption, the damaging effect of blue light, sleep deprivation, exposure to indoor air pollution, practicing yoga and physical activity. Besides the reference lists of original studies, reviews and meta-analyses were also scrutinized to identify relevant studies.
Included studies fulfilled the following criteria: (i) prospective cohort studies; (ii) review article; (ii) incident total and site-specific cancer or cancer mortality; (iii) focusing on a single lifestyle factor; (iv) a combination of only two lifestyle factors; and (v) using the combination of lifestyle factors as an exposure variable. Studies were excluded if they were: (i) other publication types (such as protocols, case-control studies) or not peer-reviewed publications (such as editorials and commentaries); (ii) formulation or validation of prediction models; (iii) duplicate reporting from the same cohort studies or duplicate publications; and (iv) studies without necessary or sufficient data.17
THE INCIDENCE OF CANCER AND LIFESTYLE FACTORS
Obesity and cancer
Obesity (BMI 3 30 kg/m2)18 is linked to an enhanced risk of cancer of the endometrium, esophagus, colon, kidney, liver, pancreatic tissues, and breast in postmenopausal women, and also poses a threat of malignant melanoma.19,20
It has been reported that intentional weight loss among obese women can reduce the risk of endometrial cancer by 54%.21 Excessive body fat at a young age is linked to the development of eight kinds of cancer in later stages of life.22 Postmenopausal breast cancer risk is greater in adult women who have a body mass index > 23.4 kg/m2 at 20 years of age.23 Chronic inflammations, inhibition of apoptosis, and oxidative stress have been observed in carcinogenesis, which is stimulated by obesity.24
Sedentary behavior and cancer
Inflammatory factors like tumor-necrosis factor-a, interleukin-6, and leptin might lead to the progression of cancer in the lung and these factors might aggravate due to sedentary behaviors.25 It has been reported by a meta-analysis that sedentary behavior and television watching are linked to lung cancer, colon cancer, and endometrial cancer.26
More than a quarter of the global population is not properly active.27 An inverse relationship has been found between physical activity and many types of cancer.28 Obesity-induced carcinogenesis has been linked to oxidative stress, apoptotic suppression, and chronic inflammation.24 It has been observed that moderate-to-vigorous physical activity (sufficient physical activity 3 30 min/five times/week or minimum 1,600–2,400 calories/day burnt for adult women and 2,000–3,000 calories/day burnt for adult men) during leisure time and reduction of television watching has been related to an increase of cancer-free (colorectal, lung, prostate, and postmenopausal breast cancer) life span.29 It is also reported that television watching is associated with the risk of lung cancer and less television watching especially in smokers might avert lung cancer.30 Hence, moderate physical activity of 150 minutes or vigorous physical activity of not less than 75 minutes per week has been recommended (sufficient physical activity 3 30 min/five times/week or minimum 1,600–2,400 calories/day burnt for adult women and 2,000–3,000 calories/day burnt for adult men).14,15,28,31 Global action plan of WHO on physical activity 2018–2030 may be implemented by some countries32 to combat the situation.
Smoking and cancer
The smoke of tobacco contains carcinogens that induce somatic mutation as a result of the generation of DNA adducts.33 Passive smoke is also considered carcinogenic by the International Agency for Research on Cancer (IARC).34 It has been reported that cigarette smoking caused 48% of all cancer deaths in the United States.35 The incidence of cancer and cancer death associated with tobacco smoking has been extensively documented in a population-based Australian cohort study.36 Tobacco smoke causes the development of cancer in different organs throughout the body like the mouth, pharynx, trachea, voice box, lungs, liver, and esophagus [Figure 1]. Carcinogens produced during tobacco smoking are associated with pancreatic, colon, uterine and bladder cancer.37 Tobacco use is a major factor in the development of cancer; however, obesity and lack of physical activity pose a greater threat to carcinogenesis, which we have described in the previous segment.38

- Tobacco smoking can cause cancer throughout the body. Tobacco smoke contains various types of carcinogens which promote the progression of cancer in multiple sites throughout the body, for example, in mouth, pharynx, voice box, trachea, lungs, liver, esophagus, stomach, pancreas, bladder and colon. (Created in Biorender.com)
Alcohol consumption and cancer
Researchers showed that alcohol consumption is associated with pancreatic cancer.39 Consumption of alcohol escalates cancers such as of the liver, stomach, colorectal area, mouth, larynx, and pharynx.19 As alcohol plays a major role in the development of cancer, population awareness regarding the risk of cancer due to alcohol consumption should be increased and alcohol restriction policy measures need to be implemented.40
Indoor and outdoor ambient air pollution and cancer
Indoor air pollution due to the use of coal has been associated with lung cancer.41 Globally, it has been observed that outdoor ambient air pollution is linked to an increased incidence of lung cancer and many lung cancer–related deaths.42 The carcinogenic potential of outdoor air pollution might be associated with black carbon exposure.43 Polluted air contains particles as well as gases.44 Particulate matter (PM2.5) has been recognized as a risk factor for lung cancer by IARC.45
Air pollution might cause a risk of brain cancer through oxidative stress mediated by neuroinflammatory signaling pathways.46 The IARC Working Group has reckoned outdoor air pollution and particulate matter as carcinogenic to humans.47 Long-term exposure to low-level ambient air pollution is also related to cancer incidence in the lung.48
Unhealthy diet and cancer
It has been well documented that some dietary and lifestyle factors such as the consumption of red meat has been associated with the incidence of colon cancer.49 In the Chinese population, processed meat could cause nearly 1% of CRC deaths.50 According to a study done in the United States of America, a daily increase in the consumption of processed and unprocessed red meat was associated with a 13% rise in cancer mortality.51 It has been presumed that taking large amounts (determined by the United Nations to be 200 g or more on a daily basis) of red meat is linked to enhanced cancer risk.52
Heterocyclic aromatic hydrocarbons, which are hazardous chemicals, might originate during the processing, curing, and preservation of food and red meat.53 Healthy eating patterns have been recommended by the American Cancer Society for all ages.54 A healthy lifestyle should be followed to prevent cancer incidence.55
Effective role of fish oil in cancer prevention
Omega-3 fatty acids present in fish oil show anti-inflammatory, anti-proliferative, and anti-metastatic potential.56
Protective potential of green tea against cancer
Polyphenol present in green tea is epigallocatechin-3-gallate (EGCG), which is a phytochemical and it plays a significant role in various cancers mediated by epigenetic mechanisms.57 Consumption of green tea along with green leafy vegetables might hinder ovarian cancer.58 Green tea has been studied for its cancer-fighting properties, and the results are encouraging. EGCG has been linked to cancer prevention.59 The recent information regarding the anti-cancer effects of green tea extracts in the prevention and treatment of prostate cancer has been reviewed.60 EGCG has been reported to sensitize cancerous cells to apoptosis caused by antineoplastic drugs, and it can guard noncancerous cells against the dangerous outcome of ultraviolet radiation exposure.61
Endocrine-disrupting chemicals and cancer
It has been observed that endocrine-disrupting chemicals (EDCs) has carcinogenic potential.62 It has been reported that EDCs such as Bisphenol A,63 Phthalate,64 Parabens,65 various personal care products,66 and other EDCs67 can act as the triggering factor of cancer.
Mental and physical stress and generation of free radicals
Stress is the altered physiological condition in the body which occurs due to intrinsic or extrinsic stressors, and these affect the homeostasis of the body.68 The production of free radicals, such as reactive oxygen species and reactive nitrogen species (ROS/RNS) is elevated during stress. Continuous stressful conditions can induce anxiety and depression, thereby producing these free radicals and oxidative damage.69 Mental and physical stress result in the formation of free radicals and oxidative stress in the human body, which in turn destroy the antioxidant properties of our body, leading to cancer growth. The abundance of free radicals reduces the effectiveness of antioxidant enzymes which eventually increases cancer risk. It has been observed in cancerous and precancerous tissues that elevated ROS level is linked to changes in nucleobases.70
The development of HCC has been induced by oxidative stress.71 The levels of glutathione peroxidase, catalase, and superoxide dismutase, which are potential antioxidant enzymes reduced during stress, are associated with cancer.72 Increased generation of HO• (hydroxyl radical or hydroxide ion) and other free radicals makes the cells susceptible to DNA mutation and activates oncogenes, which cause initiation and progression of cancer.73 Several lifestyle factors such as consumption of alcohol, smoking, improper diet, and lack of sufficient exercise play important roles in the development of oxidative stress.74
Changes in the sleep cycle and sleep deprivation
People need adequate sleep to function properly. Melatonin, which is required for sleep, is secreted at maximum levels till midnight from the pineal gland and gradually decreases in the morning.75 People today are becoming more and more addicted to social media and use their electronic devices excessively. It is now established that blue light emitted from electronic gadgets is one of the most important reasons for sleep deprivation.76 Sleep deprivation influences the generation of free radicals, which induces the development of many types of cancer in the body.77 The sleep cycle is altered as a result of people sleeping less at night and more in the morning. Melatonin also acts as an antioxidant.78 Hence, decreased melatonin levels due to sleep deprivation can be considered a cause of cancer.79
The damaging effect of blue light on the eye
The human eye may be badly affected by blue light. It is noted that a portion of blue light overlaps with UV which causes skin cancer.80 Several physiological problems arise due to smartphone light fluxes (SPLF), such as reduction of melatonin secretion, changes in circadian rhythm, and faulty eyesight as (SPLF) spectrum overlaps in UVA (320–410 nm) portion.81 It is reported that blue light at night produced by electronic devices such as smartphones causes a detrimental effect on the body’s physiological activity.82
It is reported that intensive blue light (400 nm to 440 nm) induces damage to the retina and is associated with the process of photo-bleaching83, causing absorption of photons by rhodopsin and increasing the generation of reactive oxygen species which causes oxidative damage due to the accumulation of lipofuscin pigment (the yellow-brown pigment which consists of lipids and proteins and has fluorescent properties) in the retinal pigment epithelium.75,84 Artificial blue light at night exposure results in a disruption of circadian rhythm, which might enhance breast and prostate cancer risk.85 Exposure to outdoor blue light that has become enhanced in recent times might pose a threat to producing CRC.86
Harmful effects of blue light on circadian rhythm and sleep deprivation can cause oxidative stress
The suprachiasmatic nucleus in the hypothalamus regulates the circadian rhythm and sleep. Blue light emitted by electronic gadgets affects the phase delay of the circadian rhythm as well as causes suppression of melatonin release. Human physiology and mood are largely influenced by exposure to light.75 Excessive involvement with digital devices at bedtime results in an alteration in the quality and amount of sleep.87 Sleep deprivation causes oxidative stress.88 Some chronic and degenerative diseases such as cancer, arthritis, cardiovascular and neurodegenerative diseases, etc., are associated with oxidative stress.89 Reduced melatonin level is associated with major oxidative damage to DNA.90
The beneficial effect of melatonin
It has been reported that melatonin has anti-carcinogenic potentiality as well as antioxidant and immunomodulatory characteristics.91 Melatonin protects the body from oxidative stress caused by free radicals produced at the time of metabolism.92 Free radical scavenging activity of melatonin has been documented by many researchers.93 There are several noteworthy functions of melatonin such as ameliorating sleep quality, decreasing free radicals formation, and restitution of antioxidant enzymes.94
Different reviews described anti-carcinogenic potential,95 therapeutic efficacy,96 and protective effect of melatonin against oxidative harm to DNA.92 Melatonin has the potential to reduce breast cancer.97 Melatonin can alleviate oxidative stress directly through a detoxification mechanism or indirectly by preventing prooxidative enzymes and inducing the body’s antioxidant enzymes.98 Initiation, progression, and metastasis of cancer can be prevented by melatonin.99 By combating oxidative damage, melatonin renders protection to proteins, lipids, and DNA.100
Detrimental effect of melatonin suppression at night
It has been documented that disruption of the normal secretion of melatonin at night due to exposure to light is associated with cancer risk.101 Working at night for a long time with exposure to blue light disrupts the circadian rhythm and decreases melatonin secretion and results in sleep deprivation.102 It is reported that shifting working hours increases the risk of breast cancer in females by 40%.103 Disruption of circadian rhythm by exposure to light at night during shifting duty and night work may act as triggers of Group 2A carcinogen according to IARC.104
DISCUSSION
This review focuses on spreading public awareness about modifiable lifestyle risk factors with the help of scientific literature and evidence of experimental works and aims to overview the impact of changes in these factors to prevent the incidence of cancer. Obesity, smoking, alcohol use, physical inactivity, poor eating habits, disturbed sleep, and oxidative stress are few risk factors that can raise the risk of developing cancer. People who eat diets rich in trans fat, saturated fat, and high calories are generally obese. People who do not exercise regularly may be at increased risk of cancer. Inadequate sleep is reckoned as a vital risk factor for stress, which results in the initiation of cancer. Consumption of green tea along with green leafy vegetables might hinder ovarian cancer. Catecholamines’ level increases on account of the inadequacy of sleep; as a result, blood pressure and blood glucose levels increase, causing oxidative stress and injury in the wall of blood vessels. Restoration of good health requires proper sleep at night. Unhealthy lifestyle choices might influence the risk of cancer [Figure 2].
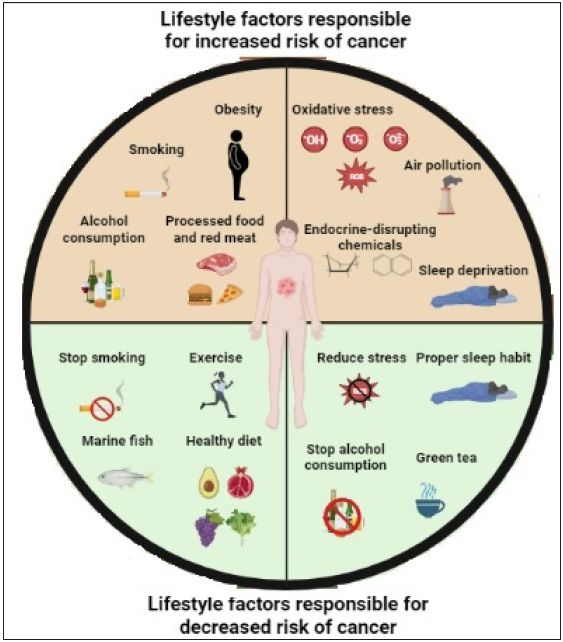
- Cancer incidence and prevention are significantly impacted by changes in lifestyle risk factors. Among many risk factors, the most important are alcohol, processed food and red meat consumption, smoking, obesity, changes in circadian rhythm, excessive stress, air pollution and endocrine-disrupting chemicals and are responsible for different human malignancies. However, 30–40% of these cancers can be prevented by avoiding these lifestyle risk factors and maintaining a healthy lifestyle. (Created in Biorender.com)
RECOMMENDATIONS TO REDUCE THE RISK OF CANCER
Stop smoking
Consuming tobacco in any form (smoking or chewing) is linked to cancer of the mouth, larynx, throat, lung, pancreas, kidney, bladder, and cervix.105–108 Passive smoking also triggers the risk of lung cancer.34
Avoid alcohol consumption
According to a report by World Cancer Research Fund International (WCRF), alcohol intake raises the risk of many forms of cancers, including those of esophagus, breast, colorectum, stomach, liver, mouth, pharynx, and larynx.19 Drinking alcohol is a significant lifestyle risk factor for cancer.40
Avoid red meat consumption
Avoid eating red meat to prevent colon and liver cancer development. Replacement of red meat with foods such as legumes, soy, nuts, poultry, and fish would decrease the threat of cancer and reduce levels of cholesterol.109
Take a healthy diet
Fruits and vegetables have a possible anti-carcinogenic effect. Eating an abundance of fruits and vegetables with dietary fiber reduces the risk of CRC and liver cancer in males.110 Bacteria reside in the colon and produce products through the fermentation of dietary fibers, having anti-proliferative potentiality.111 Less quantity of vegetable and fruit consumption is ascribable to the burden of diseases worldwide, and available recommendations for the intake of fruit and vegetables should be followed.112 Follow the WCRF/American Institute for Cancer Research (AICR) recommendation to take a diet that consists of plenty of whole grains, beans, vegetables, and fruits to prevent cancer as well as various chronic diseases.113 The Mediterranean diet, which contains fruits, vegetables, legumes, nuts, and grains, is considered to be an effective anti-cancer diet.114
Consume plenty of fish
Oily fish such as herring, salmon, and mackerel contain omega-3 fatty acid, and the effective role played by omega-3 fatty acids found in various types of cancer has been extensively reviewed.115
Drink green tea
It contains catechins, a large group of flavonoids which are polyphenolic compounds with antioxidant characteristics. The principal type of catechin is EGCG, which has strong chemopreventive, anti-obesity, anti-cancer, and immune modulatory effects.116 Intake of green tea might be propitious for oral, esophageal, lung, ovarian, and endometrial cancer and cardiovascular disease.117 EGCG could control the activity and restrain the cell cycle by inducing kinase-mediating apoptosis pathways and impeding cell division, which result in cell death.118
Maintain a healthy body weight and avoid obesity
Eat lighter and stick to a low-fat diet because it has been discovered that proper weight management is linked to a decrease in the risk of cancer. High-calorie foods such as fat from animal sources and processed meat intake should be restricted. Sugar intake should also be restricted.113 When the consumption of non fried food increases, it reduces the risk of cancer of the pancreas.
Engage in physical activity
It will reduce the risk of cancer of the lung, prostate, kidney, colon, and breast. One must have physical activity of at least 30 minutes in the daily schedule. Higher levels of physical activity reduce the risk of several types of cancer.28 Leisure-time physical activity reduces the risk of bladder cancer by 13%. Physically active women had a reduction of breast cancer by 12–21% compared to those of the least active. Both in premenopausal and postmenopausal women, physical activity has been linked to similar reductions in the risk of breast cancer.119 In postmenopausal women, weight reduction due to physical exercise led to plummeting levels of C-reactive protein and estradiol, resulting in decreased risk of endometrial and breast cancer. According to the report of World Cancer Research Fund International, physical activity could reduce the risk of endometrial, breast, and colon cancer. World Health Organization provided guidelines that described the importance of physical activity.120 It has been established that cancers that are related to obesity could be decreased by physical activity.121 Exercise has also been beneficial for cancer survivors and the strength of cancer patients.122 Recommended amounts of activity, i.e., 7.5–15 metabolic equivalent task [MET] hours/week in leisure time is correlated with reduced risk of seven different types of cancers including colon, breast, endometrium, kidney, myeloma, liver, non-Hodgkin lymphoma.123
Avoid exposure to outdoor and indoor air pollution
Lung cancer due to short-term and long-term exposure to indoor and outdoor air pollutants has been described earlier.124,125 So try to avoid exposure to outdoor and indoor air pollution.
Avoid endocrine-disrupting chemicals
Consider maintaining a healthy lifestyle
Perform adequate physical exercise and practice yoga for a relaxed and healthy life. Smoking, drinking a large amount of alcohol, physical inactivity, and an unhealthy diet which are regarded by researchers as lifestyle and environmental factors are associated with pancreatic cancer.129 Approximately 12% of pancreatic cancer is estimated to be caused by obesity and 29% are linked to smoking.130 Yoga shows promising effects in decreasing the level of pro-inflammatory cytokines and upgrading the quality of human lives.131 Yoga is good for people because it reduces the Nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, a transcription factor that increases the production of inflammatory genes in response to chronic stress.132 A proper, healthy lifestyle regimen must be followed in order to reduce the cancer burden.121
Keep living a stress-free life
The effect of stress on the progression of cancer has been extensively reviewed. Mravec et al. described the importance of treatment with b-blocker and psychotherapy on the survival of cancer patients.133 Animal studies showed the mechanisms through which cancer progression has been expedited by stressful conditions. Hence, stress management interventions could decrease repetitiveness and death in cancer.134
Sleep well and sufficiently
Since circadian rhythm, quantity, and quality of sleep are affected by blue light,87 it is recommended to restrict oneself from using electronic gadgets before bedtime.135
Individuals should exercise daily and have a healthy lifestyle to prevent cancer
The American Cancer Society recommends physical activity of 150–300 minutes with moderate intensity or physical activity of 75–150 minutes with vigorous intensity per week in adults to reduce cancer risk.54 Recommendations regarding lifestyle for cancer prevention have been advised.55
CONCLUSION
The comprehensive analysis of this review gives prominence to the effect that modifiable lifestyle risk factors exert on the incidence and prevention of cancer. As this review discusses, dietary habits, physical activity levels, tobacco use, and alcohol use are important factors in cancer prevention and mitigation. Incorporating a healthy diet while minimizing processed foods and red meat intake, coupled with regular exercise, substantially reduces the risk of cancer development. Furthermore, strategies aimed at smoking cessation and limiting alcohol consumption are imperative in mitigating cancer risk, prioritizing the critical role of behavioral modifications in preventive efforts. Equally significant is the maintenance of a healthy body weight, as obesity not only escalates cancer risk but also worsens prognosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The burden of non communicable diseases in developing countries. Int J Equity Health. 2005;4:2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic Diseases: The emerging pandemic. Clin Transl Sci. 2011;4:225-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-communicable diseases (NCDs) in developing countries: A symposium report. Glob Health. 2014;10:81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438-47.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008;25:2097-3116. [Erratum in: Pharm Res 2008;25:2200. Kunnumakara, Ajaikumar B [corrected to Kunnumakkara, Ajaikumar B]
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diet and cancer prevention: Contributions from the European prospective investigation into cancer and nutrition (EPIC) study. Eur J Cancer. 2010;46:2555-62.
- [CrossRef] [PubMed] [Google Scholar]
- Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-917.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer statistics for the year 2020: An overview. Int J Cancer. 2021;149:778-89.
- [CrossRef] [PubMed] [Google Scholar]
- Lung cancer identification: A review on detection and classification. Cancer Metastasis Rev. 2020;39:989-98.
- [CrossRef] [PubMed] [Google Scholar]
- Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-49.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative risk assessment collaborating group (Cancers). Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366:1784-93.
- [CrossRef] [PubMed] [Google Scholar]
- Physical Activity, obesity and sedentary behavior in cancer etiology: Epidemiologic evidence and biologic mechanisms. Mol Oncol. 2021;15:790-800.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Combined lifestyle factors, incident cancer, and cancer mortality: A systematic review and meta-analysis of prospective cohort studies. Br J Cancer. 2020;122:1085-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105:S77-S81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The current and future burden of cancer attributable to modifiable risk factors in Canada: Summary of results. Prev Med. 2019;122:140-7.
- [CrossRef] [PubMed] [Google Scholar]
- Proportion of cancers attributable to major lifestyle and environmental risk factors in the Eastern Mediterranean region. Int J Cancer. 2020;146:646-56.
- [CrossRef] [PubMed] [Google Scholar]
- Appraising the quality of medical education research methods: The medical education research study quality instrument and the newcastle-ottawa scale-education. Acad Med. 2015;90:1067-76.
- [CrossRef] [PubMed] [Google Scholar]
- Another side of the association between body mass index (BMI) and clinical outcomes of cancer patients receiving programmed cell death protein-1 (PD-1)/programmed cell death-ligand 1 (PD-L1) checkpoint inhibitors: A multicentre analysis of immune-related adverse events. Eur J Cancer. 2020;128:17-26.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous Update Project Expert Report 2018. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective (the third expert report). https://www.wcrf.org/diet-and-cancer/ World Cancer Research Fund International. Continuous Update Project Expert Report 2018. http://dietandcancerreport.org. (World Cancer Research Fund International. Diet, nutrition, physical activity and cancer: A global perspective (the third expert report): 2018) (Accessed December 12, 2021).
- Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism. 2019;92:121-35.
- [CrossRef] [PubMed] [Google Scholar]
- Intentional weight loss and endometrial cancer risk. J Clin Oncol. 2017;35:1189-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Body fatness at a young age and risks of eight types of cancer: Systematic review and meta-analysis of observational studies. Obes Rev. 2018;19:1385-94.
- [CrossRef] [PubMed] [Google Scholar]
- Young adulthood body mass index, adult weight gain and breast cancer risk: The PROCAS study (United Kingdom) Br J Cancer. 2020;122:1552-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mechanisms linking excess adiposity and carcinogenesis promotion. Front Endocrinol (Lausanne). 2014;5:65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prognostic value of vascular endothelial growth factor expression in patients with lung cancer: A systematic review with meta-analysis. J Thorac Oncol. 2009;4:1094-103.
- [CrossRef] [PubMed] [Google Scholar]
- Television viewing and time spent sedentary in relation to cancer risk: A meta-analysis. J Natl Cancer Inst. 2014;106:dju098.
- [CrossRef] [PubMed] [Google Scholar]
- Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6:e1077-e1086. Erratum in: Lancet Glob Health 2019;7:e36
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity in cancer prevention and survival: A systematic review. Med Sci Sports Exerc. 2019;51:1252-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Associations of leisure-time physical activity and television viewing with life expectancy cancer-free at age 50: The ARIC study. Cancer Epidemiol Biomarkers Prev. 2020;29:2617-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leisure sedentary behavior and risk of lung cancer: A two-sample mendelian randomization study and mediation analysis. Front Genet. 2021;12:763626.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: A prospective cohort study. Am J Clin Nutr. 2015;101:558-69.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global action plan on physical activity 2018–2030: More active people for a healthier world. Geneva: World Health Organization; 2018. (Accessed January 18, 2022)
- How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. Publications and reports of the surgeon general. (Accessed March 10, 2022)
- Tobacco smoke and involuntary smoking. IARC Monogr Eval Carcinog Risks Hum. 2004;83:1-1438.
- [PubMed] [PubMed Central] [Google Scholar]
- The health consequences of smoking: A report of the surgeon general. Atlanta, GA: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2014. (Accessed March 18, 2022)
- Cancer incidence and cancer death in relation to tobacco smoking in a population-based Australian cohort study. Int J Cancer. 2021;149:1076-88.
- [CrossRef] [PubMed] [Google Scholar]
- Strong excess risk of pancreatic cancer for low frequency and duration of cigarette smoking: A comprehensive review and meta-analysis. Eur J Cancer. 2018;104:117-26.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity estimates. Geneva: World Health Organization; 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (WHO, Geneva, 2020). (Accessed April 5, 2022)
- Alcohol and gastrointestinal cancers. Curr Opin Gastroenterol. 2019;35:107-13.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol use and cancer in the European union. Eur Addict Res. 2021;27:1-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Research opportunities for cancer associated with indoor air pollution from solid-fuel combustion. Environ Health Perspect. 2012;120:1495-98.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J Clin. 2020;70:460-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Contribution of long-term exposure to outdoor black carbon to the carcinogenicity of air pollution: Evidence regarding risk of cancer in the Gazel cohort. Environ Health Perspect. 2021;129:37005.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Multi-pollutant modeling through examination of susceptible subpopulations using profile regression. Curr Environ Health Rep. 2018;5:59-69.
- [CrossRef] [PubMed] [Google Scholar]
- IARC Monographs Volume 109: Outdoor Air Pollution. IARC Monogr Eval Carcinog Risks Hum, 109. International Agency for Research on Cancer, Lyon 9–444. https://monographs.iarc.fr/iarc-monographs-on-the-evaluationof-carcinogenic-risks-to-humans-7/. (2016). (Accessed April 8, 2022).
- Association between outdoor air pollution and risk of malignant and benign brain tumors: The multiethnic cohort study. JNCI Cancer Spectrum. 2020;4:pkz107.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- International agency for research on cancer monograph working group IARC. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14:1262-3.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term low-level ambient air pollution exposure and risk of lung cancer – A pooled analysis of 7 European cohorts. Environ International. 2021;146:106249.
- [CrossRef] [PubMed] [Google Scholar]
- Association between red meat consumption and colon cancer: A systematic review of experimental results. Exp Biol Med (Maywood). 2017;242:813-39.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: A comparative risk assessment. Lancet Glob Health. 2019;7:e257-e269.
- [CrossRef] [PubMed] [Google Scholar]
- Association of changes in red meat consumption with total and cause specific mortality among US women and men: Two prospective cohort studies. BMJ. 2019;365:l2110.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dietary patterns in association to cancer incidence and survival: Concept, current evidence, and suggestions for future research. Eur J Clin Nutr. 2018;72:818-25.
- [CrossRef] [PubMed] [Google Scholar]
- Concentrations and dietary exposure to polycyclic aromatic hydrocarbons (PAHs) from grilled and smoked foods. Food Control. 2011;22:2028-35.
- [Google Scholar]
- American cancer society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020;70:245-71.
- [CrossRef] [PubMed] [Google Scholar]
- 2016. Available from: Cancer Prevention Recommendations | WCRF International. (Accessed April 12, 2022)
- w-3 and w-6 polyunsaturated fatty acids, obesity and cancer. Nutrients. 2020;12:2751.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Updated review on green tea polyphenol epigallocatechin-3-gallate as a cancer epigenetic regulator. Semin Cancer Biol. 2022;83:335-52.
- [CrossRef] [PubMed] [Google Scholar]
- Association between dietary intake and risk of ovarian cancer: A systematic review and meta-analysis. Eur J Nutr. 2021;60:1707-36.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oxidative stress and dietary phytochemicals: Role in cancer chemoprevention and treatment. Cancer Lett. 2018;413:122-34.
- [CrossRef] [PubMed] [Google Scholar]
- Anti-cancer effects of green tea polyphenols against prostate cancer. Molecules. 2019;24:193.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Phytochemicals in skin cancer prevention and treatment: An updated review. Int J Mol Sci. 2018;19:941.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Environmental causes of cancer: Endocrine disruptors as carcinogens. Nat Rev Endocrinol. 2010;6:363-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Endocrine-disrupting effects of bisphenols on urological cancers. Environ Res. 2021;195:110485.
- [CrossRef] [PubMed] [Google Scholar]
- Endocrine disrupting chemicals and thyroid cancer: An overview. Toxics. 2021;9:14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Paraben content in adjacent normal-malignant breast tissues from women with breast cancer. Biomed Environ Sci. 2019;32:893-904.
- [CrossRef] [PubMed] [Google Scholar]
- Progression of breast cancer cells was enhanced by endocrine-disrupting chemicals, triclosan and octylphenol, via an estrogen receptor-dependent signaling pathway in cellular and mouse xenograft models. Chem Res Toxicol. 2014;27:834-42.
- [CrossRef] [PubMed] [Google Scholar]
- Untangling the association between environmental endocrine disruptive chemicals and the etiology of male genitourinary cancers. Biochem Pharmacol. 2020;172:113743.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5:374-81.
- [CrossRef] [PubMed] [Google Scholar]
- Depression’s multiple comorbidities explained by (neuro) inflammatory and oxidative and nitrosative stress pathways. Neuroendocrinol Lett. 2011;32:7-24.
- [PubMed] [Google Scholar]
- Oxidative DNA base modifications as factors in carcinogenesis. Acta Biochim Pol. 1998;45:561-72.
- [PubMed] [Google Scholar]
- Expression of 8-hydroxy-2¢-deoxyguanosine in chronic liver disease and hepatocellular carcinoma. Liver Int. 2003;23:338-45.
- [CrossRef] [PubMed] [Google Scholar]
- Antioxidant potential of vitamins A, E and C in modulating oxidative stress in rat brain. Clin Chimica Acta. 2004;340:229-33.
- [CrossRef] [PubMed] [Google Scholar]
- Free radicals in biology and medicine (5th Edition). United Kingdom: Oxford University Press; 2015.
- Lifestyle, oxidative stress, and antioxidants: Back and forth in the pathophysiology of chronic diseases. Front Physiol. 2020;11:694.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The inner clock-blue light sets the human rhythm. J Biophotonics. 2019;12:e201900102.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci USA. 2015;112:1232-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rotating night shift work and risk of ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2011;20:934-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Melatonin and associated signaling pathways that control normal breast epithelium and breast cancer. J Mammary Gland Biol Neoplasia. 2011;16:235-45.
- [CrossRef] [PubMed] [Google Scholar]
- UV-induced DNA damage, repair, mutations and oncogenic pathways in skin cancer. J Photochem Photobiol B. 2001;63:19-27.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep. 2015;5:11325.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effects of blue light on the circadian system and eye physiology. Mol Vis. 2016;22:61-72.
- [PubMed] [PubMed Central] [Google Scholar]
- Lipofuscin: A key compound in ophthalmic practice. Rom J Ophthalmol. 2021;65:109-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evaluating the association between artificial light-at-night exposure and breast and prostate cancer risk in Spain (MCC-Spain study) Environ Health Perspec. 2018;126:047011.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association between outdoor light-at-night exposure and colorectal cancer in Spain. Epidemiology. 2020;31:718-27.
- [CrossRef] [PubMed] [Google Scholar]
- Unrestricted evening use of light-emitting tablet computers delays self-selected bedtime and disrupts circadian timing and alertness. Physiol Rep. 2018;6:e13692.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sleep deprivation and cellular responses to oxidative stress. Sleep. 2004;27:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- Free radicals, antioxidants in disease and health. Int J Biomed Sci. 2008;4:89-96.
- [PubMed] [PubMed Central] [Google Scholar]
- Endogenous melatonin and oxidatively damaged guanine in DNA. BMC Endocr Disord. 2009;9:22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Melatonin anticancer effects: Review. Int J Mol Sci. 2013;14:2410-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Melatonin: A versatile protector against oxidative DNA damage. Molecules. 2018;23:530.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- On the free radical scavenging activities of melatonin’s metabolites, AFMK and AMK. J Pineal Res. 2013;54:245-57.
- [CrossRef] [PubMed] [Google Scholar]
- Role of glutathione, lipid peroxidation and antioxidants on acute bile-duct obstruction in the rat. Biochim Biophys Acta. 1999;1472:173-80.
- [CrossRef] [PubMed] [Google Scholar]
- Melatonin in cancer treatment: Current knowledge and future opportunities. Molecules. 2021;26:2506.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Role and therapeutic potential of melatonin in various type of cancers. Onco Targets Ther. 2021;14:2019-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Molecular deficiency(ies) in MT1 melatonin signaling pathway underlies the melatonin-unresponsive phenotype in MDA-MB-231 human breast cancer cells. J Pineal Res. 2014;56:246-53.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Melatonin as an antioxidant: Under promises but over delivers. J Pineal Res. 2016;61:253-78.
- [CrossRef] [PubMed] [Google Scholar]
- Melatonin, a full service anti-cancer agent: Inhibition of initiation, progression and metastasis. Int J Mol Sci. 2017;18:843.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: A review. J Pineal Res. 2014;56:225-37.
- [CrossRef] [PubMed] [Google Scholar]
- Melatonin-mediated Bim up-regulation and cyclooxygenase-2 (COX-2) down-regulation enhances tunicamycin-induced apoptosis in MDA-MB-231 cells. J Pineal Res. 2015;58:310-20.
- [CrossRef] [PubMed] [Google Scholar]
- Shift work and cancer - considerations on rationale, mechanisms, and epidemiology. Scand J Work Environ Health. 2010;36:163-79.
- [CrossRef] [PubMed] [Google Scholar]
- Circulating melatonin and the risk of breast and endometrial cancer in women. Cancer Lett. 2009;281:1-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Painting, firefighting, and shiftwork. IARC Monogr Eval Carcinog Risks Hum. 2010;98:9-764.
- [PubMed] [PubMed Central] [Google Scholar]
- Tobacco use and cancer: An epidemiologic perspective for geneticists. Oncogene. 2002;21:7307-25.
- [CrossRef] [PubMed] [Google Scholar]
- Personal habits and indoor combustions. IARC Monogr Eval Carcinog Risks Hum. 2012;100:1-538.
- [PubMed] [PubMed Central] [Google Scholar]
- Exposure to chewing tobacco promotes primary oral squamous cell carcinoma and regional lymph node metastasis by alterations of SDF1a/CXCR4 axis. Int J Exp Pathol. 2021;102:80-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cancer incidence and cancer death in relation to tobacco smoking in a population‐based Australian cohort study. Int J Cancer. 2021;149:1076-88.
- [CrossRef] [PubMed] [Google Scholar]
- Red and processed meat consumption and cancer outcomes: Umbrella review. Food Chem. 2021;356:129697.
- [CrossRef] [PubMed] [Google Scholar]
- Fruit and vegetable intake and liver cancer risk: A meta-analysis of prospective cohort studies. Food Funct. 2019;10:4478-85.
- [CrossRef] [PubMed] [Google Scholar]
- Revisit dietary fiber on colorectal cancer: Butyrate and its role on prevention and treatment. Cancer Metastasis Rev. 2015;34:465-78.
- [CrossRef] [PubMed] [Google Scholar]
- The associations of fruit and vegetable intakes with burden of diseases: A systematic review of meta-analyses. J Acad Nutr Diet. 2019;119:464-81.
- [CrossRef] [PubMed] [Google Scholar]
- The world cancer research fund/american institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: Impact and future directions. J Nutr. 2020;150:663-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br J Pharmacol. 2019;177:1241-57.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Omega-3 polyunsaturated fatty acids and cancer: Lessons learned from clinical trials. Cancer Metastasis Rev. 2015;34:359-80.
- [CrossRef] [PubMed] [Google Scholar]
- Interaction of green tea catechins with breast cancer endocrine treatment: A systematic review. Pharmacology. 2014;94:245-8.
- [CrossRef] [PubMed] [Google Scholar]
- Green tea and cancer and cardiometabolic diseases: A review of the current epidemiological evidence. Eur J Clin Nutr. 2021;75:865-76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Therapeutic role of green tea in obesity and cancer. In: Kumar S, Gupta S, eds. Obesity and cancer. Singapore: Springer; 2021. p. :143-64.
- [Google Scholar]
- Physical activity and weight loss reduce the risk of breast cancer: A meta-analysis of 139 prospective and retrospective studies. Clin Breast Cancer. 2018;18:e601-12.
- [CrossRef] [PubMed] [Google Scholar]
- World health organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. 2020;54:1451-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Physical activity, sedentary behaviour, diet, and cancer: An update and emerging new evidence. Lancet Oncol. 2017;18:e457-e471.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Preliminary evidence on the effects of exercise on tumor biology: A potential guide for prescribing exercise. Curr Physical Med Rehabilitation Rep. 2021;9:136-41.
- [Google Scholar]
- Amount and intensity of leisure-time physical activity and lower cancer risk. J Clin Oncol. 2020;38:686-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health and economic benefits of building ventilation interventions for reducing indoor PM2.5 exposure from both indoor and outdoor origins in urban Beijing, China. Sci Total Environ. 2018;626:546-54.
- [CrossRef] [PubMed] [Google Scholar]
- Spatial association between outdoor air pollution and lung cancer incidence in China. BMC Public Health. 2019;19:1377.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The molecular mechanisms of action of the endocrine disrupting chemical bisphenol A in the development of cancer. Gene. 2018;647:235-43.
- [CrossRef] [PubMed] [Google Scholar]
- Phthalate exposure and breast cancer incidence: A danish nationwide cohort study. J Clin Oncol. 2019;37:1800-09.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exposure to endocrine disrupting chemicals and risk of breast cancer. Int J Mol Sci. 2020;21:9139.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nutrients and the pancreas: An epigenetic perspective. Nutrients. 2017;9:283.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Molecular signature of the immune response to yoga therapy in stress-related chronic disease conditions: An insight. International journal of yoga. 2020;13:9-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- What is the molecular signature of mind-body interventions? A systematic review of gene expression changes induced by meditation and related practices. Front Immunol. 2017;8:670.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Stress and cancer. Part II: Therapeutic implications for oncology. J Neuroimmunol. 2020;346:577312.
- [CrossRef] [PubMed] [Google Scholar]
- Stress and cancer: Mechanisms, significance and future directions. Nat Rev Cancer. 2021;21:767-85.
- [CrossRef] [PubMed] [Google Scholar]
- Disruption of adolescents’ circadian clock: The vicious circle of media use, exposure to light at night, sleep loss and risk behaviors. J Physiol Paris. 2016;110:467-79.
- [CrossRef] [PubMed] [Google Scholar]






