Translate this page into:
Influence of`COVID infection or vaccination on pregnancy outcome
*Corresponding author: Shreya Satheesh, Department of Medical Genetics, Apollo Proton Cancer Centre, Chennai, India. shreyasatheesh2011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Satheesh S, Tadikonda S, Jitta S, Hasan A. Influence of COVID infection or vaccination on pregnancy outcome. Ann Natl Acad Med Sci (India). 2024;60:197-200. doi: 10.25259/ANAMS-2023-10-1-(1035)
Abstract
Objectives
The study aimed to assess the effect of Covid infection or Vaccination on pregnancy outcomes.
Material and Methods
Infection and vaccination status of 372 women were collected during the pandemic period (March 2020 to March 2022) from medical records and personal interviews of pregnant women visiting two hospitals for antenatal care and through a survey form circulated online. Seventy-eight women were still on follow-up during the study.
The women were categorized into (i) Infected during gestation, (ii) Vaccinated before pregnancy, (iii) Vaccinated during pregnancy, (iv) Vaccinated after delivery (v) unvaccinated. Individuals in (iv) and (v) categories were taken as controls.
Results
Thirty-six women were infected during gestation, 156 were vaccinated before/during pregnancy, and 180 were kept as controls The result showed that 35 individuals from the sample size had adverse pregnancy outcomes such as Spontaneous abortions, MTPs (Carried out after an ultrasound detected abnormality), and Intrauterine deaths, 4 of them were infected and 23 were vaccinated before/ during pregnancy, and 8 were the controls, indicating that 77% of individuals with adverse pregnancy outcomes were exposed to either virus/vaccination. Eighty-nine women had mild complications during pregnancy, such as Oligo/Polyhydramnios, Abnormal USG, and biochemical markers. 56.1% of these individuals were exposed to the virus or vaccination, slightly higher than the control group.
Conclusion
In this preliminary follow-up study, an association was seen between SARS-CoV-2 infection, COVID-19 vaccination, and adverse pregnancy outcomes.
Keywords
Adverse pregnancy outcomes
Covid
Covid vaccination
Miscarriage
Pregnancy
INTRODUCTION
Covid-19 is a disease caused by a novel virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was first identified amid an outbreak of respiratory illness in Wuhan City, China. SARS-CoV-2 is a member of the coronavirus family, Coronaviridae, which includes other viruses that cause the common cold, Middle East respiratory syndrome (MERS), and severe acute respiratory syndrome (SARS).
Cases of Covid-19 were reported in India from the last week of January 2020. The government imposed a nationwide lockdown in March 2020 to curb the spread of the SARS-CoV-2 virus. The number of cases in each state varied with international traffic, inter and intra-state migration, and population density of the state, and districts. Case fatality and recovery were different based on population composition and the status of health services, including the vaccination drive.1
SARS-CoV-2 as a teratogen
Several viruses are known to be teratogenic in humans, such as Zika, cytomegalovirus, Rubella, and herpes simplex. The growing risk of pandemics is making it essential for us to understand the role of viral infections and vaccinations during pregnancy, as these may significantly affect the pregnant mother as well as the fetus. There is substantial epidemiologic evidence that pregnant women are at higher risk of severe illness and mortality from viral infections and that these may predispose them to spontaneous abortions, preterm labor, and congenital anomalies.2
The effect of COVID infection on the unborn fetus during pregnancy is still poorly understood. However, there have been anecdotal reports of women infected with the virus during pregnancy, resulting in fetal distress. A study by Wong et al (2004),3 on the effect of SARS on pregnancy outcomes revealed that the women who were infected with the virus during their gestation either had a first-trimester spontaneous abortion, delivered preterm, or the pregnancies were complicated by IUGR(Intra Uterine Growth Reduction).
Vaccination during pregnancy
Maternal immunization provides benefits to both pregnant mothers and fetuses. Immunization during pregnancy directly protects the fetus by transferring the antibodies from the mother to the fetus. Some vaccines, such as the ones for hepatitis A or B or the influenza virus, are safe to receive before and during pregnancy. Other vaccinations, such as the ones for chickenpox or Rubella, contain weakened but live versions of the virus/bacteria and are best given at least a month before a woman conceives.4
The effect of the COVID-19 Vaccine on the developing fetus has not been characterized. The Centers for Disease Control and Prevention (CDC), The American College of Obstetricians and Gynecologists (ACOG) and Society for Maternal - Fetal Medicine (SMFM) say the Food and Drug Administration (FDA) has authorized COVID-19 vaccines for pregnant and/or lactating women since June 2021. The World Health Organization believes that the pros of vaccination during pregnancy outweigh the cons.
The present observational study assessed the effect of the SARS-CoV2 infection and COVID-19 vaccination before and during gestation on pregnancy outcomes during the pandemic.
MATERIAL AND METHODS
All pregnant women who attended the Out Patient (OP) and In Patient (IP) Department of three hospitals (two urban and one rural) from March 2020 to March 2022 were included in this study.
Data from the Radiology Department during the same period was also assessed for identifying abnormal cases through routine antenatal scans—nuchal translucency (NT) and Targeted imaging for fetal aneuploidies (TIFFA) at 11-13th weeks and 18-22 weeks, respectively.
Information was also collected by interviewing pregnant women who were currently visiting the Obstetric and Gynaecology outpatient (OBG OP) department, women in the labor room for delivery, and those who came to collect reports of Newborn Screening.
Information about COVID-19 virus infection and COVID-19 vaccination for antenatal cases during the COVID-19 period was collected from the Medical Records.
A survey form with the questions mentioned in the annexure was circulated on social media, targeting pregnant women during the COVID period and not associated with our hospitals (From March 2020 to March 2022) to increase the number of cases.
Individuals who got vaccinated after delivery and those who remained unvaccinated were kept as the controls for this study.
RESULTS
As they informed, the 372 pregnant women included in the study were categorized according to their Viral infection status based on RT- PCR or Rapid Antigen test and Vaccination status.
They were grouped into the following five categories.
-
Women infected with the virus before or during their gestation (n = 36).
-
Women who took the Covid vaccine less than 3 months before conception (n = 69).
-
Women who took the Covid vaccine during pregnancy (n = 87).
-
Women who took the Covid vaccine after delivery (these included individuals who took the Covid vaccine while/after breastfeeding, after a miscarriage/Termination of pregnancy) (n = 99)
-
Women who were unvaccinated (n = 81)
36 women out of the 372 included in the study individuals were infected with the virus during their gestation. Ten were asymptomatic, while 26 had cough, cold, high-grade fever, body pain, etc.
Further into the study, the sample size was categorized according to their term of delivery and adverse outcomes such as miscarriages/medically terminated pregnancies and intra uterine death (IUD). The individuals who were unvaccinated and the individuals who took the vaccine after delivery were kept as controls.
At the time of data collection’s completion, 78 individuals were still pregnant. Therefore, the analysis was carried out based on the remaining 294 individuals.
The infection or vaccination status does not affect the term of delivery. However, adverse outcomes like Medical Termination of Pregnancy (MTP) (Carried out after an ultrasound detected abnormality) and Spontaneous Abortions (SA) in individuals who were vaccinated before or during pregnancy were higher, while infection during pregnancy did not result in adverse outcomes.
Other complications such as oligohydramnios, polyhydramnios, Increased NT, Abnormal TIFFA, and Abnormal biochemical marker tests were observed in 89/372 (23.7%) individuals.
A higher number of women who took vaccination either before or during pregnancy had increased NT compared to the controls. All other complications were lower than the controls.
DISCUSSION
Viruses have long been studied for their teratogenicity. Viruses like Herpes, CMV, Rubella, etc., have been known to cause preterm births and congenital disabilities such as microcephaly, ocular abnormalities, hearing defects, and neural tube defects, among others.5 The vaccination in pregnant women was studied separately for these viruses. Some types of vaccines are considered unsafe for pregnant women. Hence, vaccination during gestation and lactation is avoided. COVID-19 vaccine was offered to women from July 2021 without prior testing and was released into the market immediately.
The teratogenicity of SARS- CoV2 virus has been the subject of several papers, and the meta-analysis by Zaigham and Andersson (2020)6 based on 108 pregnancies exhibited evidence that there may be vertical transmission of SARS-CoV 2 virus. A more recent meta-analysis on a larger sample of 4,38,548 pregnant women showed that COVID-19 may be associated with increased risks of preeclampsia, preterm birth, and other adverse pregnancy outcomes (Wei et al., 2021)7.
In this study, out of 372 pregnant women of different stages of gestation, 294 were individually followed up during the pandemic until delivery. Seventy-eight still had an ongoing pregnancy at the time of the end of data collection. Among these, 36 (9.7%) women were RT-PCR positive and considered infected with the virus during their gestation. 10/36 (27.7%) were asymptomatic, 26/36 (72.3%) had symptoms like cough, cold, fever, and body pains, and none had severe symptoms requiring hospitalization. However, it was noted that one of the individuals who was infected with the virus in her second trimester developed Bell’s palsy during her third trimester. According to other reports also, the clinical presentations of COVID-19 in pregnant women were not very severe and were similar to that seen in the general population8,9
We categorized the pregnant women into four groups [Figure 1] and considered those who were not infected or vaccinated after delivery as controls (n = 180). The results indicate that most deliveries were full-term (89.2%). However, the percentage of women who had a pre-term delivery after getting infected or vaccinated during pregnancy was the same [Table 1], and this percentage was lower than the controls. Adverse outcomes like MTP (Carried out after an ultrasound detected abnormality) and SA were seen in all four categories but were highest in women who were vaccinated before or during pregnancy, and the lowest frequency was in those who were infected during pregnancy [Table 1]. Other complications like oligohydramnios, polyhydramnios, Increased NT, Abnormal TIFFA, and Abnormal biochemical marker tests were observed in 89/372 (23.7%) individuals [Table 2]. However, none of the complications except increased NT had a higher frequency of occurrence when compared to the control. A review of COVID-19 vaccines in pregnancy reported that the vaccine is safe and it effectively protects them against the disease.9 This paper only focuses on the fetal outcomes and does not include maternal aspects such as gestational diabetes and pre-eclampsia. The adverse fetal outcomes (if any) recorded in the sample size 372 have been categorized and analyzed according to their infection and vaccination statuses.
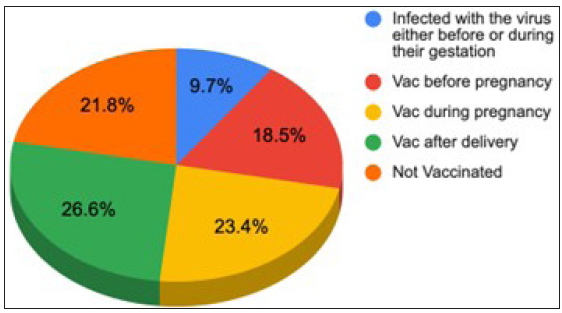
- Pie chart representing women included in the study categorized according to their infection and vaccination (Vac) status.
| Type | Number of individuals | Delivered | Adverse pregnancy outcomes | |||
|---|---|---|---|---|---|---|
| Total | 294 | 259 | 35 (11.9%) | |||
| Full term (231) | Preterm (28) | MTP (18) | SA (13) | IUD (4) | ||
| Infected during pregnancy | 32 | 24 (10.4%) | 4 (14.3%) | 3 (16.7%) | 1 (7.7%) | 0 |
| VAC before pregnancy | 36 | 22 (9.5%) | 0 | 6 (33.3%) | 6 (46.1%) | 2 (50%) |
| VAC during pregnancy | 66 | 53 (23%) | 4 (14.3%) | 5 (27.8%) | 4 (30.8%) | 0 |
| VAC after deliver Y+ not vaccinated | 160 | 132 (57.1%) | 20 (71.4%) | 4 (22.2%) | 2 (15.4%) | 2 (50%) |
MTP: Medical termination of pregnancy, SA: Spontaneous abortions, IUD: Intra uterine death.
| Type | Oligohydramnios | Polyhydramnios | Increased NT | Abnormal TIFFA | Abnormal biochemical markers |
|---|---|---|---|---|---|
| Total number of individuals | 21 | 2 | 12 | 35 | 19 |
| Infected during pregnancy | 3 (14.3%) | 1 (50%) | 0 | 8 (22.8%) | 6 (31.5%) |
| VAC before pregnancy | 1 (4.8%) | 0 | 5 (41.7%) | 7 (20%) | 3 (15.7%) |
| VAC during pregnancy | 4 (19%) | 0 | 4 (33.3%) | 6 (17.2%) | 2 (10.5%) |
| VAC after delivery + not vaccinated | 13 (61.9%) | 1 (50%) | 3 (25%) | 14 (40%) | 8 (42.3%) |
TIFFA: Targeted imaging for fetal anomalies, VAC: Vaccinated, NT: Nuchal translucency.
Therefore, this follow-up study of pregnant women during the COVID-19 pandemic exhibited that the symptoms of infection during gestation were not different from those seen in the general population. Pre-term deliveries in controls were higher; this may be because the norms for antenatal management were altered during this period. However, the same percentage of pre-term deliveries were seen in both women infected or vaccinated during pregnancy, suggesting that both interventions have similar effects. MTP (Carried out after an ultrasound detected abnormality) and SA were higher in women getting vaccinated before or during pregnancy compared to those infected during pregnancy. The two IUDs were also seen in women who were vaccinated before pregnancy. This is unlike some studies demonstrating that vaccination did not affect pregnancy outcomes.
CONCLUSION
We believe that caution is required before vaccinating women of reproductive age, especially those planning a pregnancy.
Acknowledgements
Thank you Dr. Annie Hasan for your support and guidance. Thank you, Dr. Aruna Priya and Ms. Nandini Shyamali Bora for your patience and constant encouragement. Thank you Dr. Menaka, HOD of Obstetrics and Gynecology, Kamineni Hospitals. Lastly, thanks to the participants of this survey.
Ethical approval
Institutional Review Board approval is not required as it is a retrospective study.
Declaration of patient consent
Patient consent not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that no artificial intelligence (AI)- assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
REFERENCES
- COVID-19 pandemic in India: A Comparison of pandemic pattern in selected States. Nepal J Epidemiol. 2020;10:856-64.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Viral infections during pregnancy. Am J Reprod Immunol. 2015;73:199-213.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191:292-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vaccinations for pregnant women. Obstet Gynecol. 2015;125:212-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Altered bivalent positioning in metaphase I human spermatocytes from Robertsonian translocation carriers. J Assist Reprod Genet. 2017;34:131-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020;99:823-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. Cmaj. 2021;193:E540-E548.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company ‘ s public news and information . 2020;(January)
- Clinical presentation and outcomes of pregnant women with coronavirus disease 2019: A systematic review and meta-analysis. Clin Infect Dis. 2021;72:521-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





