NAMS task force report on Obesity and lifestyle diseases in India
BACKGROUND
India's health landscape is shifting dramatically. Rapid economic and social changes are leading to a rise in chronic diseases, often called non-communicable diseases (NCDs). These conditions, like heart disease and diabetes, are now the top killers in India, affecting adults much earlier than in developed countries. While NCDs typically strike people over 55 in wealthier nations, Indians are experiencing them a decade sooner, around age 45 or older. This trend highlights the urgent need for India to address the growing burden of NCDs.
Magnifying this problem are the issues of multiple chronic conditions and the fact that many remain undiagnosed due to a lack of awareness and insufficient healthcare access. Rapid urbanization and industrialization drives the rising burden of NCDs that are characterized by the uptake of unhealthy lifestyles such as tobacco and alcohol use, physical inactivity, and unhealthy diet. The Global Burden of Disease study (Indian estimates) reports blood pressure as one of the three leading risk factors for national disease burden. In India, the prevalence of various NCDs and its risk factors shows wide variations across geographic regions. Although the NCD burden has grown, India still does not have sufficiently detailed data on NCDs for research and policy purposes. Therefore, NAMS constituted this Task Force (TF) on Obesity and Lifestyle Diseases for situational analysis and future directives.
TF targeted obesity, diabetes, hypertension, dyslipidemia, metabolic syndrome, and NAFLD in this document, as these lifestyle disorders are the major cause for morbidity and mortality and are responsible for various other lifestyle diseases like cardiovascular and cerebrovascular diseases, cancers, chronic liver disease, etc.
TERMS OF REFERENCE (TORS) FOR THE TASK FORCE
The Executive Council of the National Academy of Medical Sciences assigned the following terms of reference for the TF on Obesity and Lifestyle Diseases in June 2022:
The task force (TF) was required to make recommendations to the GOI for prevention and control of obesity and lifestyle diseases in India at the health policy and implementation levels.
The TF would prepare a “White Paper,” which may include the existing morbidity and mortality status due to obesity and lifestyle diseases.
The TF would identify existing lacunae and deficiencies in the thematic area and make recommendations to address these.
METHODOLOGY
The TF conducted meetings using a virtual platform, and focused group discussions were held. In addition, the chairperson and members co-opted expert members as and when required to facilitate the discussions. Through a process of frequent discussions on the virtual mode, consensus was reached amongst the members of the TF, on the methodology to be adopted for developing the guidelines. The task at hand was divided into sections, and members allocated the sections based on their specific domain expertise.
The relevant technical documents, published papers, reports, and various national and state guidelines were used as background materials. An extensive literature review was undertaken using the websites PubMed, Scopus, Embase, and Google Scholar using the search terms “Obesity” OR “Dyslipidemia,” OR “Hypertension,” OR “Diabetes” OR “Metabolic Syndrome” “NAFLD” AND “Epidemiology” AND “India” for English language documents, with a preference for Original Articles, Review articles, Clinical Trials, Consensus Statements, and Guidelines. Professional Society websites were browsed for the latest guidelines and consensus statements. Thus, almost all published works from India were reviewed. A synthesis of the obtained literature was prepared and deliberated upon by the TF.
The key recommendations were arrived at by consensus of the members based on their expertise and experience.
A series of weekly meetings were conducted in virtual mode for reviewing the progress being made and to discuss the allocated sections of the White Paper. Minutes of the meetings were prepared and circulated within the TF for information and guidance.
While developing the document, the Problem/Patients, Intervention, Comparison/Control, Outcome (PICO) framework was relied upon to define the various at-risk patient groups and recommend the interventions required. Iterations of the document developed with the contributions of the members were circulated and discussed sequentially over the term of the TF. This modification of the Delphi technique was essential for the process of eventual consensus, as the guidelines required reference to the latest evidence and conformity with professional society guidelines, keeping in view the requirements of the country and the best interests of the patient population.
CURRENT SITUATION OF OBESITY AND LIFESTYLE DISEASES IN INDIA
Magnitude of obesity and lifestyle diseases in India
Obesity is defined as a disease process characterized by excessive body fat accumulation with multiple organ-specific consequences.1 There are two ingredients integral to this definition: (i) excess body fat and (ii) multiple organ-specific consequences. Several morbidities can be associated with the presence of excess fat. Obesity contributes to or worsens allergic airway disease, cancers, degenerative diseases, inflammatory diseases, heart and cerebrovascular diseases, diabetes, fertility issues, and also sleep disorders, and psychiatric morbidities. Therefore, the consequences can be troublesome and disastrous and can result in even increased mortality. Hence, there is an urgent need to control excess fat and maintain body weight.
As per the WHO Asia-Pacific criteria, overweight is defined as a body mass index (BMI) ≥23 kg/m2 but <25 kg/m2 for both genders with or without abdominal obesity (AO). Generalized obesity (GO) is defined as a BMI ≥25 kg/m2 for both genders with or without AO. AO is defined as a waist circumference (WC) ≥90 cm for men and ≥80 cm for women with or without GO. Isolated generalized obesity (IGO) is defined as a BMI ≥25 kg/m2 with WC of <90 cm in men and <80 cm in women. Isolated abdominal obesity (IAO) is defined as a WC of ≥90 cm in men or ≥80 cm in women with a BMI <25 kg/m2. Combined obesity (CO) refers to individuals with both GO and AO. Non-obese subjects refer to individuals without either GO or AO.2
Magnitude of Obesity - World including India
The 2016 Global Nutrition Report states that the rates of overweight/obese people are rising in every region of the world and in nearly every country. The global adult obesity prevalence is 13% as against 4.9% in India, and for overweight, the prevalence is 39% global and 22% for India, virtually indicating that one in four Indians has a weight problem of abundance. The World Health Organization (WHO) has declared obesity as the largest global chronic health problem in adults, which is increasingly turning into a more serious problem than malnutrition. Obesity is a gateway to ill health, and it has become one of the leading causes of disability and death, affecting not only adults but also children and adolescents worldwide. In 2014, more than 1.9 billion adults (18 years and older) were overweight. Of these, over 600 million were obese. Forty-two million children under the age of 5 were overweight or obese in 2013.3
Magnitude of obesity in India
In India, different geographical areas were studied for the prevalence of obesity. It was found that the prevalence of general obesity (GO) was 24.6%, 16.6%, 11.8%, and 31.3% among residents of Tamil Nadu (TN), Maharashtra (MH), Jharkhand (JH), and Chandigarh, respectively. The prevalence of AO was 26.6%, 18.7%, 16.9%, and 36.1% among residents of TN, MH, JH, and Chandigarh, respectively.
The survey conducted by National Family Health Survey-3 (NFHS-3) in India also found that obesity (BMI ≥25 kg/m2) was more prevalent in urban areas and in higher socioeconomic groups compared to rural areas, especially among women (Men - urban: 15.9 vs. rural: 5.6%; Women - urban: 23.5 vs. rural: 7.2%).4
A similar study from Jaipur called the “The Jaipur Heart Watch Study (I–IV)” showed that generalized and AO were significantly higher among the urban compared to the rural population.5 Pandey et al. studied middle-aged women in four urban and five rural areas and found that the prevalence of obesity in urban vs. rural was 45.6% vs. 22.5% and AO was 44.3% vs. 13.0%, respectively.6
In the Indian Council of Medical Research–India Diabetes (ICMR–INDIAB) study, it was found that women had higher mean BMI values than men (Urban: women: 23.6 vs. men: 22.7 kg/m2 and Rural: women: 21.2 vs. men: 20.9, kg/m2). However, mean WC values were higher in men than in women (Urban: women: 77.4 vs. men: 83.6 cm; Rural: women: 71.7 vs. men: 78.1 cm).
The Chennai Urban Rural Epidemiology Study (CURES) conducted in Chennai city of TN reported age-standardized prevalence of GO to be 45.9%, while that of AO was 46.6%. Isolated GO was found in 9.1% while isolated AO was reported in 9.7%.7
Magnitude of overweight in India
It was observed in ICMR–INDIAB study that overweight was more prevalent in urban population than rural population (Chandigarh region - 18.9 vs. 14.8%; TN region - 16.5 vs. 14.6%; JH - 12.4 vs. 5.7%; and MH region - 13.6 vs. 10.3%).
Magnitude of childhood obesity in India
The Centre for Disease Control has published tables for determining obesity in children. For children and adolescents (age 2–19 years), the BMI value is plotted on the Center for Disease Control (CDC) growth charts to determine the corresponding BMI-for-age percentile.
Overweight is defined as a BMI at or above the 85th percentile and lower than the 95th percentile
Obesity is defined as a BMI at or above the 95th percentile.8
In a meta-analysis of 9 studies done by Midha et al., it was estimated that the prevalence of obesity in children <18 years of age was 3.39%, and the prevalence of overweight was 12.64%.9
Diabetes mellitus in India
Diabetes mellitus (DM) is a chronic disease that occurs when the pancreas does not produce enough insulin (Type 1 DM) or when the body cannot effectively use the insulin it produces (Type 2 DM, T2DM). Hyperglycemia, or raised blood glucose, is a common effect of uncontrolled diabetes which over time leads to serious damage to many of the body’s systems, resulting in micro- and macro-vascular complications, including increased risk of coronary heart disease. TF mainly focused on T2DM as a lifestyle disorder.
Magnitude of diabetes in India
The burden of T2DM is high and increasing globally, and in developing economies like India, it is mainly fuelled by the increasing prevalence of overweight/obesity and unhealthy lifestyles. One estimate of International Diabetes Federation (IDF) in 2019 showed that 77 million individuals had diabetes in India, which is expected to rise to over 134 million by 2045.10 Approximately 57% of these individuals remain undiagnosed. The prevalence of diabetes in India has risen from 7.1% in 2009 to 8.9% in 2019.11 As per the National Family Health Survey (NFHS)-5 data in the 22 States/UTs, around 16.8% of the male adult population and 14.6% of the female adult population, on average, are estimated to be diabetic.12
Diabetes in children and adolescents
T2DM, which earlier used to be associated with adults, is now observed in children and adolescents as well. In a study done across various hospital and clinic-based registries, reviewed by Chowdhury and Ghosh, it was suggested that the percentage of type 1 diabetes in children is showing a declining trend. This implies that the prevalence of T2DM in children is rising.13 The earliest report of T2DM in children was from Madras (Chennai). In this study, 18 children with insidious onset of diabetes at age ≤15 years, response to oral glucose-lowering drugs (preserved C peptide levels [≥ 1.82 pg/mL]) and absence of decarboxylase 65 (glutamic acid decarboxylase 65) antibodies were reported. T2DM in children is gradually being reported across the country, though the prevalence is not as high as in Asian countries such as Japan. At referral centers such as Lucknow and Chennai, the proportion of children with T2DM is reported as 12% and 26.7%, respectively.14
A large project (n = 1519) that was carried out in children aged 6–11 years from Chennai, found an overall prevalence of 3%–7% of glucose intolerance (4.2% in girls, 3.2% in boys; P < 0.001). The prevalence of dysglycemia, as assessed by the oral glucose tolerance test, was 12.7% in girls with AO. Upon multivariate analysis, a family history of diabetes was found to have a significant association with glucose intolerance in girls (odds ratio [OR], 4.11; 95% confidence interval [CI], 1.28–13.22; P = 0.018). Homeostasis model assessment-insulin resistance (HOMA-IR) was significantly associated with glucose intolerance in both boys (OR, 5.19; 95% CI, 1.54–17.44; P = 0.008) andgirls (OR, 11.22; 95% CI, 4.19–30.05; P < 0.001).15 The Comprehensive National Nutrition Survey, the first-ever nationally represented nutrition survey of children and adolescents in India used a sample size of 17,865 adolescent boys and 17,965 adolescent girls. The prevalence of pre-diabetes/diabetes was 12.3% and 8.4% among adolescent boys and girls in India, respectively. BMI and subscapular skinfold thickness were the two most important predictors of pre-diabetes/diabetes among adolescents. Further, physical activities show a negative association with pre-diabetes/diabetes. Moreover, interaction models in the present study clearly reveal the fact that adolescent girls were less likely to suffer from pre-diabetes/diabetes than adolescent boys. Additionally, it was found that the prevalence of pre-diabetes/diabetes was high among adolescent girls from lower socioeconomic strata.16,17 A recent study conducted in Kerala included 607 children in the study. 56.3% were males. Prevalence of pre-diabetes was 20.4% with a combination of Oral Glucose Tolerance Test (OGTT), Fasting Blood Sugar (FBS), and Hemoglobin A1C (HbA1c) tests. Prevalence by OGTT was 5.9%, HbA1c 4.1%, and FBS was 17.1%. A higher prevalence of pre-diabetes was associated with male gender, frequent consumption of junk foods, decreased physical activities, overweight, obesity, and high waist-to-hip ratio. A combination of FBS with Glucose Tolerance Test (GTT) and FBS with HbA1c had better sensitivity and specificity when compared to a combination of OGTT with HbA1c.18 In another multicentric study on school children of MH, Gujarat, Chhattisgarh, Assam, TN, and Punjab from 40 selected schools, data on 14,339 subjects (7413 boys) were analyzed. Prevalence of obesity was 5.8%, and overweight was 10.6%. Overall, 1% had low (<54 mg/dL), 93.7% in the reference range (70–130 mg/dL), and 5.3% had elevated Random Blood Glucose (RBG) (>130 mg/dL). With increasing mean BMI, there was an increase in RBG concentrations. Children from TN were more likely to have RBG outside the reference range compared to other regions (P < 0.05). Assam and Punjab had the highest prevalence of RBG and BMI within the reference range. Energy intake partly explained regional variations. Multivariate analysis showed male gender, urban residency, age >10 years (girls) and 13 years (boys), and overweight or obesity were predictive of pre-diabetes.19
Hypertension in India
The global prevalence of hypertension is estimated to be about 22%.20 The population in India is passing through an epidemiological transition with high rates of urbanization. This has led to economic improvement, the consequences of which are increased food consumption, tobacco use, and decreased physical activity.21 Recently concluded NFHS-5 found that 21% of women and 24% of men aged 15 years and above were suffering from hypertension [Table 1]. It also found that southern states have a higher prevalence of hypertension than the national average for both men as well as women. Apart from this, the study found that the prevalence of hypertension also increased sharply with age. Another striking feature of the NFHS-5 survey was that the prevalence of hypertension was higher among Sikhs (37% for men and 31% for women), Jains (30% for men and 25% for women), and Christians (29% for men and 26% for women) than the rest of the religions.12 In a study conducted by Ramakrishnan et al as a national survey with one-day blood pressure measurement camps across 24 states, it was found that the prevalence of hypertension was 30.7% (95% CI, 30.5–30.9). They found the prevalence to be higher among men as compared to women (34.2% vs. 23.7%).22 Another study conducted among young adults (20–39 years) in Kerala by Geevar et al., the prevalence of hypertension among the study population was 11.2%, while that of pre-hypertension was almost three times that of hypertension (33.2%). Other factors such as male gender, urban residence, hypercholesterolemia, and AO were also found to be statistically significant in association with hypertension in young adults.23
| States/Union Territories | Prevalence of hypertension (%) | |
|---|---|---|
| Women | Men | |
| India | 21.3 | 24.0 |
| Chandigarh | 25 | 30.6 |
| Delhi | 24.1 | 32.7 |
| Haryana | 21.0 | 25.1 |
| Himachal Pradesh | 22.2 | 24.4 |
| Jammu & Kashmir | 20.0 | 18.9 |
| Ladakh | 15.7 | 17.4 |
| Punjab | 31.2 | 37.7 |
| Rajasthan | 15.3 | 17.9 |
| Uttarakhand | 22.9 | 31.8 |
| Chhattisgarh | 23.6 | 27.7 |
| Madhya Pradesh | 20.6 | 22.7 |
| Uttar Pradesh | 18.3 | 21.7 |
| Bihar | 15.9 | 18.4 |
| Jharkhand | 17.8 | 22.6 |
| Odisha | 22.4 | 25.6 |
| West Bengal | 20.5 | 20.1 |
| Arunachal Pradesh | 24.9 | 33.1 |
| Assam | 19.1 | 20.3 |
| Manipur | 23.0 | 33.2 |
| Meghalaya | 18.7 | 21.4 |
| Mizoram | 17.7 | 25.2 |
| Nagaland | 22.3 | 28.7 |
| Sikkim | 34.5 | 41.6 |
| Tripura | 20.8 | 22.7 |
| Dadra & Nagar Haveli and Daman & Diu | 14.9 | 15.4 |
| Goa | 27.5 | 26.8 |
| Gujarat | 20.5 | 20.3 |
| Maharashtra | 23.1 | 24.4 |
| Andaman & Nicobar Islands | 25.3 | 30.2 |
| Andhra Pradesh | 25.3 | 29.0 |
| Karnataka | 25.0 | 26.9 |
| Kerala | 30.9 | 32.8 |
| Lakshadweep | 24.8 | 24.7 |
| Puducherry | 23.0 | 30.1 |
| Tamil Nadu | 24.8 | 30.2 |
| Telangana | 26.1 | 31.4 |
UTs: Union Territories; NFHS-5: National Family Health Survey-5.
Dyslipidemia in India
Dyslipidemia refers to either lipoprotein overproduction or deficiency, which is a consequence of abnormal lipoprotein metabolism. This leads to elevated total cholesterol, low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) concentrations, and a decrease in the high-density lipoprotein cholesterol (HDL-C) concentration in blood.24 Dyslipidemia could be primary (genetic defect in the lipid metabolism that causes abnormal lipid levels) and secondary (caused due to modifiable lifestyle and environmental factors, diseases, and medications).25
In the ICMR–INDIAB study conducted across four regions (TN, MH, JH, and Chandigarh), it was found that the prevalence of at least one lipid abnormality was 79% with highest rates found in Chandigarh (82.9%), followed by JH (80%), TN (76.9%), and MH (77%) with no urban–rural differences observed in any of the four regions. No lipid abnormality was found in 21.1% of the study population across four regions.26 In a study conducted among diabetic population to determine the prevalence of metabolic syndrome, dyslipidemia, and hypertension, it was found that the prevalence of metabolic syndrome was higher among females as compared to males (58% vs. 41%). Dyslipidemia was also reported to be present in more females as compared to males (72% vs. 56.3%).27 In a descriptive cross-sectional study conducted in urban and rural training center of Rajah Muthiah Medical College to find the effects of urbanization on dyslipidemia, it was reported that the prevalence of dyslipidemia was higher in urban areas (74.5%) than rural areas (68.8%), but this difference was not found to be statistically significant.28
Metabolic syndrome in India
NCDs, such as diabetes, hypertension, cardiovascular diseases (CVDs), cancer, and chronic respiratory diseases are the leading cause of death and are responsible for 74% of deaths worldwide. The epidemiological transition has documented an evident increasing trend of NCDs in developing countries. This is majorly attributed to demographic and socioeconomic advancement. The developing world is facing the double burden with infectious and non-infectious diseases in a poor environment with ill-health systems. In 2010, NCDs accounted for more disability-adjusted life years (DALYs) in India than communicable diseases, approximately 235 million vs. 222 million DALYs, respectively. As per WHO estimates, India has lost $237 billion between 2006 and 2015 because of premature deaths due to CVD, stroke, and diabetes.
Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and T2DM. In India, metabolic syndrome has been identified as a major public health problem with the prevalence ranging from 10% to 30%.29 Metabolic syndrome is constituted by AO, insulin resistance, hypertension, and dyslipidemia that directly increases the risk of CVDs, T2DM, and mortality. The patients with MS have an average 4-fold increased risk of developing stroke and myocardial infarction.
This recent upsurge might be directly linked with rapid economic development and urbanization, which brought drastic changes in lifestyle patterns and nutrition.30, The urban population, is the most vulnerable group for developing metabolic syndrome.31 Better socioeconomic status, decreased physical activity, stress, and unhealthy diet might be the contributory factors in urban areas. The state-wise data illustrated that the maximum prevalence of metabolic syndrome was reported in Madhya Pradesh (50%) followed by New Delhi (43%) and Odisha (43%). The least prevalence of metabolic syndrome is reported in Jammu & Kashmir (15%) followed by Haryana (18%) and Punjab (21%). Among the various geographical zones, people living in Northeast India have the highest prevalence of metabolic syndrome followed by Eastern India which highlights the need of understanding the influence of sociocultural and ethnogeographical factors in determining the risk of development of metabolic syndrome. The burden across the age groups varies considerably, and there is a steady increase from 18–29 years group (13%) to 50–59 years (50%). Regarding gender-related risk, females are having a higher prevalence of metabolic syndrome when compared to males. The reason can be attributed to the gender-specific risk factors such as menopause, polycystic ovarian syndrome, and the use of hormonal contraceptives.32 Elevated body weight, increased Waist Circumference (WC), and low High Density Lipoprotein (HDL) cholesterol when compared to men also adds on to these risks in women.
In 2020, a recent systematic review and meta-analysis have analyzed data from 111 studies with 133,926 participants. The prevalence of metabolic syndrome among the adult population in India was documented as 30% (95% CI: 28%–33%). There was a steady increase in the burden across the age groups from 13% (18–29 years group) to 50% (50–59 years). Study have also found that people living in urban areas (32%; 95% CI: 29%–36%) had higher prevalence when compared to tribal (28%; 95% CI: 21%–36%) or rural people (22%; 95% CI: 20%–25%). Gender distribution of metabolic syndrome showed that the females had a higher prevalence (35%; 95% CI: 31%–38%) when compared to males 26% (95% CI: 22%–29%).33
Non-alcoholic fatty liver disease (NAFLD) in India
Non-alcoholic fatty liver disease (NAFLD) refers to the presence of “fatty liver” in the absence of significant alcohol consumption or other alternative etiologies of hepatic steatosis.34 Histologically, NAFLD includes a spectrum that includes non-alcoholic fatty liver (NAFL), non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and hepatocellular carcinoma (HCC). NASH refers to the presence of lobular inflammation and hepatocyte ballooning in addition to hepatic steatosis and has been conventionally considered to be the severe form of NAFLD. The presence of underlying fibrosis is the main driver of clinical outcomes. NAFLD is a slowly progressive disease in the vast majority of patients, although there may be a rapid progression of fibrosis to cirrhosis in around 20%–30% patients.35
It has been estimated that almost one-quarter of the world’s adult population have underlying NAFLD.3 In India, the reported prevalence of NAFLD ranges from 9% to 53%, with a pooled prevalence of 38.6% among adults.36,37 One of the caveats in interpreting epidemiological data on NAFLD from India is that most of the studies have been conducted in the hospital setting and are therefore liable to referral bias, with the actual burden being lower in the community.37 The pooled prevalence of NAFLD in rural areas (29.2%) is substantially lower than that in urban areas (40.8%).38 Few studies have simultaneously looked at the prevalence of NAFLD in urban and rural communities and corroborate that the risk of NAFLD in urban-domiciled populations may indeed be higher compared to rural domicile.39,40 Studies also suggest that there may be a possible geographic variation in the burden of NAFLD in India, with the pooled prevalence being lower in the eastern states (14.5%) compared to those in the north (29.1%) and south (40.1%) India.38 This possible geographic variation may be partially attributable to differences in dietary practices, socioeconomic standards, and degree of urbanization. It should be acknowledged that various studies have used different definitions and diagnostic modalities for determining NAFLD, which may also account for the heterogeneity in their observations.
The prevalence of NAFLD has been reported to be even higher among high-risk patients like those with T2DM, pre-diabetes, obesity, metabolic syndrome, polycystic ovarian syndrome, or obstructive sleep apnoea.38 For instance, among patients with DM, the prevalence of NAFLD was estimated to be 56.5% in a multicentric study conducted in 189 centers in more than a hundred Indian cities.41 The pooled prevalence of NAFLD among those with one of the high-risk factors mentioned above has been estimated to be 52.8% (95% CI 46.5–59.1).38
There is increasing recognition of a high prevalence of NAFLD among Indian children, particularly in those who are obese.42 A meta-analysis incorporating eight studies and almost 2900 children reported a pooled NAFLD prevalence of 12.4% and 63.4% among non-obese and obese Indian children, respectively.38
RISK FACTORS OBESITY AND LIFESTYLE DISEASES IN INDIA
Diet and physical activity as risk factors for obesity in India
Recent studies have reported that globally, more than 1.9 billion adults are overweight, and 650 million are obese. Approximately 2.8 million deaths are reported as a result of being overweight or obese. Due to the consumption of energy-dense food (i.e., unhealthy food habits), sedentary lifestyle, lack of health-care services, and financial support, the developing countries are facing high risk of obesity and their adverse consequences (i.e., diabetes, ischemic heart disease, etc). In India, more than 135 million individuals are affected by obesity. The prevalence of obesity in India varies due to age, gender, geographical environment, socioeconomic status, etc. According to the ICMR-INDIAB study 2015, the prevalence rate of obesity and central obesity varies from 11.8% to 31.3% and 16.9% to 36.3%, respectively. In Indian population, AO is one of the major risk factors for CVD. Various studies have shown that the prevalence of obesity among women was significantly higher as compared to men. Obesity is one of the main medical and financial burdens for the government.43
Diet as a risk factor for obesity:
Childhood obesity is an important public health issue worldwide. Urbanization, sedentary lifestyle, and changes in food habits are the chief reasons behind this pandemic. In a small proportion of children, obesity is the result of endocrine, syndromic, or monogenic causes. Production of high-fat, sugar and/ or salt-containing foods, use of complex marketing and advertising practices, aggressive sales tactics, and confusing food labeling restrict the consumers’ ability to make rational and healthy choices.44
Satija et al conducted a cross-sectional study to identify dietary patterns in an Indian population and assess their relationship with anthropometric risk factors. The participants were rural-to-urban migrants and urban non-migrant factory workers, their rural and urban resident siblings, and their co-resident spouses. Three dietary patterns were identified: “cereals–savory foods” (cooked grains, rice/rice-based dishes, snacks, condiments, soups, nuts), “fruit–veg–sweets–snacks” (western cereals, vegetables, fruit, fruit juices, cooked milk products, snacks, sugars, sweets), and “animal-food” (red meat, poultry, fish/seafood, eggs). In adjusted analysis, positive-graded associations were found between the “animal-food” pattern and both anthropometric risk factors. Moderate intake of the “cereals–savory foods” pattern was associated with reduced odds of obesity and central obesity.45
Ganguly et al performed a cross-sectional study in 701 women (aged 35 years and above) selected by cluster sampling from 12 different wards of the Kolkata Municipal Corporation (Kolkata, India). The following three major dietary patterns were identified: the “vegetable, fruits, and pulses” pattern (characterized by higher intakes of dark-yellow and green leafy vegetables, sweets, fruits, pulses, nuts, poultry and eggs, and lower intake of mustard oil); the “hydrogenated and saturated fat and vegetable oil” pattern (characterized by higher intakes of butter, hydrogenated oil, ghee, vegetable oil, mustard oil, condiments, sweets, fish, high-fat dairy, and refined grain); the “red meat and high-fat dairy” pattern (characterized by higher intakes of red meat, high-fat dairy products, whole grain, high-energy drinks and condiments, and lower intakes of fish, refined grain, and low-fat dairy products). The hydrogenated and saturated fat and vegetable oil pattern was positively associated with BMI, WC. In this Bengali population, these three major dietary patterns were observed, and the dietary patterns were independently associated with BMI, WC, and serum TC concentrations in women.46
Gulati et al performed a randomized controlled trial on 122 overweight/obese men and women administered either a high protein meal replacement (HPMR) or a control diet after two weeks of diet and exercise run-in. Body weight, WC, percentage body fat, fasting blood glucose, post-oral glucose tolerance test (post-OGTT) blood glucose, fasting and post-OGTT serum insulin, lipid profile, high-sensitivity C-reactive protein, kidney function, and hepatic aminotransferases were assessed before and after the intervention. The findings show that intervention with HPMR may lead to significant weight loss and improvement in obesity measures, metabolic, lipid, and inflammatory parameters, and hepatic transaminases in overweight/obese Asian Indians.47
Agarwal et al investigated the prevalence of obesity and diabetes among adult men and women in India consuming different types of vegetarian diets compared with those consuming non-vegetarian diets. Mean BMI was lowest in pesco-vegetarians (20.3 kg/m2) and vegans (20.5 kg/m2) and highest in lacto-ovo vegetarian (21.0 kg/m2) and lacto-vegetarian (21.2 kg/m2) diets. In this large, nationally representative sample of Indian adults, lacto-, lacto-ovo, and semi-vegetarian diets were associated with a lower likelihood of diabetes. These findings may assist in the development of interventions to address the growing burden of overweight/obesity and diabetes in Indian population.48
Physical inactivity as a risk factor for obesity:
Patil et al conducted a cross-sectional study among adult patients attending the health centers of Indira Gandhi Government Medical College. Out of 200 study subjects, 59% were having a sedentary lifestyle, 27% were having a moderately active lifestyle, and 14% were having a vigorously active lifestyle. A statistically significant increasing trend for sedentary study subjects (P = 0.002) with age was found. Those who reported sedentary physical activity levels (PALs) had 3.42 odds of being hypertensive, 7.44 times odds of being diabetic, three times odds of being overweight, and 2.41 odds of being obese. The adults in urban areas had significantly less PALs when compared to rural areas. Higher levels of sedentary lifestyle were found in urban areas compared to rural areas. As the age increased, the sedentary lifestyle was having a significantly increasing trend. Physical activity was associated with the diabetic status, hypertensive status, and obesity status.49
Singh et al conducted a cross-sectional study to find out the prevalence of overweight, obesity, undernutrition, and physical activity status in the urban populations of India. Cross-sectional surveys were conducted in 6–12 urban streets in each of the five cities across five different regions of India using a common study protocol and criteria of diagnosis. Obesity, overweight, central obesity, and sedentary behavior coexist with undernutrition and have become a public health problem in all the five cities of India. The prevalence of obesity and sedentary behavior was significantly greater in Trivandrum, Calcutta, and Bombay compared to Moradabad and Nagpur. Sedentary behavior was significantly associated with obesity compared to non-obese subjects in both sexes, which may be due to greater economic development in metro cities.50
Arora et al conducted a cross-sectional study in eight schools (Private and Government) of Delhi in the year 2006. Participants: 1814 students from 8th and 10th grades. A total of 944 (52.0) private schools defined as belonging to the middle-to-upper income stata and 870 (48.0) government schools defined as belonging to the low-to-middle income group were taken in the study by MYTRI end-line survey in 2006 (Project MYTRI -Mobilizing Youth for Tobacco-Related Initiatives in India). Daily breakfast consumption is associated with less overweight and obesity and with healthier dietary and physical activity-related behaviors among urban Indian students.51
Diabetes mellitus:
India has the second largest number of people with diabetes in the world. Its increased incidence is driven by a combination of factors – rapid urbanization, sedentary lifestyles, unhealthy diets, tobacco use, and increasing life expectancy. According to WHO, India had 69.2 million people living with diabetes in 2015, and nearly 98 million may have T2DM by 2030. In 2019, diabetes was the ninth leading cause of death, with an estimated 1.5 million deaths directly caused by diabetes. NFHS-5 data revealed that the prevalence of diabetes in men is 15.6 % and in women it is 13.5 %.12,52
Diet as a risk factor for DM in India:
The etiology of diabetes is believed to be multifactorial, nevertheless increase in the prevalence of T2DM in most populations has probably been driven by modifiable risk factors, including a sedentary lifestyle and/or lack of exercise and unhealthy diets like increased intake of refined grains, fat, sugar, and sweetened beverages and decreased intake of fruits and vegetables.53
Nagarathna et al. conducted across seven zones of India, studying the association of dietary factors such as milk products, meat, and junk foods with fasting blood glucose and postprandial blood glucose in 12,500 individuals. In this multicentre cluster randomized controlled study covering 60 states and four union territories; 17,285 individuals were surveyed for dietary factors. The findings of the present study revealed that regular ingestion of excessive milk, meat, and junk foods has a substantiated effect on the blood glucose levels of individuals, particularly in the case of DM. The analysis of the results showed that consumption (usual/often) of milk (OR = 7.180), meat (OR = 6.81), less fibers (OR = 17.77), and less fruits (OR = 14.71) was strongly and positively associated with fasting blood glucose (P < 0.001). The post-prandial blood glucose (PPBG) in diabetes individuals also had a strong positive association (P < 0.001) with consumption (usual/often) of meat (OR = 22.82) and milk (OR = 17.19). In pre-diabetes individuals, milk was significantly (P < 0.001) associated with fasting blood glucose (OR = 2.74). In non-diabetes individuals also, milk was significantly associated with PPBG (OR = 2.56). Consumption of junk food was associated significantly (P < 0.001) with the status of known diabetes (OR = 1.345) and known hypertension (OR = 1.247). In all, the consumption of milk, meat, less vegetables, less fruits, and junk food has a significant effect on the glycemic status and cholesterol levels, and also on the status of known diabetes and hypertension.54
Dietary carbohydrates (quantity and quality) and diabetes risk:
Increased consumption of refined cereals and white rice accounting for 73% of daily calorie intake from white rice. Due to rapid industrialization and green revolution, there has been a large increase in the consumption of refined grains (polished rice, white flour, semolina) in the last few decades. White rice, in particular, has a high glycemic index (GI) and accounts for almost 50% of the total calories in the diet of the South Indian urban population and 73% of the daily calorie intake of the rural Indian population. Data from Sri Lanka showed that white rice accounted for about 73% of caloric intake, while in Bangladesh, rice and other cereals contributed to 80% of the total calories. Thus, it is important to encourage the consumption of low-GI and high-fiber foods in this population in order to reduce the dietary glycemic load. Making a simple change in diet, such as substituting brown rice as an alternative to polished white rice, may help to reduce the burden of T2DM in India and South Asia.55
The quality of the carbohydrates is very important such that whole grains and fiber are better choices than refined grains, and that fiber intake should be at least as high in people with T2DM as recommended for the general population, that diets that have a higher glycemic index and load are associated with an increased risk of T2DM, and that there is a modest glycemic benefit in replacing foods with higher glycemic load with foods with a low glycemic load. However, debate continues about the independence of these effects from the intake of dietary fiber. Some evidence exists that consumption of potato and white rice may increase the risk of T2DM, but this is limited and further research is needed.56
Sugar and sugar-sweetened beverages:
In South Asia, the energy obtained from sugar and sweeteners has considerably increased in recent times. In Nepal, it has increased from 4 g/capita/day in 1970 to 57 g/capita/day in 2010. A report in 2009 found that sugar intake among urban South Indians was mainly in the form of added sugar in hot beverages (tea and coffee), and contributed about 3.6% of the total glycemic load compared to refined cereal (white rice), which provided 66% of the glycemic load. However, recent data suggest an increase in the intake of sugar from sugar-sweetened beverages among Indians. Further, the intake of “total” sugar (traditional sugar + sugars from sugar-sweetened beverages) among Indians (25.0 kg/capita in 2011) exceeds the average global annual per capita consumption of 23.7 kg. Diet lower in sugar-sweetened beverages has been shown to reduce the risk of diabetes in India.54
Dietary fats (quantity and quality) and diabetes risk: Evidence:
Visible fats and oils are the main contributors to daily calorie intake in Indians. However, the total intake of dietary fat among Indian urban adults (24% total calories) and rural Indians (13% total calories) appears to be within the recommended intake of 30% of total calories. Visible fats and oils contribute almost half of the total calories derived from fat in Indian diets. There has been a sharp increase in the intake of dietary fat in the last three decades, from 29 g/capita/day in 1970 to 45 g/capita/day in 1999 in the South Asian population. More worrying is the fact that the quality of dietary fat in the South Asian population comprises a low intake of monounsaturated fatty acid (MUFA) and n-3 polyunsaturated fatty acid (PUFA) and a high intake of fats such as saturated fatty acid (SFA), and trans-fatty acid (Trans-Fatty Acid (TFA); mostly related to the widespread use of vanaspati, a hydrogenated vegetable oil) showing an imbalance and association with increased risk for NCDs especially T2DM. Several studies have reported that consumption of SFA or TFA contributes to an increased risk of NCDs like T2DM. Fat-rich animal foods are the primary source of SFA in diets. The total meat consumption has increased significantly in all South Asian countries in the past two decades. Countries like India have doubled their intake of meat and poultry since 2000, but the actual quantity is still low (50 g/capita/day), compared with diets in, for example, the United States Average Intake (USAI) (128 g/capita/day).
Meat consumption in Pakistan has increased by 130%. Sri Lanka has also gradually increased the trend in meat consumption from 1992 to 2007. Studies have shown that South Asians consume an excess of n-6 PUFA. This has primarily occurred because traditional oils such as groundnut (a good source of MUFA) and sesame were replaced with oils that are high in n-6 PUFA, like sunflower and safflower oils, leading to an imbalance in the n-6/n-3 ratio. Studies have shown that this imbalance in n-6/n-3 ratio, owing to the consumption of these high-n-6 PUFA oils, is associated with an increased risk for metabolic syndrome.
Similar findings were reported by Misra et al. in 2009. TFAs are even more deleterious to health than SFAs, owing to the hydrogenation process, which converts liquid oils to solid fats like vanaspati and margarine. The consumption of vanaspati accounts for 50% of TFA use and it is predominantly consumed in South Asian countries like India and Pakistan.57 For unprocessed red meat, the evidence of possible harm because of the development of T2DM is less consistent and of a smaller magnitude.56,58
Low consumption of fruits and vegetables:
There is evidence to suggest that consumption of fruits and vegetables (≥5 servings or 400 g/day) is associated with a reduction in the risk of chronic diseases like T2DM and coronary heart disease. However, the intake of fruits and vegetables is far below the recommended levels in almost all South Asian countries.
The average per capita consumption of fruits and vegetables in India is around three servings/day, while it is 2.2 servings/day in Sri Lanka, 1.8 servings/day in Nepal, and one serving/day in Maldives. A study in South Indians showed an inverse association between intake of fruits and vegetables and blood pressure, WC, total cholesterol, and LDL-C concentrations. Another study showed that total dietary fiber intake was inversely associated with total cholesterol and LDL cholesterol levels in people with diabetes.55
South Asian diets are high in carbohydrates derived from refined cereals like white rice and refined flour. There is also a high intake of fat, especially SFA and PUFA, mainly in the forms of n-6 (omega-6) PUFA and TFA, and a low intake of MUFA and n-3 PUFA (resulting in a higher ratio of n-6/n-3). The diet is also low in dietary fiber and several micronutrients (e.g., magnesium, calcium, and vitamin D), all of which may contribute to the increased risk for NCDs like T2DM. This shift from ancestors’ diets (high in animal protein, adequate in fiber, relatively low in carbohydrates, and limited animal fat) has resulted primarily from the changes in demography and socioeconomic status and “modernization.” Urbanization and rising income levels have also led to an increase in the consumption of milled and polished grains like rice and wheat rather than unpolished brown rice, corn, and millet. Further, urbanization has led to increased employment for women. This has promoted a shift from home-cooked traditional foods to pre-cooked convenience foods, as the mother has less time to cook.53
Physical activity as a risk factor for diabetes mellitus:
Physical inactivity is an independent risk factor for T2DM, and current evidence suggests that adequate levels of physical activity may reduce the risk of T2DM by 27%. Modern technical gadgets and the use of motorized transport have reduced physical activity among children and young adults. In 2013, Ranasinghe et al.59 reported that the overall prevalence of physical inactivity among the population of India was 19%–88%, followed by Pakistan (60%) and Sri Lanka (11%–32%). The recent Indian Council of Medical Research–India Diabetes (ICMR–INDIAB) study also reported that levels of physical inactivity were high (≈55%) among Asian-Indians. According to the American Diabetes Association (ADA), “physical activity” is defined as bodily movement produced by the contraction of skeletal muscle that requires energy expenditure in excess of resting energy expenditure, while “exercise” is defined as a subset of physical activity that is planned and structured and consists of repetitive bodily movement performed to improve or maintain one or more components of physical fitness.55 Physical activity was assessed using the Global Physical Activity Questionnaire (GPAQ), which was developed by the WHO—in ICMR-(Indian Council of Medical Research–India Diabetes) study for both the rural and the urban population in India. However, in the Ranasinghe study (a review), a number of methods were used for defining physical activity [Table 2], the most common ones were the interviewer-administered questionnaire and PAL, or the interviewer-administered questionnaire or the GPAQ by WHO.55
| Organization | Type of physical activity | Frequency |
|---|---|---|
| American College of Sports Medicine (ACSM), 200060 | Moderate to vigorous aerobic training | At least 3 nonconsecutive days/week |
| Moderate to vigorous resistance training | At least 2 days/week | |
| Canadian Diabetes Association (CDA), 200361 | Moderate to vigorous aerobic training | At least 3 nonconsecutive days/week |
| Moderate to vigorous resistance training | 3 days/week | |
| American Diabetes Association (ADA), 200462 | Moderate to vigorous aerobic training | 150 min/week spread out over at least 3 days/week |
| Moderate to vigorous resistance training | 2-3 days/week | |
| ADA and ACSM, 201063 | Moderate to vigorous aerobic training | 150 min/week spread out over at least 3 days/week with no more than 2 consecutive days between bouts of aerobic activity |
| Moderate to vigorous resistance training | 2-3 days/week | |
|
For additional health benefits:
|
||
The role of physical inactivity in the diabetes epidemic:
Physical inactivity has been shown to be an important risk factor for most chronic diseases, including T2DM, and seems to increase the risk of T2DM independently of diet. A sedentary lifestyle over several years has been shown to be associated with increased risk for T2DM, CVD, and premature mortality. There is mounting epidemiological evidence that, in addition to reduced physical activity, “sedentary behavior”, defined as engaging in activities at the resting level of energy expenditure, which includes sleeping, sitting, lying down, computer time, and viewing television, also plays an important role in the etiology of T2DM.
European data suggests that even resistance training has the potential to improve muscle strength and endurance, enhance flexibility and body composition, decrease risk factors for CVD, and result in improved glucose tolerance and insulin sensitivity. In order to prevent T2DM in high-risk individuals (e.g., those with impaired glucose tolerance), the ADA and American College of Sports Medicine (ACSM) recommend at least 150 min/week (2.5 h/week) of moderate to vigorous physical activity [Table 2].53
Patterns of physical activity in South Asians:
Wide variations in the prevalence of physical activity have been reported in countries of South Asia, namely Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. In 2004, it was reported that the rates of physical activity were 50%–75% less among South Asians compared to the general population living in the United Kingdom of Great Britain and Northern Ireland. The World Health Survey, a large cross-sectional study, was conducted by WHO in 51 countries in 2002 and 2003. This included countries that had a large proportion of the world’s population, with a wide geographical distribution across WHO regions, including several countries in the Southeast Asia Region. Physical activity was assessed using the International Physical Activity Questionnaire. The prevalence of physical inactivity for men in South Asian countries, including Bangladesh, India, Nepal, Pakistan, and Sri Lanka, ranged from 6.5% to 12.8%, while for women, it ranged from 9.7% to 27.3%.
Three studies on physical activity have been reported from Sri Lanka: the WHO STEPS (STEP wise approach to Surveillance) survey, one in the western province of Sri Lanka, and finally, a nationally representative study. The prevalence of inactivity was reported to be 25% in the WHO STEPS survey, 31.8% in the western province, and 11% in the national sample. Men were more inactive than women, and inactivity was reported to be 35.2% in urban adults and 27.6% in rural adults in the study from the western province of Sri Lanka. A study on physical activity conducted in Pakistan in 2010 reported a high prevalence of inactivity (60.1%). The WHO STEPS survey conducted in Bhutan in 2007, Maldives in 2011, and Nepal in 2013 reported inactivity levels of 58.6%, 45.9%, and 3.5% in these populations, respectively.
Several studies have been done in India, and the prevalence of inactivity ranged widely from 9.7% to 54.4%, probably reflecting the methodology used or the sample surveyed. The WHO STEPS survey done on 1359 males and 1469 females in a rural area in the Faridabad district of Haryana reported a very high rate of physical inactivity. Another study conducted by Sullivan et al.60 in 2011 which assessed the PALs in migrant groups in India (n = 6447) showed that physical activity was highest in rural men, followed by migrants, and then urban men. Levels of sedentary behavior and television viewing were lower in rural residents, whereas these were similar among migrant and urban residents. In 2014, Anjana et al.61 assessed the pattern of physical activity in a community-based national survey, the ICMR–INDIAB study, in four areas of India (TN, MH, JH, and Chandigarh, representing the south, west, east, and north of India, respectively), using the GPAQ. Of the 14,227 individuals studied, 54.4% were inactive. Subjects were more inactive in urban areas compared to rural areas (65.0% vs. 50.0%). Thus, epidemiological studies from South Asian countries show that a large percentage of people in this region are inactive, with very few engaging in recreational physical activity; the explosive increase in the prevalence of T2DM in these countries may be attributed to this high percentage of inactivity.
A systematic review done by Horne and Tierney in 2012, on barriers to exercise and physical activity among older adults in South Asia, concluded that a lack of understanding about benefits, a communication gap with healthcare professionals, cultural beliefs, and a lack of culturally sensitive facilities are some of the barriers for physical activity. In a recent study conducted by Anjana and colleagues in 2015 for the Diabetes Community Lifestyle Improvement Program, the most frequent barriers to exercise perceived by men were “few places to exercise” and “tires me,” followed by “takes too much of my time” and “places to exercise are far away.” The reasons most frequently cited by women were “takes too much of my time,” followed by “few places to exercise,” and “takes time away from my family.” Thus, it is clear that these barriers to physical activity must be overcome if levels of physical activity in society are to be improved.55
Diet and physical inactivity as risk factors for metabolic syndrome in India:
Metabolic syndrome is a constellation of interrelated risk factors characterized by the co-occurrence of hyperglycemia, hypertension, high triglyceride levels, and low HDL-C levels. Metabolic syndrome also increases the risk of type 2 DM, CVD by 2-fold and a 5-fold increase in mortality over a 5–10 years period. It is estimated that 20%–25% of the world’s adult population suffer from metabolic syndrome disorders. In India, the prevalence of metabolic syndrome is increasing exponentially, as determined by 33.5% overall, 24.9% in males and 42.3% in females. It is a mixed outcome of genetic, metabolic, dietary, physical activity-related, and some environmental factors. A dietary habit seems to play a prime importance in the treatment and prevention of metabolic syndrome.
Metabolic syndrome: Dietary risk factors:
In general, the probable dietary risk factors include a shift occurring toward increasing consumption of calorie-dense foods containing refined carbohydrates, fats with high intakes of saturated fatty acids, and low intakes of omega-3 fatty acids, red meats, and low fiber increases the risk of metabolic syndrome. Although people consume a diet which includes many types of nutrients, in a cross-sectional study performed on Indian participants by Verma et al at the Institute of Medical Sciences, Banaras Hindu University (BHU), found an association between important nutrients risk factors and the number of metabolic syndrome components. Unhealthy eating practices with intake of less than three servings of fruits and vegetables were seen more among the participants who had more than three risk factors than in the participants who had three risk factors. The odds of taking more than times junk foods/week were three times higher, and sweet dishes were 2.3 times higher among the participants who had four to five risk factors when compared to the participants who had three risk factors. Significantly higher proportion of participants (33.7%) were in the habit of taking flesh foods and eggs>four times/week among the participants who had four to five risk factors in comparison to 9.3% among participants who had three risk factors. High intake of sodium is a major risk factor for CVDs for participants who had four to five risk factors. Also potassium, vitamin A, and phosphorus intake were lower among participants who had four to five risk factors.62 In another study by Misra et al. assimilating from several nutritional surveys in various developing countries, it concluded that low intake of n-3 PUFAs (obtained from flaxseed, mustard, and canola oils) and long-chain (LC) n-3 PUFAs (obtained from fish and fish oils), and increased intake of SFAs (obtained from coconut oil, palm oil, and ghee [clarified butter]) increases the risk of metabolic syndrome. Data also showed that intake of MUFAs ranged from 4.7% to 16.4% in developing countries, and supplementing it from olive, canola, mustard, groundnut, and rice bran oils may reduce metabolic risk.57 Radhika et al, in a cross-sectional study, evaluated the association of refined grains consumption with insulin resistance and metabolic syndrome in an urban South Indian population and found that the mean refined grain intake was 333 g/d (46.9% of total calories). Compared with participants in the bottom quartile, participants who were in the highest quartile of refined grain intake were significantly more likely to have metabolic syndrome (OR, 7.83; 95% CI, 4.72–12.99). Higher intake of refined grains was associated with insulin resistance and metabolic syndrome in this population of Asian Indians who habitually consume high-carbohydrate diets.63
Metabolic syndrome: Physical activity risk factors:
WHO predicts that by 2030, India, with over 79 million diabetic subjects, will contribute to more than 20% of the world’s diabetic population, and MS is probably due to the rapid demographic transition experienced in India, coupled to a more sedentary lifestyle. In data drawn in Chennai Urban Population by Mohan et al, it predicted a significantly increased prevalence of most of the components of metabolic syndrome (diabetes P < 0.001, obesity P = 0.003, AO P < 0.001, and hypertension P < 0.001) with a decrease in physical activity. Subjects in the light-grade activity group also had 2.4 higher odds of coronary heart disease (P = 0.011), compared with the heavy-grade activity group. They concluded that less physical inactivity is associated with the components of metabolic syndrome.64 In another multisite study in the urban Indian setup, the prevalence of metabolic syndrome was significantly greater in subjects with the highest vs. lowest categories of sedentary lifestyle (47 vs. 38%) (P < 0.05), where any active physical activity was considered with >30 min of work and leisure, or commute-related physical activity was classified as moderately active. Physical inactivity was associated with higher triglyceride levels in males and with higher hip circumference, diastolic blood pressure, triglycerides, and fasting plasma glucose in females.65
Non-alcoholic fatty liver disease: Diet as a risk factor:
The prevalence of NAFLD among the general population in India ranges from 9% to 53%. NAFLD is a global problem growing in parallel to the epidemics of obesity and diabetes, with South Asians being particularly susceptible. Nutrition and behavior are important modifiers of the disease. In an Indian cross-sectional case–control study held by Vijay et al, it was found that NAFLD patients had significantly higher consumption of refined rice, animal fat, red meat, refined sugar, and fried foods, and had lower consumption of vegetables, pulses, nuts, seeds, and milk compared to controls.66 The consumption of red meat, animal fat, nuts, and refined rice was positively associated with NAFLD diagnosis and the presence of fibrosis, whereas the consumption of leafy vegetables, fruits, and dried pulses was negatively associated. Fried food consumption was positively associated with NAFLD, on the other hand, boiled food consumption had a negative association. Increased consumption of animal fats was associated with diabetes, hypertension, and cardiovascular outcomes among those with NAFLD, whereas consumption of wholegrain rice was negatively associated with these clinical-related outcomes.
In other case–control study by Singh et al, it was found that dietary risk factors associated with NAFLD were non-vegetarian diet (meat/fish), fried food, spicy foods, and tea.67 This study also revealed that urban middle-class men with a sedentary lifestyle had a greater risk of NAFLD, which may be due to high fat intake in them. In a North Indian case–control study held on obese children, daily consumption of soft drinks (60.4%) and fried chips (58.5%) was more in NAFLD group than without NAFLD group. Also, calorie intake was more in obese children but excess in NAFLD group.68
In an Indian case–control study held by Bhatt et al., the mean dietary intakes of total energy, carbohydrate, protein, total fat, saturated fat, and total cholesterol were significantly higher, while intake of MUFAs and PUFAs was significantly lower in cases as compared to controls.69 In another case–control study by Sathiaraj et al., the total calorie intake, percent of carbohydrate, and fat intake of NAFLD cases were significantly higher than controls. Decreased nutritional intake with restricted fat may constitute an important therapy in subjects with NAFLD.70
Non-alcoholic fatty liver disease: Physical inactivity as a risk factor:
NAFLD has today emerged as the leading cause of liver disorder, and physical inactivity is one of the major causative factors. In an Indian case–control study held by Singh et al, a majority (90.2%) of NAFLD patients were found to be sedentary with more than four times of any kind of physical activity/week, and only 32.8% NAFLD patients undertook regular exercise (>4 times/week).67 In other North Indian case–control study by Singh et al., the mean physical activity in a day (expressed as MET. Minutes) and total energy expenditure were significantly lower in cases than in controls (33.3 ± 3.6 vs. 36.2 ± 0.5, P ¼ 0.001 and 2707.6 ± 505.6 vs. 2904.3 ± 690.3, P = 0.02, respectively) signifying lower physical activity as a risk factor for NAFLD.67 Also, in another study by Nath et al., NAFLD police trainees in a moderate-intensity exercise group and in a low-intensity exercise group were recruited for a 6-month physical training course. Subjects in the low-intensity exercise had higher triglycerides and lower HDLs than moderate-intensity exercise subjects. Also, hepatic steatosis regressed in 66.7% of the NAFLD subjects in the moderate-intensity exercise group but in only 26.3% of the low-intensity exercise NAFLD subjects (P = 0.030).71
Genetic factors in lifestyle diseases
Traditionally considered an undernourished country, the prevalence of overweight and obesity is fast increasing in India. Between 2005 and 2019, India has witnessed an increasing prevalence of overweight and obesity (BMI ≥ 25 kg/m2): from 12% to 23% in men and from 15% to 24% in women.72 Obesity is one of the strongest risk factors for other chronic diseases, including but not limited to T2DM, CVD, and NAFLD.73 Central to these is the development of overweight and the accretion of total and ectopic body fat. While discussing the genetics of NAFLD primarily, work on the genetics of selected lifestyle-associated disorders, including overweight/obesity, is also discussed below. This review focuses on Indian studies.
Genetic factors of overweight and obesity in India:
Two recent reviews shed light on the genetic variants of obesity reported in Indians.74,75 The reported variants are: FTO, MC4R, TNF-α, PPAR-γ, UCP1, UCP2, LPL, LEPR, AMD1, IL6, IL6R, APOE, ADIPOQ, DOK5, INSIG2, PBEF1, Myostatin, CXCR4, HHEX, IRX3, POMC, NGN3, FOXA2, FLJ3970, MTR, TCN, CHDH, CETP, LMNA, APOB, AGRP, TCF7L2, and THADA. None of these variants are India-specific or novel, as these studies were variant-specific validation studies for variants that had been identified through Genome-wide association studies (GWAS) or sequencing-based-genome-wide approaches in other ethnicities. A single GWAS study on 5973 Indian adults, with a replication of the findings on 1286 Indian adolescents, was reported by Giri et al. in 2020.76 This study reported the identification of novel variants in SLC22A11 and ZNF45 associated with BMI in Indians. Identification of further novel, India-specific variants, which may provide further insights into Indian aspects of obesity, will be dependent on studies done on large sample sizes with genome-wide approaches.
Genetic factors of diabetes in India:
Similar to investigations into the genetics of obesity and of NAFLD in India, attempts have been made to evaluate associations of genetic variants previously identified through genome-wide discovery approaches in other ethnicities with T2DM in Indians through variant-specific validation studies. Through such studies, associations of variants in TCF7L2, SLC30A8, STRA6, KCNQ1, INS, INSR, and PP1G.G have been confirmed in the Indian population.77–80 Tabassum et al. reported TMEM163 (coding for transmembrane protein 163) as a novel T2DM-associated gene from their GWAS study in select Indian populations in North (Delhi) and South (Chennai) India.81 Interestingly, a replication study conducted in a separate group of subjects from Northwest India belonging to the Indo-European linguistic group was unable to find this similar association of TMEM163 with T2DM indicating large within-country genetic disparity, even in geographically close population groups.82
Genetic factors of hypertension in India:
The ACE insertion/deletion polymorphism has been reported to be associated with hypertension in Indians from various parts of the country in multiple studies.83–85 Apart from ACE, variants in CYP11B2,86 NOS3,87 AGT,88 FABP2, and GST89 have also been reported to be associated with higher risk of hypertension in Indians.
Genetic factors of dyslipidemia and metabolic syndrome in India:
Since dyslipidemia is one of the conditions included within the metabolic syndrome, genetic variants associated with dyslipidemia and with metabolic syndrome usually overlap with each other and also with those associated with obesity and T2DM. Variants in FABP2 and APOC3,90 TCF7L2,91 CETP,92 RETN,93 TNF-α,94 and ADIPOQ95,96 have been reported to be associated with dyslipidemia and metabolic syndrome.
Genetic factors of NAFLD in India:
NAFLD involves progressively increasing deposition of fat in the liver, resulting in fatty liver, hepatic fibrosis, cirrhosis, and either liver failure or HCC, all without addiction to alcohol.97 The prevalence estimate of NAFLD in 2022 is 32.4% worldwide and 38.6% in India.98,99 NAFLD heritability is estimated to range between 20% and 70%6 and ∼25 genetic variants have been reported to be associated with NAFLD.100
The identification of the genes associated with NAFLD is important, as it allows for the prevention and identification of drug pathways. The first genetic variant identified in the Dallas Heart Study participants, not associated with NAFLD directly but with heightened hepatic fat content and hepatic inflammation, was the non-synonymous rs738409 C/G variant in PNPLA3 (patatin-like phospholipase domain containing 3/ adiponutrin/calcium-independent phospholipase A2-epsilon) leading to I148M amino acid substitution.101 A gene coding for a protein of unknown function at that time, this report fuelled intense work towards elucidation of the coded protein’s function. PNPLA3 turned out to be a triglyceride hydrolase with predominant expression in the liver, with the I148M variant promoting hepatic triglyceride accumulation by inhibiting triglyceride hydrolysis.102,103 Kozlitina et al. conducted an exome-wide association study and identified the rs58542926 variant (Glu167Lys) in TM6SF2 associated with liver fat content.104 Similar to PNPLA3, TM6SF2 was a gene of unknown function at that time, but this report led to extensive investigations on the function of the transmembrane protein coded by it. Utilizing Tm6sf2 knockout mice that exhibited hepatic steatosis and hypocholesterolemia, even without any dietary interventions, Smagris et al. reported that TM6SF2 is required for mobilization of neutral lipids for very low-density lipoprotein assembly.105 These examples provide justification for conducting future studies to identify novel genetic variants associated with NAFLD to understand the pathophysiology of NAFLD at a cellular and molecular level.
A further reason for studying the genetics of NAFLD is to develop ethnicity-appropriate risk-stratification. Large ethnicity-based disparities in heritability of NAFLD have been noted, with heritability of NAFLD more than double in Hispanics (33%) than in African Americans (14%).106 The MBOAT7 rs641738 variant has been reported to be associated with the development and severity of NAFLD in individuals of European descent but not in Hispanic or African-Americans.107 Clearly, ethnicity-appropriate appropriate risk-stratification seems to be the next logical step. However, comparable data for South Asian Indians are sparse and inadequate. Going beyond genetics, epigenetics of NAFLD is now increasingly coming under focus, especially in terms of changes in levels of microRNAs in plasma or DNA methylation in cell-free DNA in plasma that can act as markers of NAFLD progression or as early markers of development of Hepatocellular Carcinoma (HCC) in NAFLD patients who have progressed to steatohepatitis.108 Similar work is lacking in India.
The few GWAS or locus-specific validation studies conducted in India point to associations of NAFLD with known variants [PPARγ, SREBP-2 1784 G/C, AGTR1, SAMM50 (rs3761472), and PNPLA3 (rs738409)] and a few novel variants [FAM161A (rs17513722), and promoter of IL27 (rs4788084)].109–112 Of these studies, two studies used abdominal ultrasound-based diagnosis of NAFLD (162 NAFLD subjects) and genotyped by polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) to assess the association of the PPARγ and SREBP-2 variants with NAFLD.109,110 Zain et al. included biopsy-proven 144 NAFLD patients based on increased echogenicity (compared to renal cortex) on ultrasound with or without abnormal alanine transferase (ALT) and did genotyping with pre-designed TaqMan SNP genotyping assays to test association of AGTR1 variants with susceptibility to NAFLD111 and Chatterjee et al used exome-wide sequencing to identify SNPs associated with hepatic fat content measured by Proton magnetic resonance spectroscopy (H1-MRS) in 244 subjects with abdominal ultrasound based diagnosis of NAFLD.112 Some data suggest that there may be a variation in the genetic predisposition of NAFLD among Indians based on ancestry, with TM6SF2 being significantly associated in South Indian ancestry and PNPLA3 in Northeast Indian ancestry. Nonetheless, it should be emphasized that no single genetic polymorphism is sufficiently strong to account for NAFLD, and other additional risk factors are practically always present.
Genetics of obesity and lifestyle diseases in India:
Considering the large existing diversity amongst Indians, in terms of multiple ancestral populations and admixed groups113 as well as diversity of environmental factors such as dietary habits,114 future region-specific genetic and epigenetic studies with large sample sizes that incorporate simultaneous deep phenotyping of the subjects are the need of the hour, to improve our understanding of the modifiable factors affecting the onset and progression of obesity and associated lifestyle diseases, including T2DM, hypertension, metabolic syndrome, and NAFLD in India. Further, the exploration of biological function and associated consequences of the identified variants in a country-specific context will lead to the translation of this knowledge into improving prevention, diagnosis, and development of focused therapeutic approaches.
Other common risk factors for lifestyle diseases
India, in recent decades, has been experiencing a rapid epidemiological and economic transition, which has created several implications for the health status of the people. Lifestyle diseases or NCDs have emerged as the leading cause of morbidity and mortality for adults throughout the world, including developing countries like India. India’s burden of NCDs is escalating and contributes to around 65% of all deaths.115 NCDs are typically present in individuals aged 55 years or older in many developed countries, but their onset occurs in India a decade earlier (≥45 years of age).116
Magnifying this problem are the issues of multiple chronic conditions and the fact many remain undiagnosed due to a lack of awareness and insufficient healthcare access. Rapid urbanization and industrialization drive the rising burden of NCDs that are characterized by the uptake of unhealthy lifestyles such as tobacco and alcohol use, physical inactivity, and unhealthy diet. The Global Burden of Disease Study (Indian estimates) reports blood pressure as one of the three leading risk factors for national disease burden. In India, the prevalence of various NCDs and its risk factors shows wide variations across geographic regions. Although the NCD burden has grown, India still does not have sufficiently detailed data on NCDs for research and policy purposes.
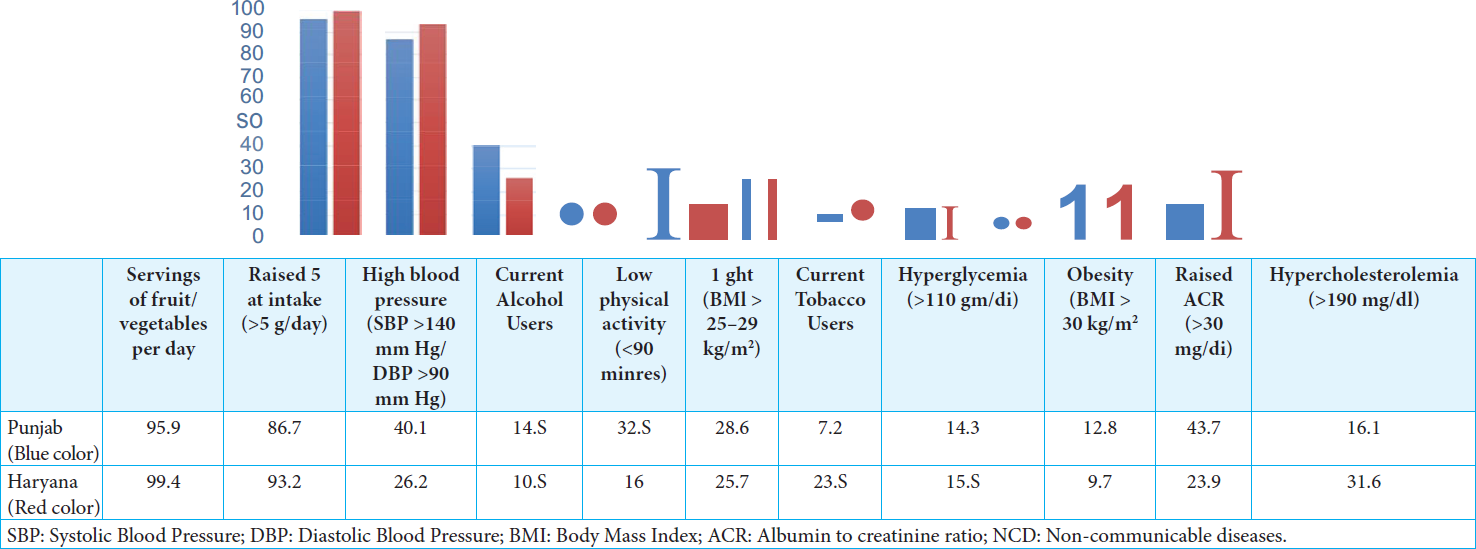
The overall prevalence of hypertension and diabetes in India is 28.5% and 9.3%, respectively. The prevalence of tobacco and alcohol use is 32.8% and 15.9%, respectively. More than one-third adults are physically inactive (41.3%). The prevalence of overweight and obesity among adults is 26.1% and 6.2%. Two-fifths, i.e., 40.2% of the adults, had a clustering of more than three risk factors. 12.8% of adults (40–69 years) have a 10-year CVD risk of ≥30% or with existing CVD.117 The regional estimates of the risk factors and disease burden varies. As per the National Non-communicable Disease Monitoring Survey regional estimates, Southern India showed significantly highest prevalence of overweight and obesity (41.1% and 12.5%), respectively, central obesity (49.5%), raised blood pressure (35.6%), and raised fasting blood glucose (21.2%), while Northeast India showed the lowest prevalence of overweight (22.4%), obesity (3.7%), and central obesity (29.0%), while raised blood pressure and raised fasting blood glucose were the lowest in the Central (26.3%) and Eastern India (7.0%), respectively.118 Two state-wide risk factors surveys conducted in Punjab and Haryana suggest that the level of NCD risk factors is high and almost uniformly prevalent in both the states.119,120 The study revealed that around 60% of the people had at least one risk factor for NCDs, while less than 1% of the population was free from any of the risk factors for NCDs in the two states [Figure 1]. In Punjab and Haryana, alcohol consumption was observed in 15% and 11% of the population, respectively. Tobacco consumption was documented among 11.3% and 26.3%, respectively. The prevalence of overweight and obesity was 28.6% and 12.8% in Punjab and 25.7% and 9.4% in Haryana, respectively. The prevalence of diabetes was 14.3% and 15.5% in the two states. Hypertension was prevalent at 40.1% and 26.2%, respectively, in the two states. The mean sodium intake in grams per day for the population was 7.4 g and 8 g, respectively. In addition, 7% of the population aged 40–69 years had a cardiovascular risk of >30% over a period of the next ten years.
A study reported that all states show a declining trend in underweight and an increasing trend in overweight/obesity. An important aspect of NCDs is the existence of comorbidities. A study reported that 45% of people with hypertension and 35% of people with diabetes had dyslipidemia.121 Similar findings were reported in Punjab, obesity and dyslipidemia were the common comorbidities affecting patients with diabetes and hypertension alone and also in those with co-existing two diseases. Diabetes was found in 13% of hypertensive patients, whereas hypertension was seen among 60% of persons with diabetes.122 The results emphasize the role of non-pharmacological interventions such as weight reduction, physical activity, and dietary modification [Table 3].
| S. No | Indicators | Estimates for India (in %) (Data Source) |
|---|---|---|
| 1. | Prevalence of current alcohol consumption in adults aged 18+ years | 6 % (WHO NCD Country Profile 2018) |
| 2. | Prevalence of obesity among adults aged 18+years (defined as BMI >30 kg/m2) | 4% (WHO NCD Country Profile 2018) |
| 3. | Prevalence of raised blood glucose/diabetes among persons aged 18+ years (defined as fasting capillary glucose concentration ≥110 mg/dl) or on medication for raised blood glucose) | 8% (WHO NCD Country Profile 2018) |
| 4. | Prevalence of insufficiently physically active persons aged 18+ years (defined as less than 150 min of moderate intensity activity per week, or equivalent) | 33% (WHO NCD Country Profile 2018) |
| 5. | Prevalence of raised blood pressure among persons aged 18+ years (defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg) and mean systolic blood pressure | 24% (WHO NCD Country Profile 2018) |
| 6. | Mean population intake of salt (sodium chloride) per day in grams in persons aged 18+ years | 9.0 g/day(WHO NCD Country Profile 2018) |
| 7. | Prevalence of current tobacco use among persons aged 18+ years | 28.6% (GATS 2 India 2016–2017) |
| 8. | Prevalence of persons (aged 18+ years) consuming less than five total servings (400 g) of fruit and vegetables per day | NA |
| 9. | The proportion of eligible persons (defined as aged 40 years and older with a 10-year cardiovascular risk ≥30%, including those with existing cardiovascular disease) receiving drug therapy and counseling (including glycemic control) to prevent heart attacks and strokes | NA |
| 10. | The proportion of women between the ages of 30 and 49 screened for cervical cancer at least once, or more often, and for lower or higher age groups according to national programs or policies | NA |
| 11. | The proportion of women aged 30 years and above screened for breast cancer by clinical examination by trained health professionals at least once in a lifetime | NA |
| 12. | The proportion of high-risk persons (using tobacco, smoking and smokeless, and betel nut) screened for oral cancer by examination of the oral cavity | NA |
NA: Not available; NCD: Non-communicable diseases; GATS: ***; BMI: Body mass index.
Source: National monitoring framework Indicators of NCD burden for India.
Other risk factors for NAFLD:
The pathogenesis of NAFLD is multifactorial and involves environmental and genetic risk factors. At its core, NAFLD is primarily a lifestyle disease attributable to excess calorie intake (increased intake of calorie-dense foods, dietary sugars, particularly fructose, trans-fats, and “junk” food) and reduced expenditure (a sedentary lifestyle). In this context, it is important to highlight that dietary constituents and cooking media vary greatly in different regions of India. Further, many Indians consume a purely vegetarian diet, which is relatively rare in Western countries. The influence of diet on NAFLD in Indians is relatively unexplored. Limited Indian data suggest that there may not be any difference between vegetarian and mixed diets on the risk of NAFLD.123 Aerated soft drinks have been linked to an increased risk of NAFLD.124
Insulin resistance is the main driver of NAFLD pathogenesis in the vast majority of patients. Globally, multi-ethnic studies have suggested that Indians are more predisposed to insulin resistance and its consequences, including NAFLD. However, insulin resistance is not universal and some studies from the Eastern coastal areas of the Indian subcontinent have documented the absence of insulin resistance in almost half of the included patients.125,126 Given the central role of insulin resistance, it is not surprising that there is an intricate relationship between NAFLD and other metabolic syndrome components like obesity, T2DM, hypertension, and dyslipidemia. On the one hand, patients with NAFLD are more likely to have metabolic comorbidities. On the other hand, the increasing number of metabolic comorbidities increases the risk and severity of NAFLD. Indeed, NAFLD is often considered to be the hepatic component of metabolic syndrome. In the ongoing multi-centric study of the Indian consortium on NAFLD (ICON-D), metabolic syndrome was observed in 43%, and at least one metabolic risk factor was present in 93% of 3553 patients with NAFLD with the commonest being central obesity in 83%. Almost 90% of the patients were obese or overweight (BMI ≥ 23 kg/m2).127
A vexing issue in the field of NAFLD is that although most patients with NAFLD are overweight or obese, around 10%–20% of patients are lean and have normal BMI.128-132
This phenotype was first described in India and China and is now being recognized globally. Current evidence suggests that although these patients have less severe metabolic dysfunction than those with the classical NAFLD phenotype, they are metabolically unhealthy compared to individuals without NAFLD.128,129 Further, the disease severity appears to be similar in non-lean and lean NAFLD patients in the Indian subcontinent.130–132
The role of gut microbiome in lifestyle diseases:
The role of gut dysbiosis is being increasingly recognized in the pathogenesis of obesity and associated lifestyle diseases. In a small study with analysis of fecal samples from five people, each with lean, normal BMI, obese, and surgically treated obese Indians, Patil et al. reported higher levels of bacterial genus Bacteroides and of higher archeal density in obese Indians.133 Faecali bacteriumprausnitzii levels were higher in fecal samples from 15 obese 11–14-year-old South Indian children compared to 13 normal-weight children.134
Higher levels of Escherichia and Prevotella have been reported in fecal samples from 17 Indian T2DM subjects compared to higher levels of Faecalibacterium, Eubacterium, and Bifidobacterium in 13 non-diabetic subjects.135 Dysbiosis of the gut microbiome was reported by a study from Pune in 2017 with fecal samples from 14 newly diagnosed T2DM subjects, 16 long-standing T2DM subjects, and 19 healthy controls, mean age 48–52 years136 and another study from Hyderabad in 2021 with fecal samples from 25 T2DM, 28 T2DM with retinopathy, and 30 healthy controls, mean age 52–57 years.137 Interestingly, of the 11 taxa, the Pune study found to be discriminatory for T2DM (Oscillospira, Faecalibacterium prausnitzii, Bifidobacterium, Bifidobacterium adolescentis, Prevotellacopri, Lachnospiraceae, Lactobacillus ruminis, Ruminococcaceae, Roseburia, Collinsellaaerofaciens, and Streptocoocus), the Hyderabad study found only two of them, Roseburia and Lachnospira significantly reduced in abundance in T2DM, thereby underlining the need for gut microbiome studies with larger sample sizes adequately representing different geographical regions of the country that differ vastly in dietary and other cultural habits with domino effect on the gut microbiome composition. In another recent study, Gaike et al. reported that the gut microbial diversity of newly diagnosed diabetics but not of pre-diabetics was different from healthy controls, and anti-diabetic treatment in long-standing diabetics tended to reverse some of these changes.138 Akkermansia, Blautia, and Ruminococcus levels were significantly decreased, and Lactobacillus levels were increased in newly diagnosed diabetics compared to healthy controls. This dysregulation was recovered in long-standing diabetics. This study was done in Pune with fecal samples from 17 pre-diabetics, 11 newly diagnosed diabetics, 39 long-standing diabetics, and 35 healthy controls, with mean age ranging from 37 years for the healthy controls to 52 years for long-standing diabetics. In another recent study on Indians and Danes, fecal samples from 157 T2DM and 137 healthy control Indians were included.139 They reported increased levels of two operational taxonomic units (OTUs) from the Lachnospiraceae family and decreased levels of Subdoligranulum and Butyricicoccus in T2DM subjects.
Relations between dyslipidemia or CVD and gut microbiota composition in Indians has not been explored. One study to date has explored these relations in 71 Assamese individuals, reporting 19 amplicon sequence variants (ASVs) were discriminatory between 37 subjects with normal (<120 mmHg) and 34 subjects with elevated (≥120 mmHg) systolic blood pressure (SBP).140 Four ASVs from genus Prevotella, two ASVs from Megasphaera, and one ASV from Butyricicoccus, Prevotellaceae, Faecalibacterium, Lachnoclostridium, Howardella, and g-UCG04 had higher abundance in those with elevated SBP while three ASVs from genus Prevotella, two from Alloprevotella, and one from Streptococcus and g-UCG-05 had higher abundance in those with normal SBP.
Data from India on relations between the gut microbial composition and NAFLD are limited and indicate that small intestinal bacterial overgrowth, lipopolysaccharides, and toll-like receptor expression play a role in the pathogenesis of NAFLD.141 Further, in a proof of concept study, the administration of high-dose probiotics showed a beneficial effect in patients with NAFLD.142
CURRENT STRATEGIES FOR MANAGEMENT OF OBESITY AND LIFESTYLE DISEASES IN INDIA
Strategies at different levels of prevention
Primordial prevention: Primordial prevention is the adaptation of strategies to stop the emergence of the risk factors before they have appeared. The preventive measures comprise the maintenance of normal body weight through the adoption of healthy nutritional habits and physical exercise.143
Health promotion: Health promotion includes promoting a healthy lifestyle by choosing healthier foods (whole grains, fruits and vegetables, healthy fats, and protein sources) and beverages. Limiting unhealthy foods (refined grains and sweets, processed foods, etc.) and beverages (sugary drinks), increasing physical activity, limiting screen time, and other sedentary activities. The role of health authorities is to manipulate the obesogenic environment in favor of a healthy lifestyle environment, providing adequate space for physical activity. It is recommended that every adult and child must perform 30 min of daily physical activity for a minimum of 5 days a week.144 Stress management also plays an important role in preventing lifestyle diseases. Stress management activities like recreational activities and mindfulness may be utilized at community levels, in schools and workplaces.145 Screening for NCDs, including NAFLD should be performed in all individuals >30 years of age. It should be carried out at an earlier age in adults who have one or more of the following risk factors: Family history of diabetes, overweight/obese (BMI ≥23 kg/m2) or have increased WC (>90 cm males, >80 cm females), history of hypertension (≥130/80 mmHg) or on treatment for hypertension, history of dyslipidemia, sedentary physical activity, history of gestational diabetes or macrosomia (birth weight >3.5 kg), history of CVD (ischemic heart disease, cerebrovascular disease), history of polycystic ovarian syndrome, and/or acanthosis nigricans.146
Health education: Health education activity includes increasing the awareness of healthy lifestyle practices in people of younger age groups. Mass campaigns and awareness through print media, television, and social media platforms may be found to be a particularly useful tool for imparting health education. It is essential to educate the masses about the risk factors associated with lifestyle diseases. People should also be informed about health facilities provided by the government in the primary health-care centers and health and wellness centers to manage the risks of lifestyle diseases.147
Primary prevention: Primary prevention is possible during the stage of early pathogenesis phase of lifestyle diseases. For example, the pre-diabetes phase [impaired fasting glucose (IFG)/impaired glucose tolerance (IGT)] before the development of DM.148 In India, NCDs like CVD, cancer, chronic respiratory diseases, diabetes are estimated to account for around 60% of all deaths. The GOI has been implementing the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) since 2010 up to the District level under the National Health Mission. The main focus of NPCDCS is awareness generation for behavior and lifestyle changes, screening and early diagnosis of persons with a high level of risk factors, and their referral to appropriate treatment facilities, i.e., community health centers and district hospital for management of NCDs including CVDs. The strengthening of infrastructure for screening, early detection, treatment, and referral is also envisaged. Several newer initiatives have been taken like the initiation of NCD App for capturing patient-wise data and further follow-up from several districts. Under Ayushman Bharat, lifestyle diseases are included in the spectrum of services being offered at Health and Wellness Centres.149
Health promotion: Primary health-care centers may be equipped with lifestyle coaches who can educate the person with pre-diabetes to modify their lifestyle. Since primary healthcare centers have access to the local population, it is easy for Primary Health Centers (PHC's) to reach the patients and their families or follow them on a regular basis. It is essential to increase the trained individuals for health promotion activities and extension activities.150 Ayurveda and Yoga have been reported as strong health promotion strategies. Yoga is also popular in many sections and populations of our society. AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy) is widely integrated with allopathic medicine to promote cross-talk among systems. An evidence-based synergy and use of integrative health approach and lifestyle medicine for health promotion should be emphasized.
Secondary prevention: Preventive strategies that are carried out after obesity and lifestyle diseases have been detected to prevent or delay the development of long-term complications of the disease.
Early diagnosis and prompt treatment of lifestyle disease Once the person is diagnosed with obesity and lifestyle diseases, the objective of health management should be the prevention of other comorbidities associated with that disease. For example, for diabetes, regular monitoring of blood glucose - Fasting Plasma Glucose (FPG) and 2 hours post prandial plasma glucose (2 h PPPG) at least once a month and more often if values are not in the ideal target range, HbA1c at least every 6–12 months and more often (every three months) if values are not in the ideal target range, or tight control is being attempted. A clinical examination needs to be done during every visit—minimum every three months. Screening for long-term complications like retinopathy, nephropathy, neuropathy, peripheral vascular disease, and coronary artery disease at least once a year, more often if needed, optimizing weight, WC, blood pressure, lipids, routine examination of the foot to be done during every visit and education regarding foot care to be given to patients in each visit. Tobacco use and excessive use of alcohol need to be discouraged. Urine glucose monitoring is not recommended. Urine examination for estimation of ketones should be done if blood glucose is greater than 400 mg/dl.146
Prompt treatment: Pharmacological and non-pharmacological treatment may be provided to the person with obesity and lifestyle diseases. In addition, regular health check-ups help in responding to the development of any co-morbid condition and referral to any other specialist if needed.
Tertiary prevention: It is carried out at the stage when complications have already set in, with the aim of preventing the progression of these complications.
Disability limitation: Tertiary prevention seeks to reduce the impact of obesity and lifestyle diseases by eliminating or reducing disability, minimizing suffering, and maximizing potential years of quality life. In epidemiological terms, tertiary prevention aims to reduce the number and/or impact of complications. This is the task of therapy and rehabilitation.
Rehabilitation: Follow-up of chronically ill obesity and lifestyle diseases patients to ensure adherence to medication regimen, monitor changes, and assist them in maintaining independence in daily life; rehabilitation of patients to restore functions, such as through physiotherapy, and prevent recurrence or further complications through appropriate medication is an essential feature of rehabilitation.149
Strategies for existing health-care delivery system
Role of centers of excellence: These include a multidisciplinary approach with an effective system of service delivery, integration, and coordination of care between different services and service providers, support for self-management, evidence-based decision-making and clinical information systems, with the focus being on proactive maintenance of good health and complication prevention. Centers of excellence also actively bridge the gap between the acute care hospital system and the care provided by primary care and community services. These can act as model facilities which may develop a management protocol based on the latest technological advances and current research.
Role of tertiary care centers: Tertiary care centers are specialized for services comprising an interdisciplinary team of health professionals dedicated to the provision of education and clinical services for people with lifestyle diseases. The service need not be located at a single geographical location. In addition to the services provided at secondary care centers, tertiary care centers provide comprehensive care, including prevention, early detection, diagnosis, treatment, minimal access surgery, aftercare, palliative care, and rehabilitation.150
Role of secondary care centers: Secondary care centers in India provide a high standard of care and education for people with lifestyle diseases in an outpatient setting, but without the same level of specialist staffing as a tertiary service. A secondary care service is defined as a unit comprising a team of health professionals dedicated to the provision of education and clinical services for people with lifestyle diseases.
Role of primary care centers/Health and wellness centers: Primary care physicians or family physicians are the first level of contact between community and health services and are usually acceptable, available, and affordable to the community as well. A primary care physician with appropriate training and expertise can thus become a provider of diabetes care services to the vast majority of people. Today, most lifestyle disease care in India is provided by the private sector, but given the need for early screening and large numbers of those with significant out-of-pocket expenditure incurred by patients, there is a clear need for active involvement of the public health system through primary care physicians. In this setting, the responsibility of screening, early diagnosis, and management of diabetes is primarily assigned to the medical officer of the primary health center.151
National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS)
Activities under the program include:
-
–
Health promotion, including information education communication (IEC), social, and behavioral change communication
-
–
Screening including population screening for early case detection
-
–
Management, monitoring, and evaluation
-
–
Capacity building
-
–
Public–private partnership
-
–
Encourage innovations
-
–
Integration with other national programs
Activities under NPCDCS149,152 at different levels of healthcare delivery are detailed in the table 4 below.
| Level of health care | Health worker | Broad activities |
|---|---|---|
| Community level | ASHA |
Using the Community Based Assessment Checklist form, ASHA will ascertain the presence of:
Patients with diabetes or abdominal obesity will be referred to sub-health center as suspected NAFLD |
| Sub-health center | Multipurpose worker (MPW) or community health officer |
Patients with obesity or diabetes, validated by ANM, will be referred to the primary health center |
| Primary health center | Medical officer |
The patient will be referred to CHC if the medical specialist is available there or to the district hospital. |
| CHC levels | CHC medical officer |
|
| District hospital | Medical Officers |
Low risk for advanced fibrosis:
High risk of advanced fibrosis:
|
| State level | Medical Officers, specialists and health administrators |
|
| National level | Medical Officers, specialists and health administrators |
|
ASHA: Accredited Social Health Activist; NAFLD: Non Alcoholic Fatty Liver Disease; ANM:Auxiliary Nurse and Midwife; USG: Ultrasonography; MO: Medical Officer; CHC: Community Health Center; CBC: Complete Blood Count; FIB-4: Fibrosis-4; NFS score: NAFLD Fibrosis Score; PHC: Primary Health Center; HCC: Hepatocellular Carcinoma; IEC: Information, Education and communication.
Role of professionals in preventing lifestyle disorders
Role of specialists: The Endocrinologist/Diabetologist/ Hepatologist/Gastroenterologist are the treating specialists who have a special interest, training, experience, and expertise in the comprehensive management of lifestyle diseases. Their role is multifaceted. They command clinical leadership in treating the patient in terms of deciding the line of treatment, prescribing appropriate medications, and provide an effective triage of protocol-based referrals to other specialists as per the patient’s requirement. They also steer the diabetes team to optimally utilize all the available resources (human and material) in providing their patient with an effective and efficient support system in managing diabetes and preventing comorbidities.
Role of physicians: They should set up structured goals with clear clinical indicators to achieve the goals like:
Identifying patients eligible for treatment at the primary care level and early diagnosis of diabetes.
Facilitates glycemic control to prevent or delay complications.
Identifying patients with IFG and IGT and follow them up.
Routine investigation and clinical examination for early detection of complications and CV risks.
Encouraging patient’s self-management and special group identification, e.g., children and pregnant women with appropriate referral.
Identifying those with high CV risk, complications, and poor metabolic control and refer to them.
Providing optimal, evidence-based care to the patients according to the latest guidelines.
Role of nurses: The Diabetes Nurse will be providing primary, secondary, and tertiary care. The diabetic patients’ problems will be addressed, whether they are physical, psychological, or social. They practice their skills in communication, counseling, and educating patients. Their care will not be confined to the patient but will include the family and the community. The nurses’ clinical skills and expertise when educating and counseling diabetics improve the care and reduce the cost of health care. This can be provided either by individual or group education. Their role includes assessing the patient’s learning needs and then setting realistic goals for management supported by the latest evidence. They keep complete informative nursing records and may also contribute in research relevant to their role.
Role of community health workers: Community health workers play a very important role in reaching out to community members. They help in screening the community members on the basis of the protocol developed for community members. Once the screening process is done and any person is diagnosed with lifestyle diseases, the community health worker can help in referring the patient to primary care physicians. After the beginning of treatment, follow-ups are particularly important to prevent further comorbidities, here, community health workers may play a very important role in facilitating the follow-ups of the patients with lifestyle diseases.
To address the grim scenario MoHFW, GOI has rolled out a population-based initiative for prevention, control, and screening for common NCDs, i.e., diabetes, hypertension, and common cancers under NHM and also as a part of Comprehensive Primary Health Care. Under the initiative, persons more than 30 years of age are targeted for their screening for the common NCDs, with a special focus for screening of breast cancer and cervical cancer among women.
The screening of these common NCDs is an integral part of service delivery under Ayushman Bharat-Health and Wellness Centres (AB-HWC). A community based assessment checklist (CBAC) has been put together to be used by grass-root level health workers (ASHAs) to collect information from the community to help screen individuals above 30 years of age vulnerable to the risk of NCDs and facilitate early detection and diagnosis along with timely administration of required health interventions such as treatment and/or behavior changes communication. The CBAC form comprises of three parts: Part A is for risk assessment of NCDs; Part B is for early detection of illnesses like TB, leprosy, precancerous oral lesions (Oral sub-mucosa fibrosis, erythroplakia, lichen planus, leukoplakia, etc.), and for breast and cervical cancer in women; Part C is for determining exposure to risk factors for chronic respiratory diseases.
KNOWLEDGE GAPS AND RECOMMENDATIONS FOR OBESITY AND LIFESTYLE DISEASES IN INDIA
The presence of NCD risk factors at high proportions calls for stepping up of responses on priorities for immediate and future policy-making. Population and high-risk strategies with multi-sectoral participation are mainly used for the prevention and control of lifestyle diseases. The following strategies and activities are recommended:
There is still a paucity of literature on the prevalence of obesity in India. The fast-developing transition from rural to urban areas, especially in recent years, has surpassed the available information on available statistics used in this document. There is an urgent need to carry out large-scale studies, especially including samples from different regions of the country to estimate the current trend of obesity in India.
Prioritizing hypertension and diabetes management as an entry point for NCD prevention and control efforts is required. A tracking system for diabetes and hypertension cases can be developed.
Metabolically healthy obese and metabolically unhealthy obese are terms that are not clearly defined in literature. They need to be defined by experts and studies before becoming a part of any guideline.
The role of gut dysbiosis in lifestyle diseases needs to be more granularly studied. Apart from adequate sample size, studies should ensure appropriate methodology and statistical adjustments to account for confounders, including the effect of diet and medications (like antibiotics) on gut microbiota and its inherent dynamic nature.
IEC/BCC activities need to be strengthened to generate public awareness about the harmful consequences of poor dietary habits, physical inactivity, tobacco use, and obesity.
A Setting-based approach in health promotion should be adopted. One of the key strategies under the NPCDCS program is to design school-based and workplace-targeted interventions. This component needs to be strengthened and requires adequate attention and resources.
Culturally appropriate state-wide strategies need to be adopted to respond to promote fruit/vegetables consumption, which is low despite enough availability. Promoting a healthy diet requires a multi-sectoral approach with active participation of health, agriculture, and food industry sectors.
Regulations need to be put in place to control the content of salt, sugar, saturated fats, and trans-fats in diet. Policy dialog should be initiated to increase GST/tax on fast foods as an effort to regulate fast food consumption. Millets and other healthier food should be promoted.
There is a need to replace and harmonize vertical single risk factor surveys with comprehensive state-level surveys for studying variations within the country and arrive at an appropriate NCD research agenda which is relevant to the local needs and setting up of national NCD surveillance units under Ministry of Health and Family Welfare, GOI to primarily gather, analyze, and report timely data for action and closely liaison with the stakeholders for interventions periodically.
Considering the large existing diversity amongst Indians, in terms of multiple ancestral populations and admixed groups as well as diversity of environmental factors such as dietary habits, future region-specific genetic and epigenetic studies with large sample sizes that incorporate simultaneous deep phenotyping of the subjects are the need of the hour, to improve our understanding of the modifiable factors affecting the onset and progression of obesity and associated lifestyle diseases, including T2DM, hypertension, metabolic syndrome, and NAFLD in India. Further, the exploration of biological function and associated consequences of the identified variants in a country-specific context will lead to the translation of this knowledge into improving prevention, diagnosis, and development of focused therapeutic approaches.
GOI has long instituted measures to prevent and control NCD risk factors in the country by several programs and introducing the National Programme for Prevention and Control of Cancer, diabetes, CVDs and Stroke (NPCDCS), however, it is important that the continuum of care is maintained and the people screened are on treatment and their status for the disease is controlled.
Knowledge gaps and recommendations for NAFLD in India
Dietary practices, physical inactivity, and other risk factors: Dietary constituents vary greatly across the different regions of India [Table 5]. A substantial proportion of our population are pure vegetarians. Cooking media like mustard oil and coconut oil, which are commonly used in East and South India are seldom used in Western diet. Further, the predominant dairy product in the Western diet is cheese, while ghee (clarified butter) is traditional in India. The impact of various dietary constituents on the risk of NAFLD in Indian patients’ needs to be looked at in granular detail. A sedentary lifestyle and physical inactivity is a well-established risk factors of NAFLD, but data from India are limited. Barriers to the adoption of a healthier, active lifestyle need to be identified. Other risk factors like gut microbiota, chronic stress, disturbances of the circadian rhythm, lack of sleep, and poor sleep quality have been implicated in metabolic diseases, including some evidence in NAFLD.153–156 However, more data need to be generated among Indian patients.
Screening for NAFLD: Apart from those with derangement in liver function tests, current guidelines from expert societies also suggest screening for NAFLD in patients with obesity, T2DM, or metabolic syndrome.157 The feasibility and cost-effectiveness of a targeted screening approach in the community setting in India needs to be looked at in future studies. Further, apart from classical metabolic syndrome comorbidities, other conditions like hypothyroidism, polycystic ovarian syndrome, etc., have also been found to be significantly associated with NAFLD. Whether such patients also need to be targeted for screening remains unknown and needs to be holistically assessed. The modality for screening should be sensitive, reliable, cost-effective, and widely available. Despite sub-optimal sensitivity and observer dependence, ultrasound abdomen is commonly recommended as the modality of choice for NAFLD screening as it is relatively cheap and widely available. Nonetheless, it may not be available in primary care centers. Non-imaging scores for predicting the presence of steatosis based on clinical risk factors and blood parameters like fatty liver index, hepatic steatosis index, etc., have not been validated in Indian patients.
Risk stratification: It is clear that risk stratification of NAFLD should be based on an assessment of fibrosis. Use of non-proprietary blood-based scores like APRI and FIB-4 appear to be the most cost-effective approach for guiding referral of high-risk patients from primary and secondary health-care centers to tertiary centers. This approach needs to be corroborated in future studies. For the implementation of this approach, there is an urgent need to define cut-offs and further validate these scores in larger cohorts of Indian patients.
Screening for cardiovascular, renal dysfunction, and HCC in NAFLD: The commonest cause of mortality in patients with NAFLD is cardiovascular. Indeed, NAFLD has been shown to be an independent risk factor for not only CVD but also chronic kidney disease, malignancies, and several other extrahepatic diseases. Optimal strategies of screening for these diseases in patients with NAFLD need to be devised, including who to screen, at what age to initiate screening assessment, and the modality for screening. The majority of patients with NAFLD-HCC have underlying cirrhosis, and all patients with NAFLD-cirrhosis should be screened for HCC. However, it is now being recognized that a substantial proportion of patients with NAFLD-HCC may not have underlying cirrhosis. The risk of developing HCC in non-cirrhotic NAFLD and the cost-effectiveness of screening these patients is unknown in the Indian setting.
Role of yoga: Exercise is one of the central pillars for the management of NAFLD. The ancient Indian tradition of yoga entails much more than exercise and aims to holistically control both the body and the mind. It may potentially benefit patients with NAFLD, and assessment of yoga in patients with NAFLD should be a priority area for research.
Role of coffee and tea: Coffee has been shown to have several beneficial effects in NAFLD. However, Indian data is practically non-existent. This is particularly important, and the beneficial effects have been mainly demonstrated with “black” coffee, while many Indians add sugar and milk or dairy whiteners to their coffee, which may be potentially counteractive. Tea is also rich in antioxidants and is popular in India. Studies are required to evaluate the effect of these beverages in Indian patients.
Pharmacotherapy: Pharmacotherapy in NASH is evolving. Although saroglitazar has been approved by DCGI for NASH with F1-F3 fibrosis and NAFLD with metabolic comorbidities, there is a need to generate more data from robust clinical trials. Vitamin E and pioglitazone are currently recommended only in biopsy-proven NASH, and there is a need to identify patients who may benefit from pharmacotherapy with non-invasive assessment. Assessment of response to pharmacotherapy and the duration till which pharmacotherapy is to be continued are other lacunas in our knowledge that are extremely relevant for the clinical management of these patients.
Lean NAFLD: Although only 10%–20% of Indian patients with NAFLD are lean, the burden of lean NAFLD is still likely to be substantial given the large population of India and the astoundingly high prevalence of NAFLD in the community. There is a need to better assess the prevalence of NAFLD among lean individuals in the community setting and to identify the risk factors for this intriguing phenotype. The management of these patients who have normal body weight remains another vexing issue since weight loss is the main target for the management of NAFLD.
| What is known | Lacunae, which is the way forward |
|---|---|
| Obesity (BMI-based) as a risk factor for lifestyle diseases |
|
| Calorie imbalance is the main cause of weight gain |
|
| High calories and high % of carbohydrates increase the risk lifestyle diseases |
|
| High intake of oil intake is a risk factor |
|
| Less vegetables and legumes is a risk factor |
|
| Non-vegetarianism (more meat) increases the risk |
|
| Increased physical activity decreases the risk of lifestyle disease by 27% independent of diet |
|
| South Asians including Indians have 50%–75% less physical activities compared to Europeans |
|
BMI: Body mass index; NALFD: ***; Ob: ***; DM: ***; MeS: ***.
Acknowledgements
ACKNOWLEDGMENT
We are grateful for the encouragement and support provided by the President NAMS, Prof SK Sarin, and Prof Umesh Kapil, Secretary NAMS and his Secretariat team, through the duration of the Task Force. We profusely thank all the Task Force chairman and members for their invaluable contribution to the various sections and collecting evidence with an overarching. view to present an easy-to-refer format for primary care physicians in the Indian context. The contributions made by various domain experts in the fields of Gastroenterology, Hepatology, General Physicians, Public Health Experts, Metabolic Research Scientists, Clinical Nutritionists, Research Labs, the Ministry of Health & Family Welfare.- Dr. Arpita Mukhopadhyay, Associate Professor, Molecular Nutrition and Physiology, St John’s Medical College, Bengaluru, India
- Ms Kanika Jain, Clinical Nutrition, ILBS New Delhi
- Dr. Rohit Katre, Senior Resident, CFM, AIIMS Rishikesh
DEFINITION OF OPERATIONAL TERMS USED IN THE REPORT
-
Overweight and Obesity (WHO Asia-Pacific).
- Overweight is defined as a BMI ≥23 kg/m2 but <25 kg/m2 for both genders with or without abdominal obesity.
- Generalized obesity is defined as a BMI ≥25 kg/m2 for both genders with or without abdominal obesity.
- Abdominal obesity is defined as a waist circumference (WC) ≥90 cm for men and ≥80 cm for women with or without generalized obesity.
- Isolated generalized obesity is defined as a BMI ≥25 kg/m2 with waist circumference of <90 cm in men and <80 cm in women.
- Isolated abdominal obesity is defined as a waist circumference of ≥90 cm in men or ≥80 cm in women with a BMI <25 kg/m2.
- Combined obesity refers to individuals with both generalized obesity and abdominal obesity.
- Non-obese subjects refer to individuals without either generalized obesity or abdominal obesity.
-
Diabetes: As per the American Diabetes Association 2022
Pre-diabetes Diabetes HbA1C 5.7–6.4% ≥6.5% Fasting plasma glucose 100–125 mg/dL ≥126 mg/dL 2-h plasma glucose during 75 g OGTT 140–199 mg/dL ≥200 mg/dL Random plasma glucose — ≥200 mg/dL HbA1c: Hemoglobin A1C; OGTT: Oral Glucose Tolerance Test. - Hypertension: The diagnosis of hypertension should be based on an office blood pressure reading of >140/90.
-
Metabolic Syndrome (as per NCEP ATP III and IDF). Any three of the following five features:
- Increased waist circumference (Men ≥90 cm, Women ≥80 cm).
- Triglyceride ≥150 mg/dL or TG treatment.
- HDL-C < 40 mg/dL (Men); < 50 mg/dL (Women).
- Blood pressure Systolic ≥130 mmHg or Diastolic ≥85 mmHg or hypertension treatment or previously diagnosed hypertension.
- Fasting blood glucose ≥100 mg/dL or treatment for elevated glucose or previously diagnosed Type 2 Diabetes).
- Non-Alcoholic Fatty Liver Disease (NAFLD)
LIST OF ABBREVIATIONS
ADA: American Diabetes Association AIIMS: All India Institute of Medical Sciences ALD: Alcoholic Liver Disease BMI: Body Mass Index CAP: Controlled attenuated parameter CLD: Chronic Liver Disease CURES: Chennai Urban Rural Epidemiology Study DAA: Directly Acting Antivirals FBG: Fasting Blood Glucose GOI: Government of India HbA1C: Hemoglobin A1C HCC: Hepatocellular Carcinoma HDLC: High-Density Lipoprotein Cholesterol ICMR–INDIAB: Indian Council of Medical Research–India Diabetes IDF: International Diabetes Federation ILBS: Institute of Liver and Biliary Sciences MOHFW: Ministry of Health and Family Welfare MTCT: Mother to Child Transmission NAFLD: Non-Alcoholic Fatty Liver Disease NCD: Non-Communicable Disease NFHS: National Family Health Survey NSAIDS: Non-Steroidal Anti-Inflammatory Drugs NCEP ATP III: National Cholesterol Education Programs Adult Treatment Panel III OGTT: Oral Glucose Tolerance Test PGIMER: Postgraduate Institute of Medical Education & Research TG: Triglycerides TF: Task Force USG: Ultrasonography WC: Waist Circumference WHO: World Health OrganizationREFERENCES
- Management of obesity: A national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2010. p. :1-85. Available from: www.sign.ac.uk
- The Asia Pacific perspective: Redefining obesity and its treatment. St Leonards, Australia: Health Communications Australia Pty Limited; 2000. p. :22-9.
- European guidelines for obesity management in adults. Obes Facts. 2015;8:402-24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National Family Health Survey (NFHS-3), 2005-06, India. Vol Vol. I. Mumbai: IIPS; 2007.
- Obesity is major determinant of coronary risk factors in India: Jaipur heart watch studies. Indian Heart J. 2008;60:26-33.
- [PubMed] [Google Scholar]
- Determinants of urban-rural differences in cardiovascular risk factors in middle-aged women in India: A cross-sectional study. Int J Cardiol. 2013;163:157-62.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and significance of generalized and central body obesity in an urban Asian Indian population in Chennai, India (CURES: 47) Eur J Clin Nutr. 2009;63:259-67.
- [CrossRef] [PubMed] [Google Scholar]
- Healthy weight, nutrition, and physical activity. About child & teen BMI. CDC. Available from: http://www.cdc.gov/nccdphp/dnpa/healthyweight/assessing/bmi/childrens_BMI/about_childrens_BMI.htm
- Childhood obesity in India: A meta-analysis. Indian J Pediatr. 2012;79:945-8.
- [CrossRef] [PubMed] [Google Scholar]
- 2022. [accessed 2022 Aug 24]. Available from: https://idf.org/our-network/regions-members/south-east-asia/members/94-india.html
- Epidemiology of type 2 diabetes in India. Indian J Ophthalmol. 2021;69:2932-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of childhood diabetes. In: Das AK, Kalra S, eds. CDiC textbook of pediatric diabetes. New Delhi (India): Jaypee; 2018. p. :8-20.
- [Google Scholar]
- Type 2 diabetes in Asian-Indian urban children. Diabetes Care. 2003;26:1022-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of glucose intolerance among children and adolescents in urban South India (ORANGE-2) Diabetes Technol Ther. 2012;15:13-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of pre-diabetes/type 2 diabetes among adolescents (10–19 years) and its association with different measures of overweight/obesity in India: A gendered perspective. BMC Endocr Disord. 2021;21:146.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comprehensive National Nutrition Survey 2016–2018. 2019.
- Prevalence of prediabetes in children and its association with risk factors. Int J Contemp Pediatr. 2019;6:1957.
- [Google Scholar]
- Random blood glucose concentrations and their association with body mass index in indian school children. Indian J Endocrinol Metab. 2019;23:529-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global status report on non-communicable diseases 2014. WHO 2014 [accessed 2022 Aug 22]. Available from: http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1
- Prevention and control of non-communicable diseases: Status and strategies July, 2003 Working paper no. 104. Indian Council for Research on International Economic Relations
- Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019;71:309-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence, awareness, treatment, and control of hypertension in young adults (20–39 years) in Kerala, South India. Front Cardiovasc Med. 2022;9:765442.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An overview on management of diabetic dyslipidemia. J Diabetes Endocrino. 2013;4:27-36.
- [Google Scholar]
- Dyslipidemia in Asian Indians: Determinants and significance. Japi. 2004;52:137-42.
- [PubMed] [Google Scholar]
- Prevalence of dyslipidemia in urban and rural India: The ICMR–INDIAB study. PloS one. 2014;9:e96808.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of dyslipidemia and hypertension in Indian type 2 diabetic patients with metabolic syndrome and its clinical significance. Osong public health and research perspectives. 2014;5:169-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of dyslipidemia in South Indian adults: An urban-rural comparison. Int J Community Med Public Health. 2016;3:2201-10.
- [Google Scholar]
- Assessment of bone turnover markers to predict mineral and bone disorder in men with pre-dialysis non-diabetic chronic kidney disease. Clin Chim Acta. 2017;469:195-200.
- [CrossRef] [PubMed] [Google Scholar]
- Global nutrition dynamics: The world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84:289-98.
- [CrossRef] [PubMed] [Google Scholar]
- Global status report on noncommunicable diseases 2014. 2014.
- Prevalence of metabolic syndrome and gender differences. Bioinformation. 2012;8:613.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of metabolic syndrome among adult population in India: A systematic review and meta-analysis. PLoS One. 2020;15:e0240971.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-alcoholic fatty liver disease and metabolic syndrome-position paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of Gastroenterology. J Clin Exp Hepatol. 2015;5:51-68.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Natural history of simple steatosis or nonalcoholic fatty liver. J Clin Exp Hepatol. 2020;10:255-262.
- [Google Scholar]
- Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84.
- [CrossRef] [PubMed] [Google Scholar]
- Nonalcoholic fatty liver disease: Indian perspective. Clin Liver Dis (Hoboken). 2021;18:158-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of non-alcoholic fatty liver disease in India: A systematic review and meta-analysis. J Clin Exp Hepatol. 2022;12:818-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A community-based study to determine the prevalence of nonalcoholic fatty liver disease (NAFLD) and its metabolic risk factors in urban and rural communities of North India. J Gastroenterol Hepatol. 2019;34:72-582.
- [Google Scholar]
- Cohort profile: The Trivandrum non-alcoholic fatty liver disease (NAFLD) cohort. BMJ Open. 2019;9:e027244.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Study of prevalence of nonalcoholic fatty liver disease (NAFLD) in type 2 diabetes patients in India (SPRINT) J Assoc Physicians India. 2013;61:448-53.
- [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease in children: An emerging public health problem in India. Indian J Community Health. 2020;32:330-6.
- [Google Scholar]
- Prevalence of obesity in India: A systematic review. Diabetes Metab Syndr. 2019;13:318-21.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity in children: Definition, etiology and approach. Indian J Pediatr. 2018;85:463-71.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary patterns in India and their association with obesity and central obesity. Public Health Nutr. 2015;18:3031-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Major dietary patterns and their associations with cardiovascular risk factors among women in West Bengal, India. Br J Nutr. 2011;105:1520-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of high-protein meal replacement on weight and cardiometabolic profile in overweight/obese Asian Indians in North India. Br J Nutr. 2017;117:1531-40.
- [CrossRef] [PubMed] [Google Scholar]
- Type of vegetarian diet, obesity and diabetes in adult Indian population. Nutr J. 2014;13:89.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A study of physical activity levels and its correlates among adults: A cross-sectional study. Int J Community Med Public Health. 2017;4:1154-8.
- [Google Scholar]
- Epidemiologic study of diet and coronary risk factors in relation to central obesity and insulin levels in rural and urban populations of North India. Int J Cardiol. 1995;47:245-55.
- [CrossRef] [PubMed] [Google Scholar]
- Association of breakfast intake with obesity, dietary and physical activity behavior among urban school-aged adolescents in Delhi, India: Results of a cross-sectional study. BMC Public Health. 2012;12:881.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- [accessed 2016 Apr 21]. Available from: https://www.who.int/publications/i/item/9789241565257
- Epidemiology of type 2 diabetes in India. Indian J Ophthalmol. 2021;69:2932-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nagendra is the indian dietary pattern associated with type 2 diabetes? A Pan-India randomized cluster sample study. Ann Neurosci. 2020;27:175-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Slowing the diabetes epidemic in the world health organization South-East Asia region: The role of diet and physical activity. WHO South East Asia J Public Health. 2016;5:5-16.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 2018;361:k2234.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Obesity, the metabolic syndrome, and type 2 diabetes in developing countries: Role of dietary fats and oils. J Am Coll Nutr. 2010;29:289S-301S.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet. 2014;383:1999-2007.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Physical activity patterns among South-Asian adults: A systematic review. Int J Behav Nutr Phys Act. 2013;10:116.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Socio-demographic patterning of physical activity across migrant groups in India: Results from the Indian migration study. PLoS One. 2011;6:e24898.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Physical activity and inactivity patterns in India - results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5] Int J Behav Nutr Phys Act. 2014;11:26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of lifestyle risk factors with metabolic syndrome components: A cross sectional study in Eastern India. Int J Prev Med. 2018;9:6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Refined grain consumption and the metabolic syndrome in urban Asian Indians (Chennai Urban Rural Epidemiology Study 57) Metabolism. 2009;58:675-81.
- [CrossRef] [PubMed] [Google Scholar]
- Association of physical inactivity with components of metabolic syndrome and coronary artery disease—the Chennai Urban Population Study (CUPS no. 15). Diabetes UK. 2005. Diabetic Medicine. 2005;22:1206-1211.
- [Google Scholar]
- High prevalence of metabolic syndrome among urban subjects in India: A multisite study. Diabetes Metab Syndr. 2014;8:156-61.
- [CrossRef] [PubMed] [Google Scholar]
- Development of food group tree-based analysis and its association with non-alcoholic fatty liver disease (NAFLD) and co-morbidities in a South Indian population: A Large case-control study. Nutrients. 2022;14:2808.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors associated with non-alcoholic fatty liver disease in Indians: A case–control study. J Clin Exp Hepatol. 2015;5:295-302.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nutritional assessment in obese children with and without NAFLD in an urban area of Punjab, India. Indian Journal of Public Helath Research and Development. 2018;9:219-22.
- [Google Scholar]
- Nutrition and physical activity in Asian Indians with non-alcoholic fatty liver: A case control study. Diabetes MetabSyndr. 2019;13:1271-74.
- [CrossRef] [PubMed] [Google Scholar]
- A case-control study on nutritional risk factors in non-alcoholic fatty liver disease in Indian population. Eur J Clin Nutr. 2011;65:533-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of exercise on NAFLD and its risk factors: comparison of moderate versus low intensity exercise. Journal of Clinical and Translational Hepatology. 2020;8:120-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National Family Health Survey (2016). [accessed 2017 Jun 13]. Available at: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf
- Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126:1477-1500.
- [CrossRef] [PubMed] [Google Scholar]
- Genetics of obesity. Indian J Clin Biochem. 2016;31:361-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Multifaceted genome-wide study identifies novel regulatory loci in SLC22A11 and ZNF45 for body mass index in Indians. Mol Genet Genomics. 2020;295:1013-26.
- [CrossRef] [PubMed] [Google Scholar]
- Replication and relevance of multiple susceptibility loci discovered from genome wide association studies for type 2 diabetes in an Indian population. PLoS One. 2016;11:e0157364.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case-control analysis of SNPs in GLUT4, RBP4 and STRA6: Association of SNPs in STRA6 with type 2 diabetes in a South Indian population. PLoS One. 2010;5:e11444.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Variants in KCNQ1 increase type II diabetes susceptibility in South Asians: A study of 3,310 subjects from India and the US. BMC Med Genet. 2011;12:18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of genetic variants in INS (rs689), INSR (rs1799816) and PP1G.G (rs1799999) with type 2 diabetes (T2D): A case–control study in three ethnic groups from North-West India. Mol Genet Genomics. 2016;291:205-16.
- [CrossRef] [PubMed] [Google Scholar]
- Genome-wide association study for type 2 diabetes in Indians identifies a new susceptibility locus at 2q21. Diabetes. 2013;62:977-86.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Replication of newly identified type 2 diabetes susceptible loci in Northwest Indian population. Diabetes Res Clin Pract. 2017;126:160-3.
- [CrossRef] [PubMed] [Google Scholar]
- Angiotensin converting enzyme gene polymorphism (insertion/deletion) and hypertension in adult Asian Indians: A population-based study from Calcutta, India. Human Biology. 2008;80:303-12.
- [CrossRef] [PubMed] [Google Scholar]
- Association of DD genotype of angiotensin-converting enzyme gene (I/D) polymorphism with hypertension among a North Indian population. J Community Genet. 2018;9:51-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of angiotensin converting enzyme gene insertion/deletion polymorphism with essential hypertension in south Indian population. Genes Dis. 2016;3:159-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of the -344C/T aldosterone synthase (CYP11B2) gene variant with hypertension and stroke. J Neurol Sci. 2010;296:34-8.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial nitric oxide synthase gene polymorphisms and the risk of hypertension in an Indian population. Biomed Res Int. 2014;2014:793040.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Gender-related association of AGT gene variants (M235T and T174M) with essential hypertension--a case-control study. Clin Exp Hypertens. 2012;34:38-44.
- [CrossRef] [PubMed] [Google Scholar]
- Association of ACE, FABP2 and GST genes polymorphism with essential hypertension risk among a North Indian population. Ann Hum Biol. 2015;42:461-9.
- [CrossRef] [PubMed] [Google Scholar]
- Polymorphisms in the fatty acid-binding protein 2 and apolipoprotein C-III genes are associated with the metabolic syndrome and dyslipidemia in a South Indian population. J Clin Endocrinol Metab. 2005;90:1705-11.
- [CrossRef] [PubMed] [Google Scholar]
- TCF7L2 polymorphisms are associated with type 2 diabetes in Khatri Sikhs from North India: Genetic variation affects lipid levels. Ann Hum Genet. 2008;72:499-509.
- [CrossRef] [PubMed] [Google Scholar]
- INDICO Genome-wide association study of metabolic syndrome reveals primary genetic variants at CETP locus in Indians. Biomolecules. 2019;9:321.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetic variants of resistin and its plasma levels: Association with obesity and dyslipidemia related to type 2 diabetes susceptibility. Genomics. 2019;111:980-5.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic variants of tumor necrosis factor-α and its levels: A correlation with dyslipidemia and type 2 diabetes susceptibility. Clin Nutr. 2019;38:1414-22.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic association of ADIPOQ gene variants (-3971A > G and +276G > T) with obesity and metabolic syndrome in North Indian Punjabi population. PLoS One. 2018;13:e0204502.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A genetic analysis identifies a haplotype at adiponectin locus: Association with obesity and type 2 diabetes. Sci Rep. 2020;10:2904.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Transbilayer lipid interactions mediate nanoclustering of lipid-anchored proteins. Cell. 2015;161:581-94.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The prevalence and incidence of NAFLD worldwide: A systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7:851-861.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of non-alcoholic fatty liver disease in India: A systematic review and meta-analysis. J Clin Exp Hepatol. 2022;12:818-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetic predisposition in nonalcoholic fatty liver disease. Clin Mol Hepatol. 2017;23:1-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetic and epigenetic disease modifiers: Non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease (ALD) Transl Gastroenterol Hepatol. 2021;6:2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A sequence variation (I148M) in PNPLA3 associated with nonalcoholic fatty liver disease disrupts triglyceride hydrolysis. J Biol Chem. 2010;285:6706-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2014;46:352-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Inactivation of Tm6sf2, a gene defective in fatty liver disease, impairs lipidation but not secretion of very low density lipoproteins. J Biol Chem. 2016;29:10659-76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Correlates and heritability of nonalcoholic fatty liver disease in a minority cohort. Obesity. 2009;17:1240-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of european descent. Gastroenterology. 2016;150:1219-1230.e6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetic and epigenetic regulation in nonalcoholic fatty liver disease (NAFLD) Int J Mol Sci. 2018;19:911.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of peroxisome proliferator activated receptor-γ gene with non-alcoholic fatty liver disease in Asian Indians residing in North India. Gene. 2013;512:43-7.
- [CrossRef] [PubMed] [Google Scholar]
- SREBP-2 1784 G/C genotype is associated with non-alcoholic fatty liver disease in North Indians. Dis Markers. 2011;31:371-7.
- [CrossRef] [PubMed] [Google Scholar]
- Susceptibility and gene interaction study of the angiotensin II type 1 receptor (AGTR1) gene polymorphisms with non-alcoholic fatty liver disease in a multi-ethnic population. PLoS One. 2013;8:e58538.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exome-wide scan identifies significant association of rs4788084 in IL27 promoter with increase in hepatic fat content among Indians. Gene. 2013;775:145431 (x).
- [CrossRef] [PubMed] [Google Scholar]
- The GenomeAsia 100K Project enables genetic discoveries across Asia. Nature. 2019;576:106-111.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heterogeneity of dietary practices in India: Current status and implications for the prevention and control of type 2 diabetes. Eur J Clin Nutr. 2023;77:145-55.
- [CrossRef] [PubMed] [Google Scholar]
- GBD compare–Viz Hub. Noncommunicable Diseases. Both sexes, all ages, 2019, total percent of deaths: IHME GHDx, Hub Viz.; 2019. Available from: https://vizhub.healthdata.org/gbd-compare/
- India’s escalating burden of non-communicable diseases. The Lancet Global Health. 2018;6:e1262-e3.
- [CrossRef] [PubMed] [Google Scholar]
- National noncommunicable disease monitoring survey (NNMS) in India: Estimating risk factor prevalence in adult population. PloS one. 2021;16:e0246712.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Regional estimates of noncommunicable diseases associated risk factors among adults in India: Results from national noncommunicable disease monitoring survey. BMC Public Health. 2022;22:1069.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-communicable diseases risk factors and their determinants: A cross-sectional state-wide STEPS survey, Haryana, North India. PloS one. 2019;14:e0208872.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Profile of risk factors for non-communicable diseases in Punjab, Northern India: Results of a state-wide STEPS survey. PLoS ONE. 2016;11:e0157705.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diet and nutritional status of urban population in india and prevalence of obesity, hypertension, diabetes and hyperlipidemia in urban men and women. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research, 2017.
- Prevalence and determinants of comorbid diabetes and hypertension: Evidence from non communicable disease risk factor STEPS survey, India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2017;11:S459-S65.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease prevalence and associated risk factors--A study from rural sector of Maharashtra. Trop Gastroenterol. 2015;36:25-30.
- [CrossRef] [PubMed] [Google Scholar]
- Soft drinks consumption and the risk of nonalcoholic fatty liver disease. J Assoc Physicians India. 2017;65:28-32.
- [PubMed] [Google Scholar]
- Nonalcoholic fatty liver disease (NAFLD) without insulin resistance: Is it different? Clin Res Hepatol Gastroenterol. 2015;39:482-8.
- [CrossRef] [PubMed] [Google Scholar]
- Insulin resistance in nonalcoholic fatty liver disease: Experience from Bangladesh. Bangladesh Critical Care Journal. 2016;4:86-91.
- [Google Scholar]
- Clinicopathological profile and outcome of a large cohort of patients with nonalcoholic fatty liver disease from South Asia: Interim results of the Indian consortium on nonalcoholic fatty liver disease. Metab Syndr Relat Disord. 2022;20:166-173.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease in lean individuals. JHEP Rep. 2019;1:329-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-Alcoholic fatty liver disease in lean and non-obese individuals: Current and future challenges. Biomedicines. 2021;9:1346.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Patients with metabolic-dysfunction associated fatty liver disease (MAFLD) without associated etiologies and non-MAFLD non-alcoholic fatty liver disease (NAFLD) have similar liver disease severity - Data from Indian Consortium on NAFLD (ICON-D) J Clin Exp Hepatol. 2022;12:S73-S74.
- [Google Scholar]
- Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: Do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J Endocrinol Metab. 2013;17:665-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical, anthropometric, biochemical, and histological characteristics of nonobesenonalcoholic fatty liver disease patients of Bangladesh. Indian J Gastroenterol. 2014;33:452-7.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular analysis of gut microbiota in obesity among Indian individuals. J Biosci. 2012;37:647-57.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative differences in intestinal Faecalibacterium prausnitzii in obese Indian children. Br J Nutr. 2010;103:335-8.
- [CrossRef] [PubMed] [Google Scholar]
- Gut Microbiota in Type 2 diabetes individuals and correlation with monocyte chemoattractant protein1 and interferon gamma from patients attending a tertiary care centre in Chennai, India. Indian J Endocrinol Metab. 2016;20:523-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Gut microbial diversity assessment of Indian type-2-diabetics reveals alterations in eubacteria, archaea, and eukaryotes. Front Microbiol. 2017;8:214.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep. 2021;11:2738.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The gut microbial diversity of newly diagnosed diabetics but not of prediabetics is significantly different from that of healthy nondiabetics. mSystems. 2020;5:e00578-19.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trans-ethnic gut microbiota signatures of type 2 diabetes in Denmark and India. Genome Med. 2021;13:37.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Human gut microbes associated with systolic blood pressure. Int J Hypertens. 2022;2022:2923941.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Small intestinal bacterial overgrowth and toll-like receptor signaling in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2016;31:213-21.
- [CrossRef] [PubMed] [Google Scholar]
- High potency multistrain probiotic improves liver histology in non-alcoholic fatty liver disease (NAFLD): A randomised, double-blind, proof of concept study. BMJ Open Gastroenterol. 2019;6:e000315.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Real life diabetes prevention initiatives in India. Global health perspectives in prediabetes and diabetes prevention 2014:281-315.
- [Google Scholar]
- Consensus physical activity guidelines for Asian Indians. Diabetes Technol Therap. 2012;15:83-98.
- [CrossRef] [PubMed] [Google Scholar]
- Health promotion interventions in type 2 diabetes. Ann Ist Super Sanita. 2015;51:192-8.
- [CrossRef] [PubMed] [Google Scholar]
- ICMR guidelines for management of type 2 diabetes 2018. 2018.
- Impact of health education on knowledge, attitude, practices and glycemic control in type 2 diabetes mellitus. J Fam Med Prim care. 2019;8:261-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary prevention of diabetes: What can be done and how much can be prevented? Annu Rev Public Health. 2004;26:445-67.
- [CrossRef] [PubMed Central] [Google Scholar]
- 2022. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. Available from: https://dghs.gov.in/content/1363_3_NationalProgrammePrevention Control.aspx
- Diabetes care in public health facilities in India: A situational analysis using a mixed methods approach. Diabetes Metab Syndr Obes. 2019;12:1189-99.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Role of primary care physicians in diabetes care in India. Int J Sci Reports. 2020;6:235.
- [Google Scholar]
- 2021. Operational Guidelines for integration of Non-Alcoholic Fatty Liver Disease (NAFLD) with NPCDCS. Available from: https://main.mohfw.gov.in/newshighlights-42
- Circadian rhythms in the pathogenesis and treatment of fatty liver disease. Gastroenterology. 2020;158:1948-1966.e1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Perceived stress and non-alcoholic fatty liver disease in apparently healthy men and women. Sci Rep. 2020;10:38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effects of sleep quality on non-alcoholic fatty liver disease: A cross-sectional survey. BMJ Open. 2020;10:e039947.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Insomnia and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. J Postgrad Med. 2017;63:226-31.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Journal of Hepatology. 2016;64:1388-402.
- [CrossRef] [PubMed] [Google Scholar]
- BACKGROUND
- TERMS OF REFERENCE (TORS) FOR THE TASK FORCE
- METHODOLOGY
- CURRENT SITUATION OF OBESITY AND LIFESTYLE DISEASES IN INDIA
- Magnitude of obesity and lifestyle diseases in India
- Diabetes mellitus in India
- Hypertension in India
- Dyslipidemia in India
- Metabolic syndrome in India
- Non-alcoholic fatty liver disease (NAFLD) in India
- RISK FACTORS OBESITY AND LIFESTYLE DISEASES IN INDIA
- Diet and physical activity as risk factors for obesity in India
- Genetic factors in lifestyle diseases
- Other common risk factors for lifestyle diseases
- CURRENT STRATEGIES FOR MANAGEMENT OF OBESITY AND LIFESTYLE DISEASES IN INDIA
- Strategies at different levels of prevention
- Strategies for existing health-care delivery system
- Role of professionals in preventing lifestyle disorders
- KNOWLEDGE GAPS AND RECOMMENDATIONS FOR OBESITY AND LIFESTYLE DISEASES IN INDIA




