Translate this page into:
Role of Chest Radiographs during COVID-19 Pandemic
Address for correspondence Ashu Seith Bhalla, MD, MAMS, FICR, Department of Radiodiagnosis, All India Institute of Medical Sciences Ansari Nagar, New Delhi 110029, India (e-mail: ashubhalla1@yahoo.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Across the globe, computed tomography is the most widely used imaging modality mentioned in the published literature on the recent COVID-19 pandemic. However, in terms of availability, ease of use, and sanitization of the equipment; chest radiograph is a much more feasible option. However, interpretation of radiographs needs expertise to achieve appropriate diagnostic accuracy. This article will discuss its current role in diagnosis and severity assessment, as well as a systematic approach toward interpretation.
Keywords
CXR
radiograph
COVID-19
radiology
Introduction
The recent COVID-19 pandemic has initiated many practice-changing trends in modern medicine. On the imaging front, this disease has been extensively evaluated using computed tomography (CT) scans and less frequently, using chest radiographs. In this article, we shall discuss the role of chest X-ray (CXR) in the current COVID-19 pandemic, and provide detailed reporting about it in a systematic manner.
CT Scan versus CXR
While the superior diagnostic accuracy of CT in the detection and quantification of changes in lung parenchymal pathology is not debatable, there are numerous advantages of using CXR in the setting of the current pandemic. The obvious advantages of CXR includes its low-cost and availability. Also, portable units can be deployed in COVID-19 wards, intensive care units (ICUs) and COVID screening areas within the emergency rooms (ERs). Even more important in the context of the highly contagious organism is the fact that sanitization/disinfection procedures for portable X-ray units is far less cumbersome than those for CT scanners. Hence, the use of X-rays is associated with less risk of cross-infection compared with CT scans.1 As the number of patients affected by this pandemic grows, use of CXR as the primary imaging tool, with CT as a problem solving tool, seems an effective strategy.
For these reasons, while in the initial weeks of the pandemic in mainland China, the emphasis of imaging in COVID-19 pneumonia was on the use of CT scans, there has been an increasing reliance on CXRs across the world recently.2,3 Current evidence (based on published literature) on use of CXR in COVID pneumonia is listed in ►Table 1.
| Author | Place of origin | Duration of study | Study population | Sample size | CXR findings | CT comparison, if any |
|---|---|---|---|---|---|---|
| Wong et al5 | Hong Kong | January- March 2020 | COVID-19 positive (by RT-PCR) patients admitted across four hospitals | 64 patients (26 men, mean age 56.19 years) | Sensitivity 69% (compared with 91% of initial RT-PCR) Consolidation > GGO bilateral, peripheral, basal CXR severity peaked 10–12 D after symptom onset | Not all (28/64) CXR and CT imaging findings similar |
| Yoon et al6 | South Korea | January–February 9, 2020 | COVID-19 confirmed (by RT-PCR) cases from three hospitals in Seoul, South Korea | 9 patients (median age, 54 years; 4 men) | 33.3% showed parenchymal abnormality in CXR lower lobe predominant peripheral distribution Consolidation > GGO | Yes, in all similar findings |
| Chen et al7 | Wuhan, China | January 1–January 20, 2020 | COVID-19 confirmed (by RT- PCR) cases in Wuhan Jinyintan Hospital | 99 patients (average age 55·5 years [SD] 13·1); 67 men and 32 women | CXR abnormality in all 74 (75%): bilateral pneumonia, 14 (14%): multiple mottling and GGO, one (1%): pneumothorax. ARDS in 17 (17%) | Yes, in all bilateral consolidation > GGO |
| Ng et al8 | Shenzhen and Hong Kong | – | COVID-19 confirmed cases in Shenzhen and Hong Kong | 21 patients (mean age 56 years) | CXR done in five. CXR abnormality in 60% patients. Peripheral consolidation commonest | Yes, detection of GGO superior on CT |
| Lomoro et al9 | Italy | February 15–March 15, 2020 | Laboratory-confirmed COVID-19 cases hospitalized in Valduce Hospital (Como, Italy) | 58 patients (36 men, 22 women; age range, 18–98 years) | CXR done in 32/58. Consolidation was commonest finding (47%) > hazy increased opacity (37.5%) Bilateral distribution, lower lobe predominance | Yes, done in 42/58 Multifocal GGO with consolidation > GGO without consolidation > crazy paving pattern |
Abbreviations: ARDS, acute respiratory distress syndrome; CXR, chest X-ray; GGO, ground glass opacity; SD, standard deviation.
Role of CXR
The role of CXR in various scenarios is as follows:
COVID-19 Positive Patient (RT-PCR Positive)
A dedicated portable CXR unit should be placed in the COVID ward/ICU and bedside CXRs performed.
Personal protection of radiographers and sanitization of equipment should be performed as per society/institutional guidelines/standard operating protocols (SOPs)2,3
Asymptomatic RT-PCR positive patients need not get CXR done.
In symptomatic patients, periodic CXRs should be performed based on patient's clinical status. Daily CXRs are not warranted.
COVID-19 Suspects
CXRs are advocated in all patients presenting with SARI (severe acute respiratory infection). In influenza-like illness (ILI), decision can be made on case-to-case basis.
CXR should be performed if any two of the following are present4:
Fever (without any apparent nonrespiratory cause).
Shortness of breath.
Immunocompromised host.
Hypoxia (room air SpO2 < or equal to 94%).
Respiratory rate >/= 20/ minute.
CXR Findings
Radiographic Patterns
Based on published literature5-10 and institutional experience, we have observed the following CXR patterns in COVID-19 pneumonia. Several radiographic patterns of COVID pneumonia have been described, several of which are considered classical signs of the infection.
Pattern 1: Peripheral Airspace Opacities
This is a classical pattern of COVID-19 pneumonia, wherein airspace opacities are distributed along the periphery of the lung (►Fig. 1A). These opacities do not necessarily show a lower lobe predominance; in our experience, although there is, in fact, a relative sparing of the lung apices and costophrenic (CP) angles. This appearance is very similar to the “reverse batwing” appearance seen in chronic eosinophilic pneumonia or organizing pneumonia.

- (A-F). CXR patterns of COVID-19 pneumonia. (A) Pattern 1: Peripheral reverse bat-wing (arrows) (B) Pattern 2: Lower and midzones GGO/consolidation (asterisk) (C) Pattern 3: Peribronchial consolidation (arrows) (D) Pattern 4: Multifocal nonspecific distribution (E) Pattern 5: Nodular/ mass-like (asterisk) (F) Pattern 6: ARDS. ARDS, acute respiratory distress syndrome; CXR, chest X-ray.
Pattern 2: Bilateral Lower Zones Consolidation/Ground Glass Opacity
This is the most frequently reported pattern (►Fig. 1B) in COVID-19 pneumonia.6,8,10 Compared with CT, ground glass opacity (GGO) can be difficult to appreciate on CXR, and hence the importance of viewing the CXR in optimal conditions. If superimposed septal thickening develops, GGO becomes easier to detect on CXR.
Pattern 3: Peribronchial Consolidation
Another pattern which has been reported on CT and observed by the authors on CXR is the peribronchial distribution of consolidation (►Fig. 1C), wherein dominant findings are present in the lower or midzones on both sides
Pattern 4: Multifocal Airspace Opacities/Consolidation/GGO
This appearance is similar to pattern 2, except that the opacities do not show the bilateral, lower lobe distribution (►Fig. 1D). This appearance is frequently encountered in viral pneumonia; unlike unilobar consolidation, which is more frequent in bacterial community-acquired pneumonia (CAP). The presence of areas of breakdown suggests a bacterial etiology.
Pattern 5: Large Nodule or “Mass-Like” Opacities (Ball Pattern)
Large nodules/localized rounded consolidation has been reported as an uncommon/rare finding in a single case.11 We have, however, encountered this pattern in several COVID-19 pneumonia patients, which we refer to as “ball-pattern” (►Fig. 1E). These lesions do not always show a lower lobe predilection. The large nodule may be a solitary lesion or be present in conjunction with other patterns.
Pattern 6: Diffuse Mid- and Lower Zones Consolidation/Airspace Opacities
This pattern is seen in more severe forms of the disease, and corresponds to a clinical picture of acute respiratory distress syndrome (ARDS) (►Fig. 1F). Once these changes develop, the appearance is nonspecific and etiology has to be surmised on the current pandemic background, as this pattern can be seen with several inflammatory/infectious/multisystem processes.
Pattern 7: Uncommon/Rare Patterns
Some additional rare lung changes include cavitation, and upper and middle lobe partial collapse, which is likely due to mucus plugs.
It should also be kept in mind that in a given patient more than one pattern can coexist.
Complications
Infrequent complications include pleural effusion, pneumothorax, pneumomediastinum, and subcutaneous emphysema. Air leaks are rare, as cavitation is rarely encountered in COVID-19 pneumonia12, and are more likely to be seen as a complication of barotrauma following ventilation.
CXR Reporting
The labeling of a CXR in four different categories (normal, classic/ probable, indeterminate, or non-COVID) should be adopted to convey a risk-stratified imaging information to the physician. Although there is no evidence on CXR for the categorization, this can be adopted as an extrapolation of CT-based risk stratification systems available with various society guidelines. In our institute, we adopt the following criteria (adapted from reference13):
Normal: CXR normal; COVID-19 not excluded.
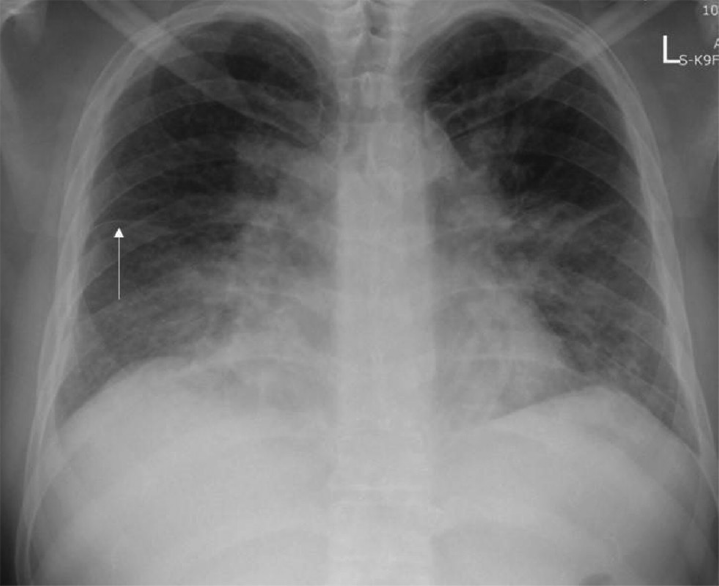
Classic/probable COVID-19: Lower lobe predominant and peripheral predominant; multiple, bilateral, areas of GGOs (►Fig. 2).

- Definite COVID-19 pneumonia on CXR. Typical peripheral bilateral consolidation. CXR, chest X-ray.
Indeterminate: Does not fit into classic/non-COVID pattern (►Fig. 3).
- Indeterminate for COVID-19 pneumonia on CXR. Bilateral perihilar consolidation and GGO, with lamellar pleural effusion and fissural thickening (arrow) on right side. CXR, chest X-ray; GGO, ground glass opacity.
Non-COVID pattern: Pneumothorax, lobar consolidation, pleural effusion, and pulmonary edema (►Fig. 4).

- (A-C) Examples of non-COVID patterns on CXR. (A) Left lower lobe collapse (asterisk) with bilateral pleural effusion (E) (B) Loculated pneumothorax (arrows), pneumomediastinum (asterisk), subcutaneous emphysema (block arrow) (C) Bilateral mid- and lower zones consolidation (asterisk) with pleural effusion (E).
Sensitivity OF CXR
The reported sensitivity of CXR in diagnosis of COVID-19 ranges from 33.3 to 69% (►Table 1). This sensitivity is lower than that of CT scans (up to 98%),14,15 and that of initial RT-PCR. It has, however, been shown that CXR may be abnormal in some patients (reported in 9% cases by Wong et al5), even when initial RT-PCR is negative. Hence, in view of the various advantages of CXR listed earlier, it is likely to be a useful tool during the pandemic.
A critical point while reporting the CXR is that it should be viewed in optimal viewing conditions, preferably on a picture archiving and communication system (PACS) with appropriate monitor by a qualified radiologist. Interpretation of the same in suboptimal conditions or by non-expert personnel will result in missing of subtle findings and misinterpretation and hence lower diagnostic accuracy. Also, non-COVID diagnosis should not be labeled as COVID-19 related due to the pandemic. It is hence suggested that understandably the CXR will be interpreted in the ER by the treating physician; however, subsequently an additional formal radiology report should always be sought and consulted.
CXR Scoring System
Recently, CXR is being used more frequently than CT to monitor the “day-to day” progression of the pulmonary involvement of SARS-CoV-2. This was first emphasized in an Italian study16 and its role emphasized in the setting of a rising number of SARS CoV-2 cases and resultant ICU admissions. If CXR is to be used as a tool for monitoring disease progression, it is important to express the extent of involvement quantitatively. To the best of our knowledge, only two CXR scoring systems have been described for COVID-19 pneumonia in English literature so far, and we are employing a third scoring system at our institute, which is under validation.
The first scoring system employed by a S. Korea6 based group considers the entire lung together, and it is mainly based in the expected pattern of progression of the pneumonia (►Table 2). In the second scoring system employed and validated by Italian investigators,16 each lung was divided into three zones, with the maximum score for each zone being 3 and the total score being 18. The description within the zones was based predominantly on the pattern within the zone, whether interstitial, alveolar or combined, with alveolar opacities representing more severe disease.
| Author | Scoring system | Based on | Validated |
|---|---|---|---|
| Yoon et al6 | 5-point scale 1: normal 2: patchy atelectasis and/or hyperinflation and/or bronchial wall thickening 3: focal alveolar consolidation involving no more than one segment or one lobe 4: multifocal consolidation 5: diffuse alveolar consolidation |
Score by Taylor et al in 201517 On hospitalized patients with acute respiratory infections |
No |
| Borghesi et al16 | Both lungs divided in three zones each (upper, middle, lower). Each zone is given a separate score 0–3 (max score: 18) 0: normal 1: interstitial infiltrates 2: Mixed interstitial and alveolar infiltrates (predominantly interstitial) 3: Mixed interstitial and alveolar infiltrates (predominantly alveolar) |
No prior study | Yes Validated with outcome of 100 admitted SARS-CoV-2 patients16 The CXR scoring interobserver agreement was very good (kw, 0.82; 95% CI, 0.79–0.86). CXR score was significantly higher in patients who died than those discharged from the hospital (p ≤ 0.002) |
| Our institute | Each lung divided in to three zones. Within each zone, a score 0–4 is given. (max score: 24) 0: normal 1: 1–25% of area involved 2: up to 50% of area involved 3: up to 75% of area involved 4: >75% of area involved |
No prior study | Under validation |
Abbreviation: CXR, chest X-ray.
In the scoring system employed at our institute, the lungs are divided into three zones each (similar to Borghes et al), but the score is based on the percentage of lung involved within the zone rather than the pattern (►Figs. 5 and 6). The maximum score for each zone is 4 and hence the total score is 24. This score is currently under validation at our institute.

- Severity score employed by the authors (4). Each zone is given a score of 0 to 4 depending on area of involvement 0: normal. 1: 1–25% of area involved. 2: up to 50% of area involved 3: up to 75% of area involved 4: > 75% of area involved maximum score: 24 (6 × 4).
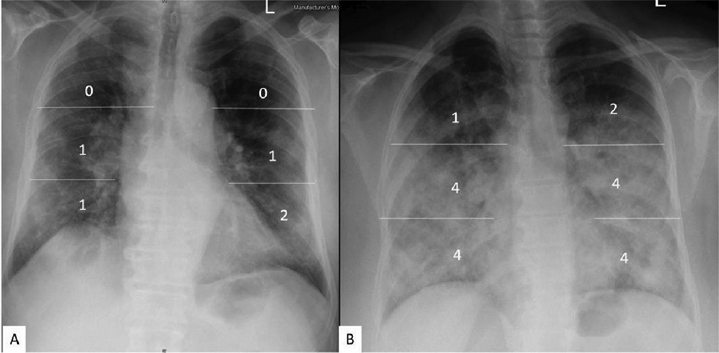
- CXR severity score: Examples: (A) Mild disease: severity score 5/24 (B) Severe disease: severity score 19/24. CXR, chest X-ray.
CXR and Disease Monitoring
Worsening of radiographic changes are generally concordant with clinical imaging. The peak CXR changes have been reported between day 10 to 12(from infection onset). While some studies have shown that radiological and virological recovery parallel each other,5 discordant timelines have been demonstrated by others.14
Structured Reporting
The authors propose the use of a structured reporting format while reporting CXR in suspected/proven COVID-19 cases. Whereas CO-RADS, a standardized reporting tool in CT of COVID-19 patients,18 is already in use, similar tools in CXR are not widely used. Various societies have proposed structured reporting templates for CXR.4,13►Fig. 7 describes the structured reporting format used at our institute which was proposed by Indian College of Radiology and Imaging.4
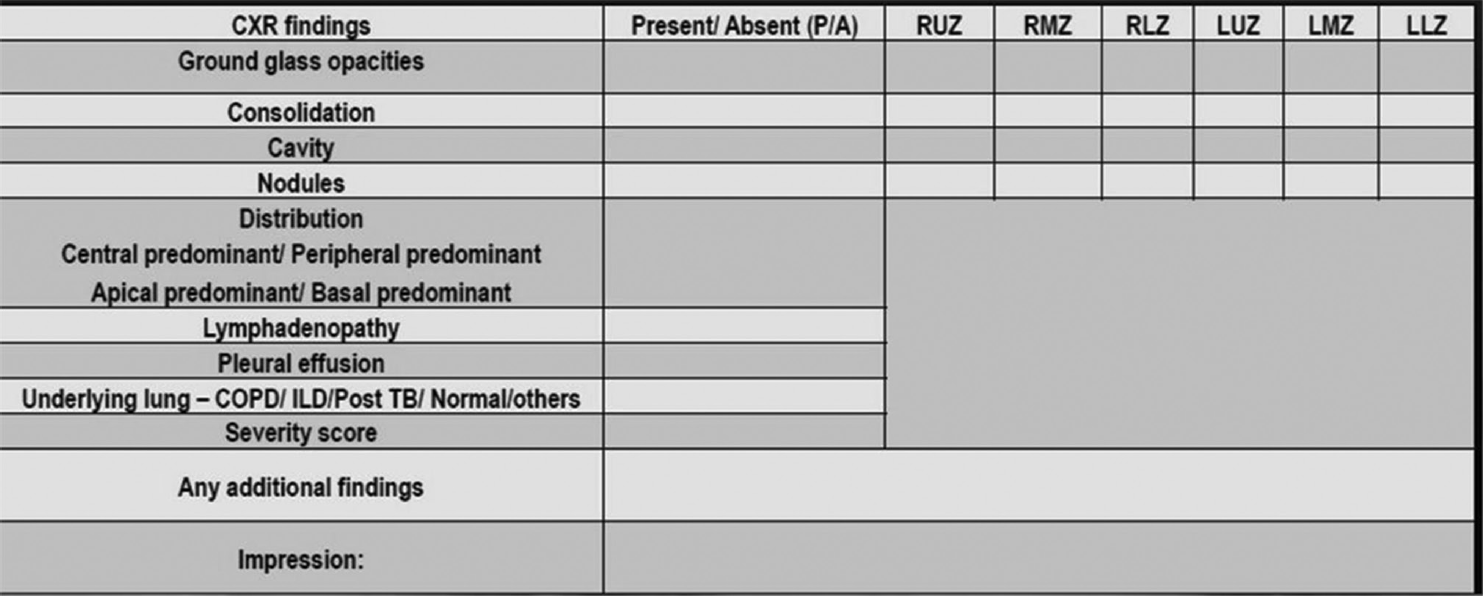
- Structured reporting format suggested by the authors.4
Conclusion
Hence, CXR is a valuable tool in better management of patients during the COVID-19 pandemic. Despite its lower sensitivity compared with CT scans, its myriad inherent advantages make it indispensable. Further addition of chest ultrasound to the CXR in ICU settings will immensely reduce the need for CT scans.
Conflict of Interest
None declared.
References
- ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection | American College of Radiology. Available at: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. (accessed )
- [Google Scholar]
- Lessons from the Frontline of the Covid-19 outbreak - The BMJ. Available at: https://blogs.bmj.com/bmj/2020/03/20/lessons-from-the-frontline-of-the-covid-19-outbreak/?utm_campaign=shareaholic&utm_medium=twitter&utm_source=socialnetwork. (accessed )
- [Google Scholar]
- Available at: https://healthcare-ineurope.com/en/news/imaging-the-coronavirus-disease-covid-19.html. (accessed )
- Imaging Recommendation by Indian Radiological and Imaging Association (IRIA) and Indian College of Radiology and Imaging (ICRI) for COVID-19. Available at: https://iria.org.in/. (accessed )
- [Google Scholar]
- Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019;x:201160.
- [Google Scholar]
- Chest radiographic and CT Findings of the 2019 novel Coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21(04):494-500.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513.
- [Google Scholar]
- Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol. Cardiothorac. Imaging. 2020;2:e200034.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7:100231.
- [CrossRef] [PubMed] [Google Scholar]
- CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295(01):202-207.
- [CrossRef] [PubMed] [Google Scholar]
- Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review. Clin Imaging. 2020;64:35-42.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. Am J Roentgenol. 2020;14:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Thoracic Imaging in COVID-19 Infection. Guidance for the Reporting Radiologist British Society of Thoracic Imaging Version 2. Available at: https:/bsti.org.uk/. (accessed )
- [Google Scholar]
- Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;200642(February):200642.
- [Google Scholar]
- Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;200432:200432.
- [Google Scholar]
- COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med (Torino). 2020;125(05):509-513.
- [CrossRef] [PubMed] [Google Scholar]
- SHIVERS Investigation Team . A chest radiograph scoring system in patients with severe acute respiratory infection: a validation study. BMC Med Imaging. 2015;15:61.
- [CrossRef] [PubMed] [Google Scholar]
- “COVID-19 Standardized Reporting” Working Group of the Dutch Radiological Society . CO-RADS - A categorical CT assessment scheme for patients with suspected COVID-19: definition and evaluation. Radiology 2020 DOI: 10.1148/radiol.2020201473.
- [CrossRef] [PubMed] [Google Scholar]





