Translate this page into:
Spectrum of bacterial isolates and their antibiogram in intensive care unit (ICU) of tertiary care hospital as a part of hospital acquired infection (HAI) surveillance
*Corresponding author: Tapan Majumdar, Department of Microbiology, Agartala Government Medical College & GBP Hospital, Tripura, India. drtapan1@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Deb J, Debnath S, Bhattacharya S, Majumdar T. Spectrum of bacterial isolates and their antibiogram in intensive care unit (ICU) of tertiary care hospital as a part of hospital acquired infection (HAI) surveillance. Ann Natl Acad Med Sci (India). 2024;60:190-6. doi: 10.25259/ANAMS-2023-3-11-(869)
Abstract
Objectives
The introduction of the study discusses the prevalence of Urinary Tract Infections (UTIs) as a common hospital-acquired infection worldwide. The specific goals of the study were to isolate and identify the organisms causing UTIs, and determine their antimicrobial sensitivity patterns.
Material and Methods
A total of 150 consecutive urine samples were collected over a 24 month period from selected surveillance units Medical-Surgical ICU (MICU) Respiratory ICU (RICU) Pediatric ICU (PICU). Microbiological culture, subsequent bacterial identification and antimicrobial susceptibility test were performed for the positive samples. The prevalence of the causative agents was analyzed according to the patient’s gender and age group.
Results
A total of 45 uropathogens were isolated, with Enterococcus spp. being the most common at 33.3%. The study found that Nitrofurantoin antibiotic had the highest sensitivity at 77% against Enterococcus spp. The study also found that nosocomial infections lengthened hospital and intensive care unit stays, and during the surveillance period eight patients expired, who were infected by Enterococcus spp., Klebsiella pneumoniae, Enterobacter spp. and Klebsiella spp.
Conclusion
The conclusion section of the study highlights that the study documented the pathogenic effect of Enterococcus spp., which was responsible for the majority of infections. This study may be useful for future studies to assess the genetic profile of the MDR gene of isolated microorganisms and to early assess the methods for detecting pathogenic organisms in clinical samples in order to save lives in critical care units. The study also suggests that Nitrofurantoin antibiotic was found to be the most effective against urinary tract isolates of Enterococcus spp.
Keywords
UTIs
CAUTI and Non- CAUTI
Antibiotics
MDR
Nosocomial infection
HAI
INTRODUCTION
A nosocomial-acquired sickness called a hospital-acquired infection (HAI) is typically dormant or developing when the patient is admitted. These infections typically start to appear >2 calendar days after being admitted to the hospital, and Centers for Disease Control and Prevention organizations like the National Healthcare Safety Network continuously monitor the infection rate.1 Infections acquired in a hospital or nosocomial settings are estimated to affect more than 1.4 million people worldwide and it is estimated that 2 million cases of HAI occur each year, and 80,000 people die from this type of infection.2 In the United States and Europe, the most prevalent urinary tract infection caused by a catheter affects more than 1 million people each year.3 One of the most frequent device-associated infections that patients admitted to the ICU get is catheter-associated urinary tract infection (CAUTI). One of the most often reports revealed that device-associated infections among patients admitted to the ICU with urinary tract infection brought on by a catheter and around 75% of hospitalized patients have a urinary catheter inserted, which creates challenges for CAUTI management and prevention. They continue to rank second in importance among health care associated infections (HCAIs) in the intensive care unit (ICU), where 95 percent of urinary infections are catheter-associated. When CAUTI is not recognized and is handled incorrectly, there is an increased risk of complications, which lowers the effectiveness of healthcare delivery and to avoid complications such as nephritis, acute urethritis, septicemia, and urosepsis, prompt action is required.4 The signs and symptoms exist as frequent urination, burning, or pain while urinating or lower abdomen pain, among signs of kidney infection are fever, chills, backache on one side or in the lower back, and nausea.4 Other elements, such as previous urinary tract infections (UTIs), sexual behavior, and modifications to the vaginal flora or bacteria, might also raise UTI risk. For instance, these bacterial alterations can be brought about by periods or urinary tract structural problems, for example, enlargement of the prostate and children who are potty training may exhibit poor cleanliness.5 According to reports by Rezai et al.6 this amount is too high and double what it is in other nations. An extended hospital stay and overall hospital costs are increased brought on by this infection and antibiotic-resistant pathogen infections typically have greater fatality rates.6 Aman et al.7 reported that the risk of contracting device-associated nosocomial infections are highest in an intensive care environment. The frequent use of medical equipment, increasing device days, length of hospital stays, and severity of patient disease are all contributing factors to the high infection prevalence in ICUs. Our study found a startling rise in multi-drug resistance (MDR) among device associated nosocomial infections (DANI) patients, indicating the urgent need to manage this MDR. This study’s updated guideline aims to address Urinary tract infection prevention for patients receiving short or long-term urinary catheterization in any setting and catheterization, external catheters, and suprapubic catheters are examined for their efficacy.7
Therefore, the specific goals of this present research work were; i) To study the isolate organisms in selected surveillance unit according to the age group of the patients, ii) To determine the antimicrobial sensitivity pattern of the isolate organisms, iii) To determine the relation between the hospital stay and the type of bacteria causing nosocomial infection.
MATERIAL AND METHODS
The CAUTI and Non-CAUTI infection surveillance were conducted in the Medical-Surgical ICU (MICU), Respiratory ICU (RICU), Pediatric ICU (PICU), in the Agartala Government Medical College and Hospital (AGMC and GBP Hospital, Agartala, Tripura, India) from July 2020 to June 2022. The institutional ethical committee granted approval for the surveillance to continue in those ICUs (IEC Ref. No. 3935). In accordance with the CDC’s (Center for Disease Control) guidelines, the surveillance was carried out.
Patient selection
Patients who had completed >2 days of with or without urine catheterization following ICU admission, and provided written informed consent were included in the study. Patients who had positive urine cultures before catheterization and had been catheterized for less than two calendar days were not included in the study.8
Sample collection
The CDC recommended that the microbiological samples were taken from patients who had UTIs and had at least one of the following signs or symptoms: fever (>38.0°C) in the event of catheter-associated urinary tract infection (CAUTI) at any age. Urinary urgency, frequency, suprapubic tenderness, and dysuria are all symptoms of a urinary tract infection. Additionally, Non-Catheter-associated Urinary Tract Infection (Non-CAUTI) in patients of any age who have a fever (higher than 38°C), Urinary frequency, urgency, or dysuria, suprapubic soreness, cerebral vascular accident (CVA), or tenderness.9
Sample collection from CAUTI patients
Get the necessary supplies and wear personal protective equipment when collecting samples from catheterized patients. Make sure the catheter tubing does not contain urine before collecting a sample from a sampling port. Apply the clamp 3 inches below the level of the sampling port and clean the sample port with a prep wipe allowed to dry it properly. Aspirate at least 10 ml of urine and disconnect the syringe put the specimen into a sterile container and, properly label it and released the clamp from the catheter tube.10
Sample collection from non-CAUTI patients
Prior to performing Midstream urine, make sure your hands and genitalia must be clean. The vaginal entrance should be held open by women. It is recommended for males to retract their foreskin. After that, discard a few drops of urine and the rest were collected and placed in a sterile container. Samples were collected in a screw cap sterile container. The infection will increase if any contact with the container while touching the patient’s genitalia and reattach the container’s lid.11
Identification of microbes
For the semi quantitative approach, routine urine cultures were plated using calibrated loops and this approach has been benefited of providing information on the CFU/ml count as well as isolated colonies for susceptibility testing and identification.12 For normal urine culture, a mixture of blood agar (BA) and MacConkey agar, cystine lactose electrolyte deficient (CLED) was applied because it promotes the growth of all potentially harmful urinary pathogens as well as a number of contaminants such diphtherias, lactobacilli, and micrococcus. Additionally, it distinguishes between colonies that ferment lactose and those that do not, and it prevents the growth of Proteus species from swarming. With all of these advantages, CLED agar may be utilized as the only medium, lowering costs without sacrificing quality.13
Bacterial identification
Pure culture isolates of the bacterial pathogen were preliminarily characterized by colony morphology and Gram staining technique along with some standard biochemical tests through which bacterial isolates were identified up to the species level.
Antimicrobial susceptibility testing
Antimicrobial susceptibility test was carried out by standardized Kirby Bauer disc diffusion method as per the Clinical Laboratory Standards Institute (CLSI) guidelines on Muller Hinton agar medium. The bacterial suspension of each isolate was prepared in 0.5 ml of nutrient broth medium and the turbidity was adjusted to match that of 0.5 McFarland standards. A sterile swab was dipped into the suspension and then the swab was applied to the center of the Muller Hinton agar plate and evenly spread on the medium. Antibiotic discs were placed onto Muller Hinton agar seeded with each isolate and were incubated for 24 hours at 35–37˚C. Inhibition zone (IZ) diameter was measured using a caliper and interpreted according to the CLSI guideline as susceptible (S), intermediate (I), or resistant (R).
Antibiotics used
In this study different antibiotic disc were used at various concentrations namely, Gentamicin 10 μg, Amikacin 10 μg, Cefotaxime 30 μg, Ceftazidime 30 μg Ceftriaxone 30 μg, tetracyclines 30 μg, trimethoprim- sulfamethoxazole 25 μg, oxacillin 30 μg, penicillin10μg, Ampicillin 10 μg, vancomycin 30 μg, Imipenem 10μg, Meropenem 10 μg and ciprofloxacin 5 μg for the determination of antibiotic property.4
Statistical analysis
All the calculations were done with the help of PAST (Alaeontological STatistics) software version 2.17c. The experimental results were analyzed using Two-Way ANOVA (analysis of variance) following Tukey’s honestly significant difference (HSD) test were conducted to find out the significance among the different parameters of studied patients at p<0.05.
RESULTS
The prevention of ICU-acquired infections requires a thorough understanding of infection rates, sources, pathogens, and the risk factors. The incidence of nosocomial infections varies according to the setting, i.e., the type of hospital or ICU, the patient population, the precise definition and surveillance techniques. This study revealed that the main causative organism for CAUTI and non-CAUTI infections varied by age group and gender.
During the study period from July 2020 to June 2022, 150 patients with hospital-acquired urinary tract infections were identified in the surveillance critical care unit. Of these, 82.2% (n = 37 out of 45) were identified as Catheter-Associated Urinary Tract Infections (CAUTIs) and 17.8% (n = 8 out of 45) as non-CAUTIs. Of the 150 samples tested and 45 tested samples isolated as positive infection. Among the 45 positive isolates, 35 were from the Medical-Surgical ICU (MICU), 5 were from the Pediatric ICU (PICU), and the remaining 5 were from the Respiratory ICU (RICU).
Outcomes of this study revealed that the most affected infection caused by CAUTI which was highly observed in the male age group it ranges from 20 years to 40 years, whereas in females it ranges from 41 years to 60 years [Figure 1]. It was also observed that males over 60 years of age becoming mostly affected age group. In the case of the RICU, the age group between 18 years to 40 years and over 60 years of age was mainly affected by CAUTI. On the other hand, infection caused by Non-CAUTI was highest at the age range of 18 years to 40 years in females and males over 60 years were mostly affected. The age ranges and relative rates of CAUTI and Non-CAUTI across patients’ sexes indicated a significant influence across age ranges and sexes (F = 3.91, p<0.0002 and F = 13.41, p<0.006).
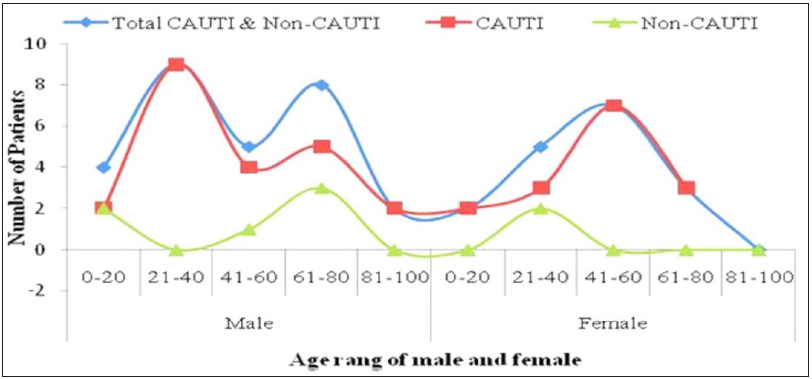
- Shown the different age group of people with and without catheter device. CAUTI: Catheter-associated urinary tract infection.
Isolation of bacteria
As a result of the processed samples 45 microbial pathogens were identified out of 150 suspected UTI infections. Among the bacteria isolated, Enterococcus spp. was found. To determine the significant effect of the isolated organisms on patients, a two-way analysis of variance (ANOVA) was applied. If a significant effect was found in at least one sample at a 5% level of significance (i.e., p<0.05), a Tukey HSD test was then conducted to identify the most significant effects of the isolated organisms in relation to the number of patients.
Among the total bacterial isolates, Enterococcus spp. accounted for the highest percentage at 33.3%, followed by Escherichia coli (29%), Staphylococcus aureus (11.1%), Klebsiella pneumoniae (8.89%), Acinetobacter spp. (2.22%), Citrobacter freundii (2.22%), and Enterococcus faecalis (2.22%). In case of CAUTI, Enterococcus spp. was the most common microbial pathogen, accounting for 32.4% of the total isolates, followed by Escherichia coli at 29.7%, Staphylococcus aureus, and Enterobacter spp. Klebsiella pneumoniae was 8.11%, Klebsiella spp. 5.41%, Acinetobacter spp, Citrobacter freundii and Enterococcus faecalis were 2.7% of total isolates. For Non-CAUTI infections, Enterococcus spp. was isolated at 37.5% from total isolates, followed by Staphylococcus aureus and Escherichia coli at 25%, and Klebsiella pneumoniae at 12.50%.
There were more cases of CAUTI in male patients than in female patients in the intensive care unit. Different age ranges and sexes of patients had significantly different relative frequencies of CAUTI and Non-CAUTI. Males between the ages of 18 to 40 and females between the ages of 41 to 60 were most likely to catch CAUTI infections in MICUs, while Non-CAUTI infections affected males over the age of 60. The age ranges and relative frequencies of CAUTI and Non-CAUTI infections in HAI patients significantly differ among the different age group of patients (F = 39, p<0.0002, and F = 13.41, p<0.006).
Antimicrobial sensitivity pattern
In order to understand the impact of drug sensitivity patterns on various isolated microorganisms from patients in the surveillance unit, a two-way analysis of variance (ANOVA) was conducted. The majority of the experimental sets displayed a significant effect at a p<0.05 level.
The present study also evaluated the drug sensitivity patterns of the isolated microorganisms [Figure 2] and it was recorded that Enterococcus spp. was found to be the most superior pathogen causing infections. Nitrofurantoin was found to be 77% sensitive in Enterococcus spp. Isolated from urine samples, followed by Doxycycline at 66.6% and Amoxy/clav at 50% sensitivity. Cefixime and Ceftriaxone were found to have 100% resistance to Enterococcus spp., followed by Ciprofloxacin at 66.67%. Levofloxacin was 75% sensitive and Amikacin was 66.67% sensitive to Escherichia coli, while Piperacillin/Tazobactum and Ciprofloxacin (50%) had the lowest sensitivity. Staphylococcus aureus was completely susceptible to Nitrofurantoin and completely resistant to Gentamycin. Amikacin, Meropenem, and Ceftazidime had showed sensitivity rates of 75%, 58.33%, and 66.67%, respectively, against Klebsiella pneumoniae. Enterobacter spp. was found to be highly susceptible (100%) to Nitrofurantoin and Cefoxitin, followed by Doxycycline at 66.6%. For Acinetobacter spp. Isolated from urine samples showed the highest sensitivity of 100% against Colistin and Minocycline, while Imipenem showed 70% resistant. Piperacillin/Tazobactum and Imipenem were 100% susceptible to Citrobacter freundii and nitrofurantoin, followed by Amoxy/clav and Levofloxacin, which was 100% resistant. Ciprofloxacin and High Sensitive Gentamycin were 100% resistant to Enterococcus faecalis, which was identified from urine samples.
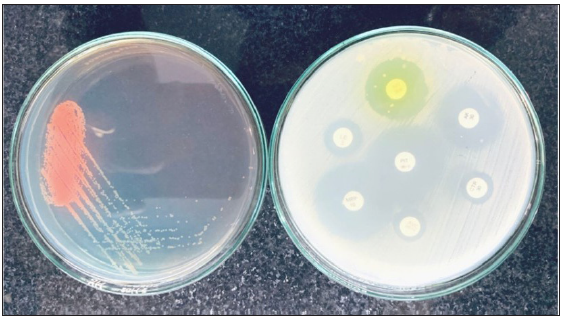
- Urine culture and sensitivity test.
Present findings revealed that a total of 8 patients had died from CAUTI infections, out of this 8 patients 7 patients were male and 1 female. The MICU had the most deaths compared to the PICU and RICU. The present research also identified Enterococcus spp. was the most commonly isolated organism from the unit MICU and accounted that 50% of cases, whereas by Klebsiella pneumoniae at 25% as well as Enterobacter spp. and Klebsiella spp. also accounted as 13% and 12% of cases, respectively. Despite recent shifts in pathogen patterns towards gram-positive bacteria, our study showed that they continue to play a significant role in nosocomial infections in the ICU. The present investigation revealed that gram-positive bacteria were the most frequently identified species and closely followed by Enterococcus spp.
This research work also documented that the duration of stay in the unit is the main factor affected by HAI organisms. In comparison to the date of the event and final outcome of the patients were already affected by the pathogens in the ward or unit before being transferred to the surveillance unit (ICU). According to the definition of nosocomial infection, the patient must be admitted to the hospital and must have completed 48 hours of hospital days. During these days, the maximum number of patients require life-saving devices during treatment. This research revealed that the majority of patients were affected by their individual units after admission. This might be due to a lack of sufficient understanding, as well as correct device care and handling (Interval of 95% Confidence: 7.89–16.07%) [Figure 3].
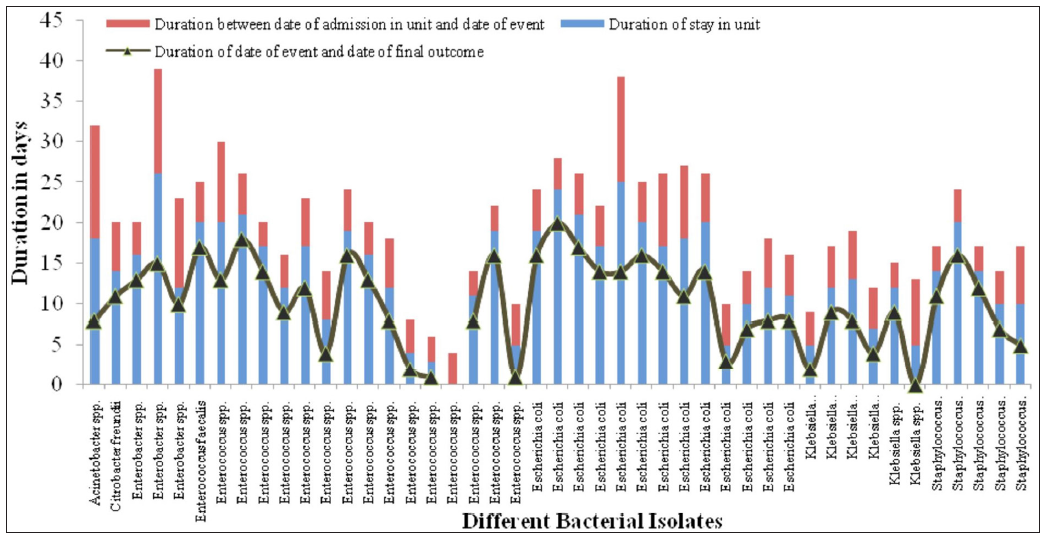
- Different duration in days against various bacterial infections.
DISCUSSION
The prevention of HAIs is a crucial cause because as it requires a comprehensive understanding of the underlying causes, including the rate of infections per month, sources of infection, types of pathogens and risk factors that facilitate the growth of pathogenic organisms. The aim of this study is to identify the causative organisms responsible for CAUTI and Non-CAUTI infections in the ICUs of a tertiary care hospital located in the state of Tripura, India. The number of patients identified with hospital-acquired infections, the proportion of CAUTIs and non-CAUTIs, the number of samples tested, and the number of samples provided by different ICUs. Additionally, the sentence also informs us of an accompanying figure that shows the age distribution of a few surveillance units.
Between July 2020 to June 2022, 150 hospital-acquired illness patients were identified in the selected surveillance units. A total of 45 samples were positive out of 150 samples. During this study period, 82.2% CAUTIs and 17.8% of non-CAUTIs were identified. Present findings showed that the distribution of age of selected surveillance units was highest in MICU. The findings of Saleem et al.14 documented that a total of 1078 patients were admitted to the hospital ICU, out of which healthcare-associated infection was reported in 316 patients and CAUTI was reported only in 70 patients (22.15%), which showed slight dissimilarity with our findings. Our findings were also comparable to the prevalence rate of other research work such as H Bizuayehu et al.4
Findings of Magliano et al.15 and Kiffer et al.16 were comparable to our present research findings, in terms of the patient population (both males and females of any age), the number of isolates, and selected age groups. Present findings revealed that more male patients had CAUTI as compared to female patients,14 whereas the most effective age ranges were 21-40 years in males and 41-60 years in females.
Isolation of bacteria
From the isolated samples, multiple Enterococcus species were isolated and accounted at 33.3%, followed by Acinetobacter spp. and Escherichia coli (29%), Klebsiella pneumonia (8.89%), and Staphylococcus aureus (11.1%), in that order. Additionally, 2.22 percent of Enterococcus faecalis and Citrobacter freundii were recorded but findings of Rezai et al.6 observed that Escherichia coli was the main agent for urinary infection (34.9%), followed by Klebsiella (15.3%), Pseudomonas aeruginosa (9.5%), and miscellaneous (40.3%). Present findings showed similarity with the findings of Magliano et al.,15 where Escherichia coli recorded as 67.6% of all isolates, followed by Klebsiella pneumoniae (8.8%), Enterococcus faecalis (6.3%), Proteus mirabilis (5.2%), and Pseudomonas aeruginosa (2.5%). The results of the current study shows that the Enterococcus spp. microbial pathogen contributed 33.0% of the total isolates in catheter-associated urinary tract infection (CAUTI), followed by Escherichia coli (29.0%), Staphylococcus aureus (11%), Enterobacter spp. (7%), Klebsiella pneumonia were 9.0%, Klebsiella spp. 5.0%, and the least percentage was observed in Acinetobacter spp. In terms of non-CAUTI infections, Enterococcus spp. was the most common isolate, accounting for 37.5% of all isolates, followed by Staphylococcus aureus and Escherichia coli at 25% and Klebsiella pneumonia at 12.50%. Similar findings was observed by Saleem et al.,14 where that Klebsiella pneumoniae (20%) was the predominant isolate, whereas Serratia (3%) and Providencia (3%) species were the least common isolates. Present observation revealed that the dominant isolate were Enterococcus sp. (50%) and Klebsiella pneumoniae (25%). Samples of E. coli isolated from patients were highly resistant to third-generation cephalosporin and aminoglycosides.
This research revealed that a total of 8 patients had passed due to CAUTI infection and there were 7 male patients and 1 female patient, additionally, it was also observed that few patients were passed away in the PICU, RICU and highest in the MICU unit. Furthermore, it was shown that Enterococcus spp. (50%) from the MICU, followed by Klebsiella pneumonia (25%), Enterobacter spp. (13%), and Klebsiella spp. (12%), were the most common isolates from the expired patient. Despite changes in the pathogen pattern in recent years toward Gram-positive bacterial infections and, they were consistently exist. The majority of research claims that Gram-negative bacteria are to blame for more than half of the nosocomial infections that occur in the ICU. Gram-positive bacteria were the most frequently identified species in the present investigation.
Antimicrobial sensitivity
In this study, the drug sensitivity patterns of isolated microorganisms from UTI patients were documented and found that Enterococcus spp showed 100% resistance to cefixime and ceftriaxone and 66% resistance to ciprofloxacin. Levofloxacin 75% and Amikacin. 66.67% were shown to have the highest sensitivity against Escherichia coli, while Piperacillin/Tazobactum and Ciprofloxacin (50%) showed the lowest sensitivity. It was also observed that Staphylococcus aureus was entirely susceptible to nitrofurantoin but completely resistant to Gentamycin. As well as Amikacin, Meropenem, and Ceftazidime showed sensitivity rates of 75%, 58.33%, and. 66.67%, respectively, against isolated Klebsiella pneumonia. Enterobacter spp. were showed highly susceptible to Doxycycline at 66.67% and highly resistant to Nitrofurantoin and Cefoxitin(100%). Isolated Acinetobacter spp. showed 100% sensitivity against Colistin and Minocycline. Piperacillin/Tazobactum and Imipenem was 100% susceptible to Citrobacter freundii. Ciprofloxacin and High Sensitive Gentamycin showed 100% resistance to Enterococcus faecalis, which was isolated and identified from the urine sample. This type of research was performed by various scientists throughout the world and results were comparatively varied from the findings of each other researchers.4,14 Aman et al.7 observed that Acinetobacter baumannii and Citrobacter species were the most common multidrug-resistant gram-negative pathogens responsible for Device associated nosocomial infection (DANI). According to Dasgupta et al.,17 K. pneumoniae (62.07%) was the most frequently discovered dominant organism in urinary tract infections, however, current data suggested that Enterococcus spp. (33%), caused the most number of urinary tract infections.
In this study, we discovered that the length of stay (days) in the unit is the most impacted by HAI organisms, in contrast to the date of the incident and the date of ultimate conclusion. Our findings revealed the maximum number of patients affected from their respective units after admission due to a lack of proper care and the maintained the device. Dasgupta et al.,17 documented that 11.98% of patients had nosocomial infections. (Interval of 95% Confidence: 7.89–16.07%) and finding revealed that the nosocomial infection statistically lengthened hospital and intensive care unit stays, but no deaths, and where is our findings showed similarity accept the death of patients at MICU, RICU and PICU.
Based on the results of the present study, we observed that the duration of stay in the unit is the main factor affected by Healthcare-Associated Infections (HAI) organisms. We found that the patients were already affected by the unit before being transferred to the surveillance unit, which highlights the importance of early identification and management of HAIs.
CONCLUSION
A high-risk setting for UTIs is an intensive care unit. The frequent use of medical devices, the duration of hospitalization, and the severity of the patient’s disease are only a few of the numerous variables that contribute to the high infection frequency in ICUs. The need to lower MDR in UTI patients is critical. Males were shown to be more likely than females to have a CAUTI infection in MICUs, whereas females aged 41 to 60 years were found to be more susceptible to non-CAUTI infections. It would be best to avoid inserting unnecessary catheters in order to reduce morbidity and length of hospital stay. If a Foley catheter is required, the aseptic procedure must be applied. The procedure will be needed to improve through ongoing training, and education of the healthcare workers as well as surveillance reduces infection by the infection control committee. This research work will help future researchers to update/modify their institutional bundle care policy to prevent device-associated hospital-acquired infection looking forward to evaluating the genetic pattern for the MDR gene of isolated microorganisms. This research work may be helpful for earlier detection of microorganisms causing nosocomial infection and appropriate management would help in reducing mortality in the ICU’s.
Ethical approval
The research/study approved by the Institutional ethical committee (IEC) at Agartala Government Medical College and GBP Hospital, number IEC Ref. No. 3935, dated 15th March 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
References
- Bennett and Brachman’s. Hospital Infections. Seventh edition. by William R. Jarvis. United Kingdom: LWW; 2022:1–946.
- When hospitals infect you. 2017, February 11. The Hindu. [accessed 2023 Nov 21]. http://www.thehindu.com/sci-tech/health/When-hospitals-infect-you/article17289370.ece
- Catheter-Associated urinary tract infection. Curr Opin Infect Dis. 2012;25:365-70.
- [CrossRef] [PubMed] [Google Scholar]
- Catheter-associated urinary tract infections in adult intensive care units at a selected tertiary hospital, Addis Ababa, Ethiopia. PLoS One. 2022;17:e0265102.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Urinary Tract Infection | Antibiotic Use. [accessed 2023 Nov 21]. https://www.cdc.gov/antibioticuse/uti.html#:∼:text=Frequent%20urination,the%20groin%20or%20lower%20abdomen.
- Catheter-related urinary nosocomial infections in intensive care units: An epidemiologic study in North of Iran. Caspian J Intern Med. 2017;8:76-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of multidrug-resistant strains in device associated nosocomial infection and their in vitro killing by nanocomposites. Ann Med Surg. 2022;78:103687.
- [CrossRef] [PubMed] [Google Scholar]
- Standard Operating Procedure. November 2018. Available at: https://www.haisindia.com/upload/fileuploads/1543398274_SOP%20updated%20November%202018.pdf.
- National Healthcare Safety Network (NHSN) - Current CAUTI Surveillance Protocol. [accessed 2023 Nov 21]. URL. https://www.cdc.gov/nhsn/PDFs/pscManual/7pscCAUTIcurrent.pdf
- Improving Diagnosis and Treatment of Maternal Sepsis: A Quality Improvement Toolkit. Stanford, CA: California Maternal Quality Care Collaborative; 2022. p. :1-66. [accessed 2023 Nov 21]. https://www.cmqcc.org/system/files/resources/Sepsis%20Appendix%20E.pdf
- Midstream specimen of urine (MSU) in Men. [accessed 2023 Nov 21]. https://patient.info/mens-health/urine-infection-in-men/midstream-specimen-of-urine-msu
- Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis. 2004;38:1150-8.
- [CrossRef] [PubMed] [Google Scholar]
- CLED Agar Composition, Uses, and Typical Colony Characteristics. Microbeonline. (Accessed on: 3rd March, 2022). [accessed 2023 Nov 21]. URL: https://microbeonline.com/cled-agar-composition-uses-typical-colony-characteristics/
- Catheter-Associated urinary tract infection in intensive care unit patients at a tertiary care hospital, Hail, Kingdom of Saudi Arabia. Diagnostics. 2022;12:1695.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Gender and age-dependent etiology of community-acquired urinary tract infections. Sci World J. 2012;2012:349597.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic resistance and trend of urinary pathogens in general outpatients from a major urban city. Int Braz J Urol. 2007;33:42-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med. 2015;19:14-20.
- [CrossRef] [PubMed] [Google Scholar]





