Translate this page into:
Use of Telemedicine in Evaluation of Pediatric Surgical Patients in COVID-19 Time
Address for correspondence Anand Pandey, MS, MCh, MAMS, Department of Pediatric Surgery, King George's Medical University, Lucknow 226003, Uttar Pradesh, India (e-mail: dranand27@rediffmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective
The word “telemedicine” literally translates to “healing at a distance.” In the current scenario of the coronavirus disease 2019 (COVID-19) pandemic and shut outpatient department, the patients are facing difficulty in consultation. This article evaluated the use of telemedicine in the management of pediatric surgical patients.
Materials and Methods
In this observational cohort study, from April 2020 to August 2020, all patients who took advice on phone/WhatsApp were assessed for addressing their complaints. The data was collected and analyzed.
Result
A total of 307 patients were provided consultation via telecommunication. The male to female ratio was 2.3:1. Fifty-six (18.2%) patients called on an emergency basis, while the remaining 251 (81.8%) patients called for nonemergency or routine problems. Of these, attendants of 25 (8.14%) patients were not able to state the situation adequately. They were called to the department. Of these, 11 (3.5% of total) patients were admitted. One-hundred and eighty-three (59.6%) patients were in the department's follow-up, while the remaining 124 (40.4%) were new patients. The attendants of 296 (96.4%) patients were satisfied by using this modality of consultation.
Conclusion
In the current scenario, telecommunication may help us to avoid unnecessary travel to the hospital. It may be helpful to deal with minor clinical complaints and evaluating for an emergency.
Keywords
COVID-19
telemedicine
pediatric surgery
teleconsultation
Introduction
Coronavirus disease 2019 (COVID-19) is defined as an illness caused by a novel coronavirus, now called severe acute respiratory syndrome coronavirus 2.1 As of now, it is an ongoing pandemic with a loss of millions of lives and other problems. A preventive, nationwide lockdown was imposed in India from March 25, 20202 because of the infectivity and mortality risks. Since the imposition of lockdown, the outpatient department (OPD) services were also stopped. It affected the patients who required treatment due to non-COVID-19 reasons.
Telemedicine uses electronic information and communications technologies to support healthcare when distance separates the participants.3 Since patients and their attendants could not attend the OPD, an attempt to provide advice was undertaken by using telemedicine. This article presents the analysis of the feasibility and effects of telemedicine in Pediatric Surgery during COVID-19 times.
Materials and Methods
A retrospective observational cohort study was conducted in the department of pediatric surgery of a university hospital from April 2020 to August 2020. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines endorsed by the EQUATOR network for conducting this study.
The attendants called on a designated number displayed on the website for their complaints. The calls were first attended by the senior residents (pursuing 3-year MCh. Pediatric Surgery course). It was discussed with the consultants of the department. The follow-up patients also called on the numbers made available to them by the department. WhatsApp message/video calling, if available, was used (►Fig. 1).

- Screenshots of the teleconsultation provided during the course of treatment.
The data of patients were evaluated for age (< 28 days, 28 days to 1 year, and > 1 year), sex, complaints, the system involved, follow-up or new patient, treatment prescribed, and satisfaction with the response provided.
The treatment prescribed was on the basis of the complaints and the diagnosis made; for example, patients of vestibular fistula were prescribed lactulose for constipation; ostomy management with the addition of multivitamins was prescribed for patients with ileostomy/colostomy, etc. Review in OPD was advised for patients with nonemergency problems, such as patients with hypospadias, etc.
If a patient was suspected of having a clinical problem needing surgical intervention or in-hospital observation, he/she was advised to come to the department for admission. In a subset of patients, we could not ascertain whether it was an emergency or not. They were called to attend the department, and a decision to admit or not was taken at that time. Those patients who had been advised treatment on the phone were asked to call again to assess the effect of treatment and satisfaction of the attendants (►Fig. 2). The satisfaction was rated on an ordinal scale having three parameters (satisfied, neutral, and dissatisfied). The consent of the parents/attendants was obtained to use the data for analysis.
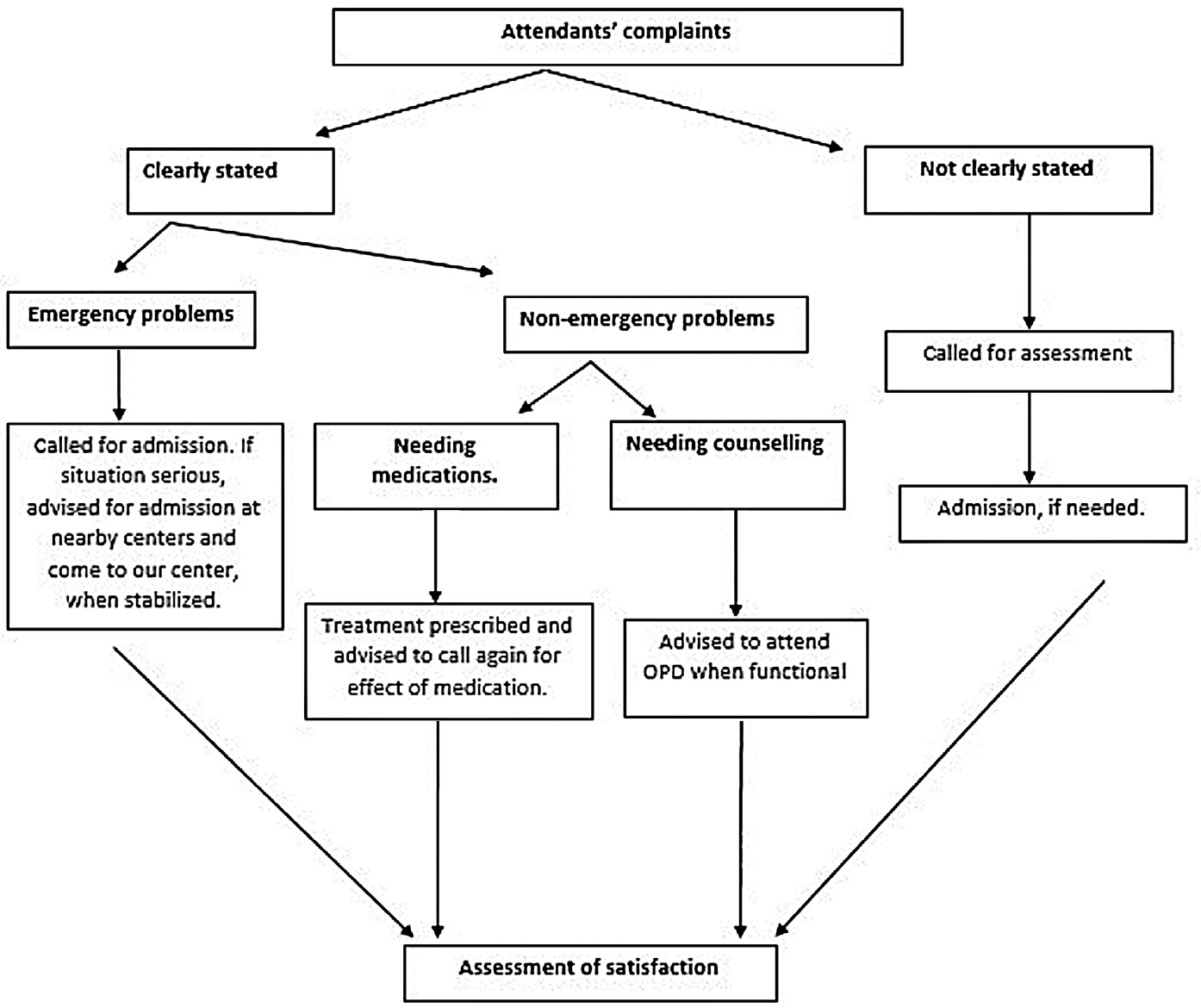
- Management algorithm for patients seeking telemedicine consultation.
All the data was entered into a Microsoft Excel sheet, and tables were analyzed. The values are presented as numbers and percentages.
Results
The duration of this study was 5 months. During this period, 307 patients were evaluated. Most of the patients were more than 1 year of age (►Table 1). The male to female ratio was 2.3:1, and the corresponding numbers to this ratio were 215 (70%) and 92 (30%), respectively. Fifty-six (18.2%) patients called on an emergency basis, while the remaining 251 (81.8%) patients called for nonemergency or routine problems. Of these, attendants of 25 (8.14%) patients could not state the situation adequately. They were called to the department. Of these, 11 (3.5% of total) patients were admitted.
| Age | Number (%) |
|---|---|
| Up to 1 month | 33 (10.7) |
| 1 to 12 months | 68 (22.1) |
| >12 months | 206 (67.1) |
| Total | 307 (100.0) |
Note: Most of the patients were beyond infantile age.
One-hundred and eighty-three (59.6%) patients were in the department's follow-up, while the remaining 124 (40.4%) were new patients. The most common major system involved was the gastrointestinal system (►Table 2), with a total of 162 (52.8%) patients, followed by the urinary system (111, 36.2% of patients). One hundred and eighty-three (59.6%) patients were reassured and advised to attend the OPD once it is open. The oral prescription of medication was done in 46 (15%) patients. Fifty-three (17.3%) patients were believed to need admission for conditions, such as congenital malformations and acute abdomen.
| System involved | Number (%) |
|---|---|
| Gastrointestinal | 162 (2.8) |
| Urinary system | 111 (36.2) |
| Nervous system | 23 (7.5) |
| Musculoskeletal | 5 (1. 6) |
| Spine | 5 (1.6) |
| Reproductive system | 1 (0.3) |
| Total | 307 (100.0) |
Note: Gastrointestinal system was the most common system involved.
Spine has been presented separately to highlight neural tube defects.
Overall, the attendants of 296 (96.4%) patients were satisfied by using this modality of consultation. The remaining 11 (3.4%) of attendants were not satisfied. They did not follow the instructions and did not call for further advice.
Discussion
Pediatric surgical services have been severely affected by the COVID-19 pandemic.4,5 Our department was no exception to it. As emergency procedures could not be delayed, the brunt of delayed surgery falls mostly on nonemergency patients. As OPDs were closed, the consultation was also not possible. It was difficult for patients as they were at risk of contracting the infection if coming to the hospital and not coming to the hospital affected the adequate care needed by them.6
The COVID-19 pandemic significantly affected traditional healthcare delivery systems. There was a need for physical distancing coupled with patients' needs, which necessitated alternatives to in-person visits by the healthcare professionals.7 Sensing the problem for all patients, the Government of India allowed telemedicine consultation. The Medical Council of India (MCI) allowed telemedicine by making it a part of the MCI Code of Medical Ethics. It was included as an amendment to the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002, by adding Regulation 3.8 titled “Consultation by Telemedicine” in the said regulations, and telemedicine guidelines included in appendix 5 of the regulations.8
It has been observed that local practitioners are less inclined to manage pediatric surgical patients due to limited technical skills in their management and fear of postoperative complications.9 Our patients also faced this problem. Telemedicine consultation helped them to have medical advice from our department. As evident from the algorithm, all those patients in whom the attendants could not specifically express themselves on the phone were called for assessment in the department. It was done to avoid missing any emergency patient. It can be seen that 11 of those 25 patients were admitted, which is 44%, thus suggesting our assumption to be right. Though patient satisfaction was 96% in this study, the treating surgeon is more satisfied if the patient is examined physically. Hence, 96% satisfaction is for the patients and not the doctors.
There are various pros and cons to using telemedicine. The pros include time-saving, easy accessibility, physical distancing, triage of patients, prescription for first aid and refill prescriptions, cost-effectiveness, and reduction in overcrowding. The cons include technological issues, such as poor Internet connectivity, lack of physical examination, possibility of a missed diagnosis, patient literacy, medicolegal issues, errors in prescription and its honor by the chemist, and maintenance of confidentiality. The benefits as mentioned above were also noted by us. The cons, such as lack of physical examination, Internet connectivity, were also present. However, the lack of physical examination was managed by calling those patients who appeared to be an emergency.8
There are some reports of successful use of telemedicine in pediatric management and pharmacy prescription, thereby continuing the healthcare management in the critical period of the COVID-19 pandemic.7,10 Regarding the strengths of this study, it is one of the first to have studied telemedicine in pediatric surgery in India, which had a simple methodology, and we were able to provide timely advice to the patients. There were some limitations in this study. It was a retrospective study. Besides, we had to rely on attendants' statements made on the phone and limited assessment of satisfaction on an ordinal scale. However, we still believe that it was the best option for us to provide unimpeded healthcare services to our patients.
In conclusion, telemedicine consultation may help avoid unnecessary travel to the hospital given the current scenario. It may be helpful to deal with minor clinical complaints and evaluating for an emergency.
Author Contributions
R.K.R. and A.P. conceptualized the idea; A.P., A.G., and G.S. conducted the literature review; A.P., R.K.R., and G.S. wrote the first draft of the manuscript; J.D.R. conducted the critical review of the manuscript; all authors read and approved the final draft of the manuscript.
Ethical Approval
The data of the present study were collected in the course of common clinical practice, and accordingly, the signed informed consent was obtained from each patient for any surgical and clinical procedure. The study protocol was in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments. Because it was a retrospective study, formal consent for this study was not required, and no approval of the institutional research committee was needed.
Conflict of Interest
None declared.
References
- Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
- [Google Scholar]
- COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr. 2020;14(05):733-737.
- [CrossRef] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine. Telemedicine: A Guide to Assessing Telecommunications in Health Care 1996:1. at: https://www.ncbi.nlm.nih.gov/books/NBK45440/ (accessed )
- [Google Scholar]
- Pediatric surgery during the COVID-19 pandemic: an International Survey of Current Practice. Eur J Pediatr Surg 2020 DOI: 10.1055/s-0040-1714714
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric surgery during coronavirus disease lockdown: multicenter experience from North India. Formos J Surg. 2020;53:216-222.
- [CrossRef] [Google Scholar]
- Using telemedicine during the COVID-19 pandemic. Indian Pediatr. 2020;57(07):652-657.
- [CrossRef] [PubMed] [Google Scholar]
- The paediatric weight management office visit via telemedicine: pre- to post-COVID-19 pandemic. Pediatr Obes. 2020;15(08):e12694.
- [CrossRef] [PubMed] [Google Scholar]
- at: https://www.mohfw.gov.in/pdf/Telemedicine.pdf (accessed )
- Active telephonic follow-up during COVID-19 lockdown: initial experience. Indian Pediatr. 2020;57(08):769.
- [CrossRef] [PubMed] [Google Scholar]
- Use of telemedicine to provide clinical pharmacy services during the SARS-CoV-2 pandemic. Am J Health Syst Pharm. 2020;77(13):1005-1006.
- [CrossRef] [PubMed] [Google Scholar]






