Translate this page into:
Validation of neck length and neck circumference together as predictors of difficult airway in overweight and obese females
* Corresponding author: Dr. Naveen Mathew A, MD, Department of Anaesthesiology, Critical Care and Pain medicine, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, New Delhi, India. naveenmathieu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kapoor R, Choudhary M, Saxena AK, Mathew A N, Jindal P. Validation of neck length and neck circumference together as predictors of difficult airway in overweight and obese females. Ann Natl Acad Med Sci (India). doi: 10.25259/ANAMS_275_2024
Abstract
Objectives
Neck circumference (NC) and neck length are used as predictors of a difficult airway. There is inconsistency in the literature regarding the factors that predict a difficult airway in obese patients. The primary objective was to assess the correlation between neck length and neck circumference with the intubation difficulty score (IDS). The secondary aim was to examine the correlation of IDS with the modified mallampati class (MMP), thyromental distance (TMD), thyromental height, the neck circumference-to-thyromental distance ratio (NC:TMD), and the presence of a neck hump.
Material and Methods
This double-blind, cross-sectional study involved 50 female patients, aged 18-60 years, with a body mass index (BMI) ≥ 25 kg m-2, who were planned for elective surgery requiring general anesthesia. Participants who were pregnant, had a BMI below 25 kg m-2, required rapid sequence intubation, had a history of cervical spine injury, or were male were excluded from the study. The IDS was utilized to assess intubation difficulty. Neck length and neck circumference were measured, and their predictive ability for a difficult airway was compared with IDS. Additionally, IDS was analyzed in relation to MMP class, thyromental distance, NC:TMD, thyromental height, and the presence of a neck hump. Data analysis was done using one-way ANOVA with Tukey’s post hoc tests, the chi-square test, and student’s t-test, with p ≤ 0.05 set as the significance level.
Results
Neck length (<7 cm) alone showed a strong correlation with a difficult airway. An average neck length of 4.9 ± 0.63 cm has been positively correlated with IDS >5, while a neck length of 6.7 ± 0.47 cm corresponded to IDS 0. An NC of ≥36 cm was significantly linked to moderate to difficult intubation, as determined by the IDS. A mean NC of 41.91 ± 4.98 cm was associated with IDS > 5, and a NC of 37 ± 1.23 cm was associated with IDS 0. The MMP class and NC:TMD ratio were also effective in predicting a difficult airway.
Conclusion
In our study, we observed a statistically significant correlation (p-value < 0.05) between both neck length and NC with the IDS in overweight and obese females.
Keywords
Airway
General Anesthesia
Difficult airway
Elective surgical procedure
Intubation difficulty score
Neck length
Neck circumference
INTRODUCTION
Recognizing the possibility of a difficult airway is crucial for effective preparation, which involves selecting the right equipment and techniques and having experienced personnel for difficult airway management to prevent any complications related to the airway. Difficult laryngoscopy is observed in 1.5% to 8% of cases under general anesthesia.1 Challenges in managing the difficult airway continue to be a primary factor contributing to anesthesia-related morbidity and mortality. Therefore, effective pre-anesthetic assessment to anticipate difficult airways is essential for reducing surgical risks and enhancing patient outcomes.
Several bedside tests have been developed to predict airway management challenges, but their sensitivity and specificity vary widely. Despite various predictors, including obstructive sleep apnea syndrome history, Mallampati score, neck circumference (NC), age, gender, neck length, body mass index (BMI), and Wilson score, no single factor provides reliable diagnostic accuracy for difficult intubation, particularly in individuals with obesity.2-4
NC strongly predicts difficult intubation, particularly in patients with a BMI exceeding 40 kg m-2. The probability of difficult intubation increases from approximately 5% at an NC of 40 cm to 35% at 60 cm.5
The predictive value of NC for difficult intubation is highly variable, especially in obese individuals, due to the dependence of cut-off values on BMI. Riad et al.6 (2016) found that an NC greater than 42 cm independently predicted difficult intubation in morbidly obese patients. The research by Brodsky et al.7 (2002) noted a significant female preponderance in their study, with a median NC of 46 cm in the ‘easy intubation’ group. Conversely, Gonzalez et al.8 (2008) suggested NC >43 cm should raise suspicion for difficult intubation, implying that a substantial proportion of the group classified as having “easy intubation” by Brodsky may have been misclassified when evaluated using Gonzalez et al.’s.8 (2008) threshold. Liaskou et al.5 (2014) further demonstrated that NC cut-offs vary between genders, with a significant improvement in predictive accuracy for difficult intubation when gender-specific thresholds were applied. These findings support the use of gender-specific NC cut-offs.
A short neck is often associated with an increased likelihood of a difficult airway. However, there are no established specific cut-off values for neck length that definitively indicate a difficult airway. Additionally, Faraj et al.3 (2023) observed that a neck length of 7.6 ± 0.9 cm was associated with moderate to major intubation difficulty and suggested that a neck length of 8 cm or less, measured from the mastoid process to the shoulder, may indicate a potentially difficult airway in obese individuals. They further recommended the inclusion of other variables and lean patients in future studies to improve predictive accuracy.
Considering the gender-specific variations in NC and the possibility of integrating neck length with other predictors, this double-blinded, cross-sectional comparative study was carried out to assess neck length and NC together as key predictors of difficult intubation in overweight and obese females, reducing gender as a confounding factor.
MATERIAL AND METHODS
This research, structured as a randomized, double-blind, cross-sectional analysis, approved by the institutional ethics committee (IEC-HR), adhered to the Declaration of Helsinki and was registered on www.ctri.nic.in before enrollment. This study was conducted at a tertiary care hospital between January 2021 and June 2022, with all participants providing written informed consent. The study included 50 female patients, aged 18-60 years, with a BMI ≥ 25 kg m-2, who were scheduled to undergo elective surgeries requiring general anesthesia. Participants were excluded from this study if they were pregnancy, required rapid sequence intubation, exhibited visible neck swelling, had a mouth opening of less than 1.5 cm, or had cervical spine trauma. Participants were thoroughly evaluated in a pre-anesthetic clinic. The following parameters were noted: mouth opening, modified mallampati class (MMP), thyromental distance (TMD), thyromental height, and sternomental distance (SMD). All measurements were done using measuring tape in a sitting position. With the head positioned neutrally, neck length was assessed by measuring postero-laterally from the tip of the mastoid process to the inflection point where the neck meets the shoulder.3 Additionally, while maintaining the same neutral head position, NC was measured at the level of the thyroid cartilage. Any presence of a neck hump was noted.
Patients were instructed to maintain an eight-hour fasting period (nil per oral) prior to the start of the surgery. Premedication consisting of alprazolam at a dosage of 0.5 mg and ranitidine at a dosage of 150 mg, given the evening before and the morning of the surgery. Upon the patient’s entry into the operating theater, baseline hemodynamic values were recorded. The standard protocol for general anesthesia was followed. Pre-oxygenation was performed for a period of three minutes. General anesthesia was initiated with intravenous propofol at a dosage of 1.5 to 2 mg kg-1 body weight (BW) and adjusted until the patient no longer responded to stimuli. Intravenous cisatracurium (0.2 mg kg-1) was administered to achieve neuromuscular blockade after confirming adequate bag and mask ventilation, and endotracheal intubation was done after 2–3 minutes, and the duration of intubation was documented. Intubation difficulty was evaluated with the intubation difficulty scale (IDS), which includes seven factors: number of intubation attempts, additional personnel involved, alternative methods used, vocal cord positioning, Cormack-Lehane grade, external laryngeal manipulation, and increased force on the laryngoscope. To minimize bias, a senior resident anesthesiologist not associated with the study performed the intubation. The percentage of glottic opening score, representing the extent of glottic opening, was recorded during each laryngoscopy. Additionally, any maneuvers performed to enhance laryngeal visualization or ventilation were noted. It was pre-decided that in the event of a failed intubation (more than three attempts), a Pro-Seal laryngeal mask airway would be placed, and a note of the same would be made. The neuromuscular block was reversed using intravenous neostigmine (0.05 mg kg-1 bw) and intravenous glycopyrrolate (0.01 mg kg-1 bw) upon completion of the surgical procedure. Post-extubation hemodynamic parameters were noted.
After a thorough review of the existing literature, no benchmark study directly related to our primary objective was identified. Therefore, 50 female participants were recruited, making this a pilot study.
Data analysis was conducted using IBM SPSS Statistics version 20.0. One-way ANOVA with Tukey’s post hoc test was used for continuous variables, and categorical variables were evaluated using the chi-square test. Statistical significance was set at p ≤ 0.05.
RESULTS
Fifty female patients with a BMI of 25 kg m-2 or higher were included. All 50 patients were intubated successfully, with no cases of failed intubation. Of these, 11 patients had IDS above 5 (moderate to major difficulty), 24 had scores between 0 and 5 (mild difficulty), and 15 had a score of 0 (easy intubation) [Figure 1].
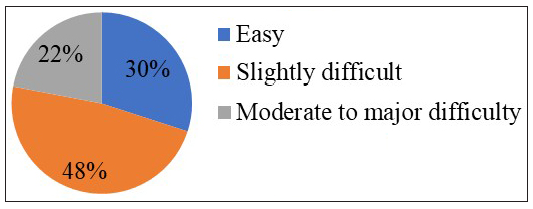
- Showing distribution of cases according to intubation difficulty score.
Among 50 patients, those with an IDS >5 (n = 11) had a mean neck length of 4.91 ± 0.63 cm (p = 0.001). Patients with IDS scores ranging from 0 to 5 (n = 24) had a mean neck length of 5.67 ± 0.48 cm, while patients with an IDS score of 0 (n = 15) had a mean neck length of 6.72 ± 0.47 cm [Table 1].
| IDS | Number of cases | Mean neck length (cm) | Std. Deviation | Significance (One-way ANOVA) | p value (Tukey’s test at 5%) |
|---|---|---|---|---|---|
| IDS 0 | 15 | 6.72 | .47 | 0.000 | 0.000 |
| IDS 0-5 | 24 | 5.67 | .48 | 0.001 | |
| IDS>5 | 11 | 4.91 | .63 | 0.001 |
P value <0.05 taken as significant. ANOVA: Analysis of variance, IDS: Intubation difficulty score
Eleven patients had an IDS >5 with an NC of 41.91 ± 4.98 cm (p = 0.001), and 24 patients had an IDS of 0-5 with an NC of 37.29 ± 3.02 cm. Fifteen out of the 50 patients had an IDS of 0, with an NC of 32.33 ± 1.23 cm [Table 2]. The study results revealed a strong Spearman’s rho correlation between IDS, NC, and neck length [Table 3]. Eight patients with MMP class 3 had an IDS > 5 (p = 0.001, [Figure 2]).
| IDS | Number of cases | Neck circumference (cm) (SD) | Significance (One Way ANOVA) | p value (Tukey’s test at 5%) |
|---|---|---|---|---|
| IDS 0 | 15 | 32.33 (1.23) | 0.001 | 0.000 |
| IDS 0-5 | 24 | 37.29 (3.02) | 0.001 | |
| IDS>5 | 11 | 41.91 (4.98) | 0.001 |
P value <0.05 is significant. ANOVA: Analysis of variance, IDS: Intubation difficulty score, SD: Standard deviation
| Parameters | Correlation | Neck length | Neck circumference | IDS |
|---|---|---|---|---|
| Neck length | Spearman rho’s correlation coefficient | -0.821* | -0.807* | |
| significance(2-tailed) | 0.000 | 0.000 | ||
| Neck circumference | Spearman rho’s correlation coefficient | -0.821* | 0.774* | |
| significance(2-tailed) | 0.000 | 0.000 | ||
| IDS | Spearman rho’s correlation coefficient | -0.807* | 0.774* | |
| significance(2-tailed) | 0.000 | 0.000 |
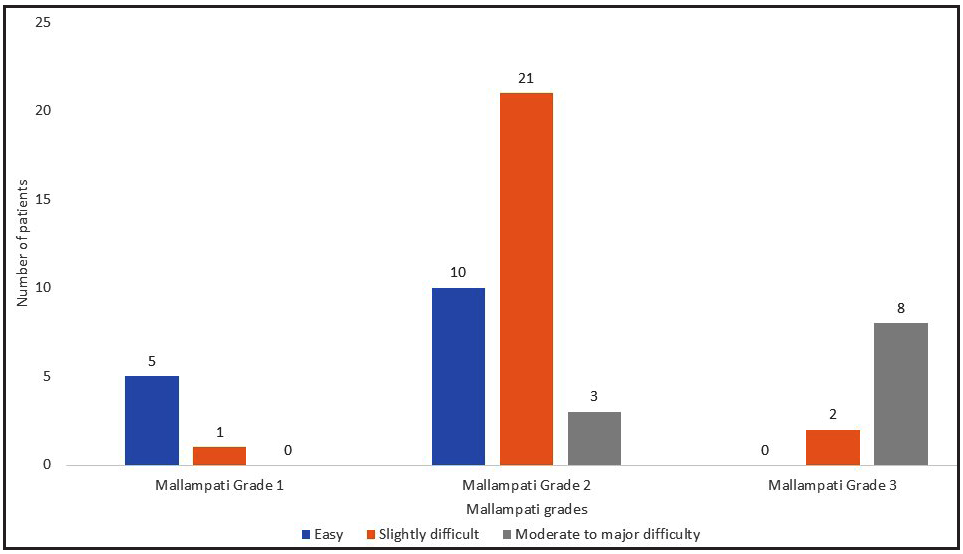
- Association of IDS with mallampati class (MMP). IDS: Intubation difficulty score.
In the study, patients with IDS >5 had a TMD of 7.50 ± 0.82 cm, patients with IDS 0-5 had a TMD of 7.87 ± 0.66 cm, and patients with IDS 0 had a TMD of 8.46 ± 0.63 cm (p = 0.003) [Table 4].
| IDS |
Thyromental Distance in cm Mean (SD) |
Significance (One-way ANOVA Test) |
p value (Tukey’s at 5%) |
|---|---|---|---|
| IDS 0 | 8.46 (0.63) | 0.003 | 0.035 |
| IDS 0-5 | 7.87 (0.66) | 0.003 | |
| IDS >5 | 7.50 (0.82) | 0.317 |
P value < 0.05 is significant. IDS: Intubation difficulty score, SD: Standard deviation, ANOVA: Analysis of variance
We found that an NC:TMD of 5.60 ± 1.20 was associated with IDS >5, an NC:TMD of 4.66 ± 0.66 had IDS 0-5, and an NC:TMD of 3.78 ± 0.28 was associated with IDS 0 (p = 0.001) [Table 5].
| IDS | NC: TMD |
Significance (One-way ANOVA Test) |
p-value (Tukey’s Test at 5%) |
|---|---|---|---|
| IDS 0 | 3.78 (0.28) | 0.001 | 0.002 |
| IDS 0-5 | 4.66 (0.66) | 0.000 | |
| IDS >5 | 5.60 (1.20) | 0.003 |
P value <0.05 is taken as significant. IDS: Intubation difficulty score, NC:TMD: Neck circumference-to-thyromental distance ratio
The study found that patients with IDS >5 had an intubation time of 37.55 ± 10.38 seconds, those with IDS 0 took 10.60 ± 1.18 seconds, and patients with IDS between 0 and 5 had a time of 25.92 ± 7.59 seconds. (p = <0.005). In the study population, the thyromental height, SMD, and inter-incisor gap did not demonstrate a significant association with IDS.
DISCUSSION
A short neck has been proposed as one of the causes of difficult intubation, but the precise neck length defining ‘short’ in relation to difficult intubation remains unclear. Limited neck length restricts movement during laryngoscopy, preventing optimal neck extension and impairing vocal cord visualization, which is why obese individuals are often classified as having a difficult airway. It has also been postulated that neck fat and neck hump could contribute to difficult intubation, particularly in obese individuals. Furthermore, since there is no clear threshold for neck length as a predictor of difficult airway, it becomes imperative to combine another parameter to effectively predict difficult airway.
Fat distribution differs by gender, resulting in variations in NC between males and females. The ability of screening tests to identify difficult intubation can be unreliable when relying on a single test, particularly in individuals with obesity.4 Therefore, this limitation has prompted investigations into combining risk factors or individual tests to improve diagnostic accuracy. Multivariable risk assessment tools, including the El-Ganzouri and Wilson scores, have been applied in various studies to predict difficult intubation.9-11 However, the multiple variables in these scores can make their use laborious and cumbersome.
Thus, combining two key risk factors could improve diagnostic precision without substantially complicating the evaluation.
Given this background, we conducted this cross-sectional observational study to assess neck length and NC and their correlation with IDS. An IDS score of 0 signifies easy intubation, 0–5 indicates mild difficulty, and >5 represents moderate to major difficulty in intubation. We observed a significant correlation (p < 0.05) between both neck length and NC with the IDS in overweight and obese females.
In the present study, an average neck length of 4.9 ± 0.63 cm was positively associated with IDS >5, indicating moderate to difficult intubation. A neck length of 5.7 ± 0.48 cm was associated with slight difficulty in intubation, while a neck length of 6.7 ± 0.47 cm was found to be easy to intubate. Moderate to difficult intubation was observed in 25% of patients with a neck length of less than 7 cm. Thus, a positive correlation between short neck length and difficult intubation was identified.
Through an extensive literature review, we found only one study by Faraj et al.,3 (2023) which proposed a short neck as a predictor of a difficult airway. They postulated that a mean neck length of 7.6 cm was correlated with difficult intubation. The variation in results may be due to gender-based differences in anthropometric variables. Additionally, this study was carried out in a genetically distinct population at a tertiary care hospital in India.
We also observed that as neck length decreases, the IDS increases. Thus, the absolute value of neck length showed a significant correlation with the IDS (p < 0.05). Faraj et al.3 (2023) also proposed that adding additional parameters into the evaluation of a short neck could enhance the prediction of difficult intubation. Gonzalez et al.8 (2008) found that individuals with a NC exceeding 43 cm had a 37% greater likelihood of experiencing intubation difficulties, with a 92% sensitivity.
In the present study, we included NC as an additional parameter to predict difficult intubation. We measured NC at the cricoid level in all individuals, and the grades of difficult intubation were determined using the IDS. Participants were grouped based on their NC: those with a circumference <36 cm and those with a circumference of 36 cm or more. IDS >5 was significantly higher in individuals with an NC ≥36 cm, at 37%, compared to just 4.3% in those with an NC <36 cm.
Further analysis revealed that mean NCs of 41.1 ± 4.9 cm, 37.2 ± 3.02 cm, and 32.3 ± 1.2 cm were associated with moderate/major, slightly difficult, and easy intubation, respectively. A strong positive correlation (p < 0.001) was observed between NC and IDS, indicating that as NC increases, the potential for difficult intubation also increases. Liaskou et al.5 (2014) identified an NC threshold of >37.5 cm in adults with a BMI below 35 kg m-2, reporting a sensitivity of 54.2% and a specificity of 77.3% (p = 0.02). We also observed elevated NC (mean 41.9 ± 4.9 cm) in individuals with IDS >5.
Difficult intubation occurred in 37% of individuals with an IDS score > 5 and an NC ≥ 36 cm (mean: 41.9 ± 4.9 cm). Riad et al. (2016) observed that patients with a BMI over 50 kg m-2 had a fivefold higher likelihood of encountering difficult intubation.6 Similarly, Lundstrom et al.12 (2011) identified a BMI over 35 kg m-2 as a significant determinant of intubation difficulty. These observations were consistent with Juvin et al.,13 (2003) who examined lean and obese patients (n=263) and reported comparable results regarding difficult intubation incidence.
In our study, 8 out of 10 (80%) patients with MMP class III experienced major difficulty with intubation, demonstrating a significant association between MMP class and IDS (p < 0.001). However, Lundstrom et al.12 (2011) found the MMP classification alone to have poor prognostic value for predicting difficult intubation.
We observed that a mean TMD of 7.5 ± 0.82 cm was associated with difficult intubation, with an IDS >5. Frerk et al. (1991) observed similar results, indicating that a TMD of <7 cm was linked to a higher number of difficult intubations.14 Unlike the study by Frerk et al., which examined a general population, our research focused exclusively on female individuals with a BMI of 25 kg m-2 or higher.
SMD, IIG, and thyromental height were evaluated as additional airway assessment parameters in the study but did not demonstrate a significant correlation with IDS. In the present study, we also observed that difficult intubation (IDS >5) was associated with a mean NC:TMD ratio of 75.6 ± 1.2. A mean NC:TMD ratio of 4.6 ± 0.66 was associated with slightly difficult intubation, and a mean NC:TMD ratio of 3.7 ± 0.28 was easy to intubate. Intergroup analysis revealed a statistically significant result, indicating that as the NC:TMD ratio increases, the IDS also increases.
A key strength of this study is that a single investigator conducted all observations, thereby eliminating inter-observer variability. However, this study does have a few limitations. Although the laryngoscopy was performed by a senior resident with one year of experience, variability in performance among different anesthesiologists could be a limitation of our study. Due to its single-center design, this study necessitates validation through a multicenter, large-scale research. Furthermore, the exclusive focus on Indian females limits the generalizability of our results to other demographics. Future studies should include diverse populations to improve the applicability of these findings.
The study by Workeneh et al.15 (2017) concluded that no individual test could perfectly predict difficult laryngoscopy and intubation with 100% accuracy in both sensitivity and specificity. Thus, there remains scope to discover new parameters that can more effectively predict a difficult airway, especially in overweight and obese individuals.
CONCLUSION
The present study validates neck length and NC together as predictors of difficult airways in overweight and obese individuals. Further research is required to conclusively define cut-off values for the short neck and to conclusively predict difficult airway with better accuracy.
Authors’ contributions
RK: Concept and design, review of literature, data collection and handling, data interpretation, preparing a draft of manuscript, review of manuscript and approval of final version to be published; MC: Data collection and handling, data interpretation, preparing a draft of manuscript, review of manuscript and approval of final version to be published; AKS: Concept and design, data interpretation preparing a draft of manuscript, review of manuscript and approval of final version to be published; NMA: Review of literature, preparing a draft of manuscript, review of manuscript; PJ: Concept and design, review of literature.
Ethical approval
The research/study approved by the Institutional Review Board at University College of Medical Sciences, Delhi, number IECHR/2020/PG/46/87-R1, dated 24th December,2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- A systematic review (meta-analysis) of the accuracy of the mallampati tests to predict the difficult airway. Anesth Analg. 2006;102:1867-78.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between neck length, sleep, and psychiatric disorders: A psychiatric aspect. Korean J Fam Med. 2015;36:156-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Short Neck, A new criterion for airway assessment: A pilot, cross sectional single blind study. J Anesth Clin Res. 2023;11:954.
- [Google Scholar]
- Predicting difficult intubation in apparently normal patients. Anesthesiology. 2005;103:429-37.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic features of the neck as predictive markers of difficult direct laryngoscopy in men and women: A prospective study. Indian J Anaesth. 2014;58:176-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: A prospective observational study. Eur J Anaesthesiol. 2016;33:244-9.
- [CrossRef] [PubMed] [Google Scholar]
- Morbid obesity and tracheal intubation. Anesth Analg. 2002;94:732-6.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of increased neck circumference to intubation difficulties in obese patients. Anesth Analg. 2008;106:1132-6.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of the El-Ganzouri multivariate risk index for difficult tracheal intubation: a comparison of Glidescope videolaryngoscopy and conventional Macintosh laryngoscopy. Br J Anaesth. 2007;99:906-11.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197-204.
- [CrossRef] [PubMed] [Google Scholar]
- Poor prognostic value of the modified mallampati score: A meta-analysis involving 177 088 patients. Br J Anaesth. 2011;107:659-67.
- [CrossRef] [PubMed] [Google Scholar]
- Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003;97:595-600.
- [CrossRef] [PubMed] [Google Scholar]
- Magnitude and predisposing factors of difficult airway during induction of general anaesthesia. Anesthesiol Res Pract. 2017;2017:5836397.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





