Translate this page into:
Burden of Cardiometabolic Disorders among Subjects Undergoing Preventive Health Check-up: A Follow-up Study
Correspondence : Dr. Jitendra Nath Pande, Senior Consultant in Medicine, Sitaram Bhartia Institute of Science and Research, B-16, Qutub Institutional Area, New Delh-110016. Email: jnpande@hotmail.com.
Abstract
Objective:
To study the incidence of hypertension (HTN), diabetes mellitus and coronary artery disease (CAD) in a cohort of adult subjects.
Methods:
A total 2159 participants (mean age: 48.6±11.6 years; 1342 males and 817 females) who attended the hospital for a comprehensive health check up were recruited and followed-up as a cohort for a mean period of 3.5 years. Their baseline and follow-up evaluation included clinical examination, biochemical investigations and cardiac check-up.
Results:
At baseline, 64% participants were overweight or obese, 44.3% had HTN (grade I or above), 16.7% had diabetes mellitus with additional 29.3% having impaired fasting glucose or glucose intolerance, and 46.6% had metabolic syndrome. The prevalence of CAD at baseline was 6% in males and 3% in females. The incidence (per 1000 person-years of follow-up) of HTN, diabetes mellitus and CAD was 72.2, 26.3 and 12.2, respectively.
Conclusion:
The burden of cardiometabolic disorders and their risk factors is high in India. Urgent remedial public health preventive measures are required to curtail the emerging epidemic of cardiometabolic disorders.
Keywords
Hypertension
diabetes mellitus
coronary artery disease
cardiometabolic syndrome.
Introduction
India has a large burden of cardiovascular disease (CVD) due to high prevalence and suboptimal management of several risk factors including diabetes mellitus (DM), hypertension (HTN), obesity and dyslipidemia (1-3). There are few cohort studies reported from India, which provide data on incidence of coronary artery disease (CAD), HTN and DM in susceptible middle aged and elderly subjects.
A large number of apparently healthy subjects undergo preventive health check-up at Sitaram Bhartia Institute of Science and Research, New Delhi. Their evaluation includes detailed clinical history, physical examination and several investigations to assess their cardiovascular risk status. Many subjects undergo repeat evaluation after a variable period of time to assess changes in their status following life-style modifications and pharmacotherapy as prescribed at the time of the first visit. We utilized this opportunity to establish a follow-up cohort to determine the incidence of CAD, DM and HTN.
Methods
Study Design
Retrospective-cum-prospective cohort study.
Setting and Selection of Participants
Records of 5611 apparently-healthy adult subjects (>20 years) participating in preventive health check-up (PHC) at Sitaram Bhartia Institute of Science and Research, New Delhi from January 2000 to September 2009 were recruited as potential participants. Those with complete baseline information and fulfilling the eligible minimum follow-up of 150 days or more were invited to participate for follow-up (n=2453). Of those successfully contacted, 2098 (85.6%) consented for second evaluation, 13.7% refused and 0.7% were reported to have died (cause not known). Seventy one of these 2098 subjects were excluded from analysis on account of non-eligibility: age<20 years, period of follow-up<150 days, incomplete information and certain outliers.
Another 132 subjects were enrolled prospectively from October 2009 onwards, if the follow-up data for a minimum of 150 days was available. Thus, 2159 individuals formed the cohort and were included for analysis (Fig. 1). Clinical details were recorded in a structured form by a consultant in medicine. Information was recorded about the present symptoms, if any, with a detailed system review on direct questioning. Tobacco consumption, alcohol intake, anthropometry (height and weight) and blood pressure were recorded. Biochemical and other clinical investigations included plasma glucose (fasting and 2 hours after 75 g glucose), lipid profile, resting 12 lead electrocardiogram (ECG) and treadmill stress test (TMT)/ echocardiography. Details of current medications, if any, were recorded. Similar observations were recorded on follow-up. Ethical clearance was obtained from the local Institutional Ethics Committee. A written informed consent was obtained from each subject for the follow-up evaluation.
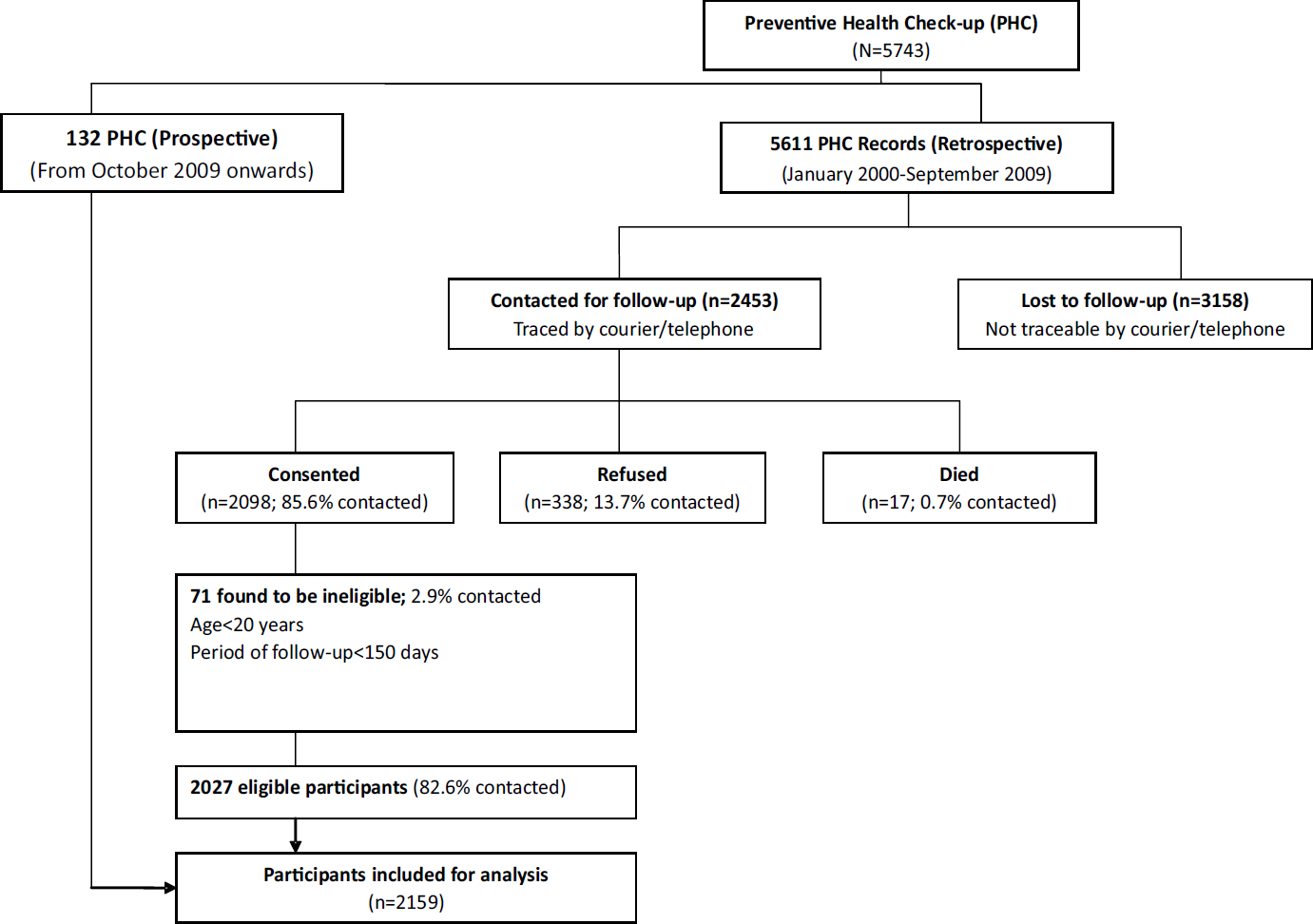
- Participant flow chart
Statistical Methods
Statistical analysis was undertaken using STATA (Ver 9.0). Appropriate log transformations were done for variables having skewed distributions (plasma glucose, total cholesterol, triglycerides, high density lipoprotein cholesterol (HDL-c), low density lipoprotein cholesterol (LDL-c). Significance of differences between mean of continuous variables at baseline and during follow-up were determined using Student's t-test for paired values. Student's t-test was used for assessing significance of difference in the means of continuous variables in different categories of subjects. Chi-square test was used to compare proportions in two groups.
Results
Baseline Characteristics
Of the 2159 participants, 1342 were males (mean age 48.5 ±12.0 years) and 817 females (mean age 48.8±11.0 years). Their weight, height, body mass index (BMI) and important physiological and biochemical characteristics are summarized in Table 1. One hundred and twenty eight of 817 women (15.6%) and 724 of 1342 men (54.0%) consumed alcohol (<120 G/week), the difference being highly significant (p<0.001). Three hundred and sixteen (14.4%) were current smokers while 185 (8.5%) had quit smoking. Prevalence of current or past smoking was significantly higher amongst men.
| Variable | Males | Females | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | P value* | Baseline | Follow-Up | P value* | |||||
| N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | |||
| Anthropometry | ||||||||||
| Weight (kg) | 1342 | 75.3(11.4) | 1342 | 75.6(11.7) | 0.0222 | 817 | 66.8(11.2) | 817 | 67.5(11.5) | 0.0000 |
| Height (cm) | 1342 | 169.6(6.5) | 1342 | 169.6 (6.6) | 0.8335 | 817 | 156.6(6.2) | 817 | 156.4(6.3) | 0.0000 |
| BMI (kg/m2) | 1342 | 26.1 (3.4) | 1342 | 26.2(3.5) | 0.0172 | 817 | 27.2 (4.4) | 817 | 27.6(4.5) | 0.0000 |
| Blood Pressure (mm Hg) | ||||||||||
| Systolic | 1329 | 131.5(18.3) | 1329 | 130.6(19.0) | 0.1076 | 804 | 128.0(19.0) | 804 | 127.8(18.9) | 0.7516 |
| Diastolic | 1329 | 82.8(10.2) | 1329 | 81.1 (10.6) | 0.0000 | 804 | 79.5 (9.5) | 804 | 78.1 (9.9) | 0.0001 |
| Glucose Profile (mg/dl)** | ||||||||||
| Fasting Plasma Glucose | 1292 | 104.7(1.2) | 1292 | 109.4(1.2) | 0.000 | 779 | 101.9(1.2) | 779 | 105.6(1.2) | 0.000 |
| Post Prandial Plasma Glucose | 1234 | 107.8(1.5) | 1234 | 105.5(1.5) | 0.0369 | 747 | 107.9(1.4) | 747 | 105.0(1.4) | 0.0186 |
| Lipid Profile (mg/dl)** | ||||||||||
| Total Cholesterol | 1272 | 180.9(1.2) | 1272 | 176.3(1.2) | 0.0000 | 765 | 184.3(1.2) | 765 | 182.6(1.2) | 0.2139 |
| Triglycerides | 1274 | 133.4(1.6) | 1274 | 134.0(1.6) | 0.7316 | 760 | 112.5(1.6) | 760 | 118.1 (1.6) | 0.0008 |
| HDGc | 1269 | 41.1 (1.2) | 1269 | 38.3(1.2) | 0.0000 | 756 | 47.0(1.2) | 756 | 45.4(1.2) | 0.0000 |
| LDL-c | 1262 | 110.1(1.4) | 1262 | 107.1 (1.4) | 0.0132 | 753 | 111.2(1.3) | 753 | 110.1 (1.3) | 0.4379 |
*P value between baseline and follow-up by paired Student's t-test; #P value between baseline and follow-up by two sample test of proportion;
** Geometric means using log transformation. BMI- Body Mass Index; HDL-c- High Density Lipoprotein Cholesterol; LDL-c- Low Density Lipoprotein Cholesterol
The men were taller and heavier as compared to women, but the BMI was significantly higher in women. The subjects were considered to be overweight and obese if their BMI was ≥25 kgm-2. The age specific prevalence of overweight and obese was significantly higher in females as compared to males after the age of 60 years (Fig. 2). Only 35.8% of the participants were in the normal weight range (BMI <25.0 kgm-2), whereas 47.5% were overweight and 16.4% were obese (≥ 30 kgm-2) (4). If WHO recommended criteria for Asian population (5) were used (BMI 23 kgm-2) for classification of normal and overweight, 84.5% were overweight or obese.

- Age and gender-specific prevalence of overweight/obesity, metabolic syndrome, dyslipidemia, hypertension, diabetes mellitus and coronary artery disease at baseline
Subjects were labeled hypertensive if their systolic blood pressure was ≥140 mmHg and/or the diastolic pressure was ≥90 mmHg, or if they were receiving anti-hypertensive medications (6). HTN grade I or above (6) was noted in 955 (44.3%) of the participants (Table 2). The prevalence of HTN increased with age and was higher in males as compared to females (Fig. 2), particularly in the age groups below 50 years.
| Disease | Males | Females | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % (n) | 95% CI | N | % (n) | 95% CI | N | % (n) | 95% CI | |
| Hypertension | 1340 | 48.1 (645) | 45.4-50.8 | 815 | 38.0 (310) | 34.6-41.3 | 2155 | 44.3 (955) | 42.2-46.4 |
| Diabetes Mellitus | 1330 | 17.2 (229) | 15.1-19.2 | 815 | 15.8 (129) | 13.3-18.3 | 2145 | 16.7 (358) | 15.1-18.2 |
| Pre-Diabetes | 1330 | 31.7 (422) | 29.2-34.2 | 815 | 25.4 (207) | 22.4-28.3 | 2145 | 29.3 (629) | 27.3-31.2 |
| Coronary Artery Disease | 1342 | 6.0 (81) | 4.7-7.3 | 817 | 3.0 (25) | 1.8-4.2 | 2159 | 4.9 (106) | 3.9-5.8 |
Fifty-four percent of the subjects had normal fasting and postprandial plasma glucose values (<100 and <141 mg/dl, respectively), whereas another 29.3% had pre-diabetes (impaired fasting glucose: fasting plasma glucose between 100 and 125 mg/dl or impaired glucose tolerance: postprandial glucose between 140 and 199 mg/dl). Three hundred and fifty-eight subjects (16.7%) had DM; the diagnosis was made if their fasting or postprandial plasma glucose was ≥125 or ≥200 mg/dl, respectively, or they were on antidiabetic medications. The prevalence of DM increased with age in both males and females (Fig. 2).
Participants were considered to have dyslipidemia if serum triglyceride was ≥ 150mg/dL and/or if HDL-c was <40 mg/dL in males and <50 mg/dL in females. Using this criterion, dyslipidemia was present in more than half of the subjects. There was a trend for decline in the prevalence of dyslipidemia with advancing age in male subjects only (Fig. 2).
Metabolic syndrome (MS) was diagnosed if any three of the following 5 were present (modified from Adult Treatment Panel III (6) criteria as waist circumference was not recorded in all subjects): (i) BMI ≥25.0 kgm-2 which was used as a surrogate for increased waist circumference; (ii) Systolic blood pressure >130 mmHg or diastolic pressure >85 mmHg; (iii) Serum triglycerides ≥150 mg/dL; (iv) Serum HDL-c <40 mg/dL in males or <50 mg/dL in females; and (v) Fasting plasma glucose >100 mg/dL. Using these criteria for clinical diagnosis, 46.6% of the subjects had metabolic syndrome. There was no gender difference in prevalence of MS. The prevalence of MS increased with age in male subjects only (Fig. 2).
CAD was defined to be present if an individual gave a history of pre-existent disease diagnosed by a cardiologist or had undergone an intervention for the same (angioplasty/coronary artery bypass grafting). It was also diagnosed if on the current evaluation, the echocardiography, ECG and/or TMT were compatible with the diagnosis in the opinion of a consultant cardiologist. The prevalence of CAD increased with age. It was significantly higher in males compared to females above 50 years of age (Fig. 2).
Changes in Baseline Characteristics on Follow-up
Gender specific changes in important parameters are shown in Table 1. Notably, there was a mild increase in weight, BMI and fasting plasma glucose in both males and females on follow-up. Height decreased significantly in females only. Diastolic blood pressure and postprandial glucose decreased significantly in both males and females, whereas LDL-c decreased significantly in males only. The number of patients taking antihypertensive and antidiabetic medication and lipid lowering drugs was significantly greater on follow-up (results not included in the Table).
Incidence of HTN, DM and CAD
Patients were followed-up for a variable period of time with a mean duration of 3.7±2.5 years for males and 3.5±2.3 years for females. The age-specific incidence of diseases was not calculated because of small number of subjects. The incidence of HTN, DM and CAD per 1000 person years follow-up was 72.2, 26.3 and 12.2, respectively (Table 3). The incidence of HTN and DM was lower in females but difference was not statistically significant except for incidence of pre-diabetes. It is noteworthy that the incidence of CAD in men and women was similar in this cohort of middle aged and elderly subjects, despite higher prevalence of disease amongst the males. On univariate analysis, the incidence of hypertension, CAD and DM increased with age, BMI, diastolic blood pressure and post-prandial glucose (Table 4). The proportion of subjects taking medications for HTN, DM and dyslipidemia increased significantly on follow-up (data not shown).
| Disease | Males | Females | Total | |||
|---|---|---|---|---|---|---|
| n/N* | Incidence (per 1000 person years) (95% CI) | n/N* | Incidence (per 1000 person years) (95% CI) | n/N* | Incidence (per 1000 person years) (95% CI) | |
| Hypertension | 192/692 | 75.4 (70.1-81.8) | 118/500 | 66.8 (61.7-72.8) | 310/1192 | 72.2 (68.2-76.2) |
| Diabetes Mellitus | 113/1070 | 29.0 (27.4-30.6) | 49/659 | 21.5 (20.1-22.9) | 162/1729 | 26.3 (25.0-27.2) |
| Pre-Diabetes# | 229/632 | 97.1 (89.9-105.3) | 103/450 | 64.0 (59.2-69.9) | 332/1082 | 83.8 (79.2-88.9) |
| Pre-Diabetes to Diabetes Mellitus+ | 86/306 | 81.4 (73.7-90.9) | 40/150 | 78.5 (67.3-94.2) | 126/456 | 81.0 (74.5-88.7) |
| Coronary Artery Disease | 56/1261 | 12.2 (11.5-12.7) | 34/792 | 12.4 (11.4-12.8) | 90/2053 | 12.2 (11.6-12.5) |
*n=number of subjects developing the event at the end of follow-up; N=number of subjects at risk for the development of event at baseline; # Incidence of Pre-diabetes amongst normoglycemic; +Incidence of diabetes amongst pre-diabetics
| Parameters | Incident Hypertension | Incident CAD | Incident Diabetes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | P-value | No | Yes | P-value | No | Yes | P-value | |||||||
| N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | N | Mean (S.D.) | ||||
| Age (years) | 882 | 44.0 (10.8) | 310 | 48.9 (10.5) | <0.001 | 1963 | 47.9 (11.4) | 90 | 53.3 (10.1) | <0.001 | 1567 | 47.0 (11.5) | 162 | 51.5 (10.7) | <0.001 |
| BMI (kg/m2) | 882 | 25.5 (3.5) | 310 | 26.9 (4.0) | <0.001 | 1963 | 26.2 (3.9) | 90 | 26.1 (3.3) | 0.2708 | 1567 | 26.2 (3.7) | 162 | 27.7 (4.2) | <0.001 |
| Diastolic Blood Pressure (mm Hg) | 882 | 75.5 (6.1) | 310 | 77.6 (6.2) | <0.001 | 1959 | 81.7 (9.9) | 90 | 81.8 (11.8) | 0.9207 | 1564 | 80.9 (9.9) | 162 | 84.1 (10.0) | <0.001 |
| Post Prandial Plasma Glucose (mg/dL) | 859 | 104.0 (45.7) | 301 | 117.2 (56.6) | 0.0001 | 1909 | 117.4 (59.1) | 89 | 134.1 (74.2) | 0.0098 | 1535 | 96.5 (27.7) | 161 | 134.1 (45.2) | <0.001 |
CAD- Coronary Artery Disease; BMI- Body Mass Index
Discussion
The prevalence of overweight and obesity, even by the western standards (BMI ≥25 kg m2), was high in this sample of subjects drawn from a relatively higher socioeconomic status. This, however, is comparable to several studies from India in urban populations. In conformity with earlier reports, we also observed higher prevalence of obesity amongst women compared to men (7-9). High BMI is associated with increased cardiovascular mortality globally. It has been reported that this association is rather weak in data from India (10, 11). This may in part be due to paucity of long term cohort studies examining this relationship. Pednekar et al (12) reported lowest mortality from all causes in Mumbai in the BMI group 25 to <30 kg m-2; only obese men >60 years of age had increased mortality. In our study, BMI was not significantly associated either with the prevalence of CAD at baseline or incident CAD during follow-up. Abdominal obesity did not emerge as a significant predictor of myocardial infarction in Interheart Modifiable Risk Score (13, 14).
The prevalence of HTN in the present study (44.3%) is higher than other reports on urban Indian subjects. In a meta-analysis of 25 studies on urban subjects from different parts of India, Anchala et al (15) reported a prevalence of 33.8% (95% CI 29.7-37.8). This, however, included all age groups above 18 years. Prevalence of HTN increases significantly with advancing age as noted by us as well (Fig. 2); this explains the higher overall prevalence of HTN in the present sample of subjects. The prevalence of HTN was significantly higher in males. Many authors have not reported gender-specific prevalence of HTN as they did not document significant differences. The incidence of HTN in the current cohort was 75.4 per 1000 person years for males and 66.8 per 1000 person years for females. However, in the community-based New Delhi Birth Cohort (NDBC) (16), over an average follow-up period of 7 years in a relatively younger group of subjects (mean age 29 years), the incidence of HTN was 42.4 per 1000 person years for men and 18.0 per 1000 person years for women. This lower incidence in NDBC is related to the age difference. Only 54.7% of the hypertensive subjects were aware of HTN at baseline. This lack of awareness of HTN is fairly common all over the world. Thus, overall estimates for the awareness of high blood pressure were 25.3% (95% CI 21.4– 29.3) for rural Indians; and 42.0% (95% CI 35.2– 48.9) for urban Indians in a meta-analysis (15).
The prevalence of DM in 16.7% of the subjects with an additional 29.3% having prediabetes is high, but in consonance with numerous other reports from India (2). The incidence of DM in the present study (26.3 per 1000 person-years) is comparable to the finding reported by Anjana et al (17) who observed the incidence to be 22.2 per 1000 person-years in a larger cohort of subjects from rural and urban areas of Chennai followed-up for 9.1 years (11,629 person-years of follow-up). Again, the incidence of DM amongst subjects with prediabetes at baseline in the present study (83.8 per 1000 person-years) is similar to the finding reported by Anjana et al (17) (78.9 per 1000 person-years). In the relatively younger NDBC the incidence for DM were 10.4 per 1000 person years for men and 5.2 per 1000 person years for women (16).
Several authors have reported the prevalence of CAD in India ranging from 3.212.6% over the past two decades. In a community-based survey, overall age-adjusted prevalence of CAD was reported as 3.5% (4.8% in men and 2.6% in women) in a recent report from Kerala (18). Chadha et al in 1990 reported the overall prevalence of 3.19% (3.95% in men and 2.53% in women) in a random urban sample of 13,723 adults in Delhi (19). The prevalence of CAD amongst women has been reported to be higher by certain authors (20-22). However, the electrocardiographic criteria for the diagnosis of CAD are inaccurate in women (23). The prevalence observed in our study (6.0% in men and 3.0% in women) is somewhat higher compared to the prevalence noted in community-based surveys (18, 19). There are few studies reporting the incidence of CAD in Indian subjects. The present study shows that with advancing age the incidence of CAD in women catches up with the incidence in men. This has been emphasized in a recent review on the subject (24). The incidence of CVD in a cohort of subjects with DM was reported to be 5.6 per 1000 person-years follow-up (25). This compares with the incidence of CAD as 12.2 subjects per 1000 person years noted in the present study after detailed evaluation with ECG, TMT and echocardiography for diagnosis of CAD.
The risk factors for the development of HTN, DM and CAD noted in the present study are well recognized. Apart from age, overweight/obesity was the single most important factor predicting leading to the HTN and DM. Further, increasing age in itself was also related to obesity (Fig. 2). Increasing age and dysglycemia were noted to be the most important factors related to development of CAD. These observations emphasize the urgent need for controlling the epidemic of overweight/obesity in India by instituting lifestyle interventions in susceptible populations.
This study is based on observations in subjects attending a tertiary care hospital, and is not community-based. Further, the subject population is derived from the relatively higher socio-economic status and this may not be the representative of the community at large. To this extent, the findings of the present study will need to be corroborated by larger community-based cohort studies representing various socioeconomic strata. We present the findings of the present study considering that there are few cohort studies looking at the incidence of HTN, DM, and CAD from India. The baseline observations are mostly retrospective and the period of follow-up is short and variable. Further, the follow-up has been done after usual interventions for the risk factors noted at the time of the initial evaluation. The ascertainment of CAD in this study was not always based on angiographic evidence of critical arterial narrowing or definitive procedures such as angioplasty or Coronary Artery Bypass Grafting (CABPG). Thus, a positive TMT or stress echo or stress thallium was considered consistent with CAD as opined by a senior cardiologist. Considering that these investigative procedures have significant false positive and false negative rates, our estimates of prevalence and incidence of CAD could be in some error.
The high prevalence of MS in the present study is similar to other reports. It is reported to vary from 8%-43% in men and from 7% to 56% in women around the world (26). Increase in prevalence of MS with increasing age has been reported by others (27). Gender had no influence on prevalence of MS, similar to the observations in the present study.
The present study for definition and follow-up of the cohort was not merely an observational study. After baseline evaluation, all subjects were individually counseled regarding diet, exercise, abnormalities detected, diagnosis made, pharmacotherapy if required, and need for follow-up. The observations made at the time of follow-up, therefore, are influenced by compliance with recommendations made at baseline. It was noted that both systolic and diastolic mean blood pressures showed a significant decline in both men and women on follow-up. The number of subjects using anti-hypertensive medications also increased significantly. It is well known that HTN in early stages results in few symptoms and therefore remains undetected. Similarly, post-prandial plasma glucose showed a significant decrease on follow-up, likely because of better control of DM by appropriate interventions. These findings suggest that routine health check-up in middle aged subjects may help in controlling some of the risk factors for cardiometabolic disorders.
Conclusions
The prevalence of obesity, HTN, DM and MS in this hospital-based sample of subjects undergoing preventive health check-up was high but comparable to other published reports. Urgent remedial public health preventive measures are required to curtail the emerging epidemic of cardiometabolic disorders.
Funding Source:
This study was funded by Indian Council of Medical Research (5/4/1- 16/08-NCD-II).
Acknowledgement
The study idea was conceived by Late Prof. Rajendra Tandon who also undertook the assessment of subjects for probable CAD, and financially supported by the ICMR. We are thankful for the inputs provided by Senior Research Fellow Ms. Harshita Sehra.
References
- Premature coronary artery disease in Indians and its associated risk factors. Vas Health Risk Management. 2005;1:217-225.
- [Google Scholar]
- Prevalence of diabetes and cardiovascular risk factors in middleclass urban participants in India. BMJ Open Diabetes Research and Care. 2014;2:e000048.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of risk factors for coronary artery disease in an urban Indian population. BMJ Open. 2014;4:e005346.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity: Preventing and Managing the Global Epidemic. In: Report of a WHO Consultation. Geneva: WHO; 2000. p. :894.
- [Google Scholar]
- Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157-163.
- [CrossRef] [PubMed] [Google Scholar]
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. . 2004;42:1206.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of obesity on cardiometabolic risk factors in Asian Indians. J Cardiovasc Disease Res. 2013;4:116-122.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163-170.
- [Google Scholar]
- Is obesity becoming a public health problem in India? Examine the shift from under - to overnutrition problems over time. Obes Rev. 2009;10:456-474.
- [CrossRef] [PubMed] [Google Scholar]
- Association between body mass index and cardiovascular disease mortality in east Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. Br Med J. 2013;347:5446.
- [CrossRef] [PubMed] [Google Scholar]
- Association between body mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719-729.
- [Google Scholar]
- Association of body mass index with all-cause and cause-specific mortality: findings from a prospective cohort study in Mumbai (Bombay), India. Int J Epidemiol. 2008;37:524-535.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART Modifiable Risk Score. European Heart J. 2011;32:581-590.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of stroke and coronary artery disease in Asia. Circ J. 2013;77:1923-1932.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170-1177.
- [CrossRef] [PubMed] [Google Scholar]
- I ncidence of cardiovascular risk factors in an Indian urban cohort: results from the New Delhi birth cohort. J Am Coll Cardiol. 2011;57:1765-1774.
- [Google Scholar]
- Incidence of diabetes and prediabetes and predictors of progression among Asian Indians: 10-Year follow-up of the Chennai Urban Rural Epidemiology Study (CURES) Diabetes Care. 2015;38:1441-1448.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of coronary artery disease and its risk factors in Kerala, South India: a community-based cross-sectional study. BMC Cardiovasc Disord. 2016;16:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological study of coronary heart disease in urban population of Delhi. Indian J Med Res. 1990;92:424-430.
- [Google Scholar]
- Prevalence of coronary heart disease and coronary risk factors in an urban population of Rajasthan. Indian Heart J. 1995;47:331-338.
- [CrossRef] [Google Scholar]
- Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J. 2002;54:59-66.
- [Google Scholar]
- Prevalence of coronary artery disease and coronary risk factors in an urban population of Tirupati. Indian Heart J. 2007;59:157-164.
- [Google Scholar]
- Comparison of methods to assess coronary heart disease prevalence in South Asians. Natl Med J India. 1997;10:210-213.
- [Google Scholar]
- Sex differentiation with regard to coronary artery disease. J Cardiol. 2013;62:4-11.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of cardiovascular diseases and associated risk factors among subjects with type 2 diabetes - an 11-year follow-up study. Indian Heart J. 2014;66:5-10.
- [CrossRef] [PubMed] [Google Scholar]
- The metabolic syndrome: prevalence in worldwide populations. Endocrinol Metabol Clinics America. 2004;33:351-375.
- [CrossRef] [PubMed] [Google Scholar]
- The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Archives Int Med. 2003;163:427-436.
- [CrossRef] [PubMed] [Google Scholar]





