Translate this page into:
NAMS task force report on Alcohol, substance use disorders, and behavioral addictions in India
*Corresponding author: Dr. Rakesh K Chadda, Chairperson, Professor and Head, Department of Psychiatry, Chief, National Drug Dependence Treatment Centre (NDDTC), All India Institute of Medical Sciences, New Delhi-110029. Email: drrakeshchadda@gmail.com; nams_aca@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: National Academy of Medical Sciences (India). NAMS task force report on Alcohol, substance use disorders, and behavioral addictions in India. Ann Natl Acad Med Sci (India). 2024;60:88–100. doi: 10.25259/ANAMS_TFR_04_2024
INTRODUCTION
Substance use disorders and behavioral addictions are growing public health problems all over the world, including India.1-4 Substances that are commonly used in India include tobacco (both smoked and smokeless forms), alcohol (beer, wine, spirit, toddy, etc.), cannabis (bhang, ganja, charas, etc.), and opioids (heroin, raw opium, Doda, pharmaceutical opioids, etc.). While many people use substances, some of them suffer adverse health consequences, develop dependence, and/or require help and treatment. Sometimes, certain rewarding behaviors like playing video games and gambling may become excessive and can lead to serious social, financial, and legal consequences. These excessive behaviors are manifestations of behavioral addictions, as the person finds it difficult to stop indulging in these behaviors despite acknowledging the harms caused by these behaviors.
Community-based surveys have suggested that substance use disorders and behavioral addictions affect a substantial proportion of the population. Among the substance users, some become regular users, exhibit problematic patterns of use, and a minority also develop substance dependence as depicted in Figure 1. Similarly, behavioral addictions may also affect a considerable proportion of the population, though a larger proportion may indulge in the behaviors in a nonaddictive manner.5,6 Many factors play a role in the development of problematic substance use among users. It is seen that the onset of substance use generally starts in adolescence, and multiple biological, psychological, and social factors play a role in the genesis of substance use disorders.

- Continuum of substance-related issues.
Substance use disorders and behavioral addictions can cause impairment of physical, psychological, social, and financial health at both individual and societal levels. The profile of substances being used has changed over time, as evidenced by the changing profile of patients.7 There has also been an increase in behavioral addictions, reflected by an increase in the number of adolescents presenting with addiction to Internet/gaming disorders.
Substance use is a risk factor for many noncommunicable diseases (NCDs) like hypertension, mental health problems, and malignancies.8,9 Thus, substance use and substance use disorders are likely to be encountered by a range of healthcare professionals and in various settings like routine outpatient, inpatient, wellness clinics, and emergencies. Injection drug use (IDU) is associated with increased rates of transmission of the human immunodeficiency virus (HIV), Hepatitis B, and Hepatitis C. Substance use disorders and behavioral addictions are found to be more commonly present along with other mental health conditions than expected by chance, and substance use disorders can worsen the course and outcomes of psychiatric disorders.
The high magnitude of substance use disorders and behavioral addictions call for a multipronged and multifaceted action. The approaches to addressing substance use disorders can generally be categorized into supply reduction (reduction of availability of substances), demand reduction (effective treatment of substance use disorders and awareness to reduce initiation of substance use), harm reduction (reducing the harms associated with substance use, without necessarily effecting cessation of substance use), and rehabilitation of individuals who have quit substance use to ensure they return to the mainstream of society. Services can be provided at the primary, secondary, and tertiary levels of care. Apart from therapeutic efforts, preventive efforts also have a major role in reducing the burden of substance use disorders and behavioral addictions. However, different organizations and entities are involved in addressing different aspects of addictive disorders. Hence, there is a need for convergence to jointly address the problem of substance abuse under a coordinating body.
Despite preventive approaches and availability of services, substance use disorders and behavioral addictions remain a serious problem at the community level in India. There is a need to further plan about means and measures to address the issue more coherently and effectively. Medical professionals have the expertise and responsibility to chalk out the manner in which addictive disorders can be better addressed in India. Thus, the present white paper, under the auspices of the National Academy of Medical Sciences (India), discusses the manner in which substance use disorders and behavioral addictions can be tackled better.
BACKGROUND
Medical professionals can play an important role in mitigating the effect of substance use disorders and behavior addictions in the general population. The NAMS, India, has taken the initiative to constitute a task force in this area to develop guidelines for various stakeholders for addressing the problem of substance use disorders and behavioral addictions in the Indian population. In pursuance of the meeting of NAMS held on 21st April 2022 and the constitution of a Task Force on Alcohol and Substance Abuse to develop a white paper to be submitted to the Government of India for improving the health intervention activities in the area of Alcohol and Substance Abuse, the objectives of the task force were laid out.
This white paper document discusses the extent of substance use disorders and behavioral addictions in India and offers a roadmap for policymakers to address these more effectively with the help of medically oriented interventions.
TERMS OF REFERENCE (TORS) FOR THE TASK FORCE
The main objectives of the Task Force are:
To identify the current status in the area of alcohol and substance use disorders and behavioral addictions
To identify the deficiencies that need to be addressed
To recommend the prevention of alcohol and substance use disorder and behavioral addictions and to make improvements in this field.
METHODOLOGY
The Task Force reviewed the current reports and data pertaining to substance use disorders and behavioral addictions in India. It then developed a consensus on the key observations and recommendations, taking into consideration the healthcare services and the varied social-cultural-economic contexts across the Indian landscape. The initial working draft was circulated among the Task Force members, and comments were sought. The working draft was modified based on the suggestions. Subsequently, an online meeting was held on 21st Sept 2022, in which the experts deliberated on the various aspects of the document. Further modifications were made to the document based on the inputs received from the experts.
OBSERVATION/CRITICAL REVIEW
Current situation in the country
Alcohol and other substance use and behavioral addictions constitute an important public health issue all around the world, including India. Several research endeavors have estimated the prevalence of substance use and substance use disorders in India. In this section, we present the magnitude of the problem based on reports from India.
The National Survey on Magnitude of Substance Use in India (2019), conducted by the National Drug Dependence Treatment Centre (NDDTC), All India Institute of Medical Sciences (AIIMS), New Delhi, has estimated the national and state-wise prevalence of substance use in the country.1 The survey has reported that alcohol is the most common psychoactive substance used by the Indian population. Nearly 15% of the population aged between 10 and 75 years consume alcohol. Converting these to absolute numbers, about 16 crore persons consume alcohol in India. The prevalence rate of alcohol use is much higher among men (about 27.3%) as compared to women (1.6%). The states with the highest prevalence of alcohol use, as per this survey, are Chhattisgarh, Tripura, Punjab, Arunachal Pradesh, and Goa. The types of alcohol commonly consumed in India include both country liquor and Indian-made foreign liquor. Among the 16 crore alcohol users, about 5.7 crore individuals were found to be problem users (i.e., experiencing some problems with the use of substances), and about 2.9 crore individuals were identified as dependent users [Figures 2 and 3]. This suggests that there are a large number of individuals with alcohol use disorders.
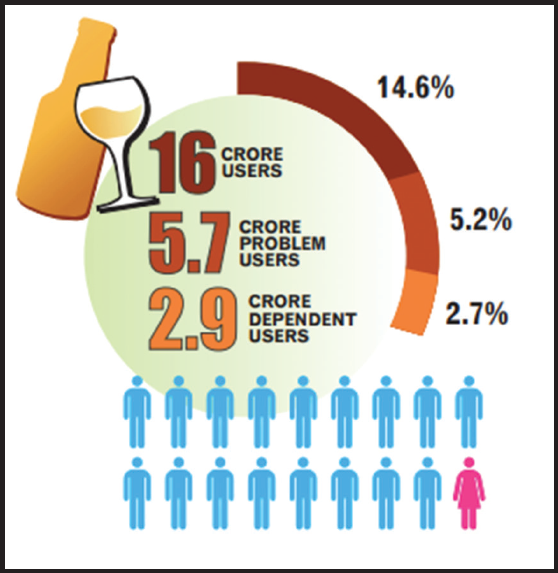
- Alcohol use in India.
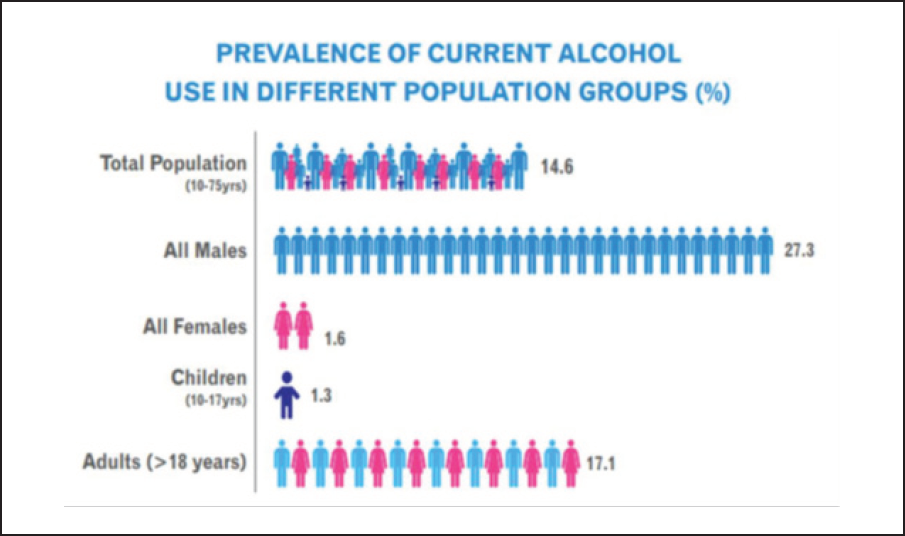
- Alcohol use in different population subgroups.
Cannabis use was reported by about 2.8% of the population. This translates to about 3.1 crore individuals reporting cannabis use in India. Different forms of cannabis used have also been assessed in this survey. About 2% of the population uses bhang (translating to about 2.2 crore individuals), and 1.2% of the population uses ganja and charas (translating to about 1.3 crore individuals). The states with the highest reported prevalence of cannabis use were Uttar Pradesh, Punjab, Sikkim, Chhattisgarh, and Delhi. There were about 72 lakh problem users and 25 lakh dependent users of cannabis across the country [Figure 4].
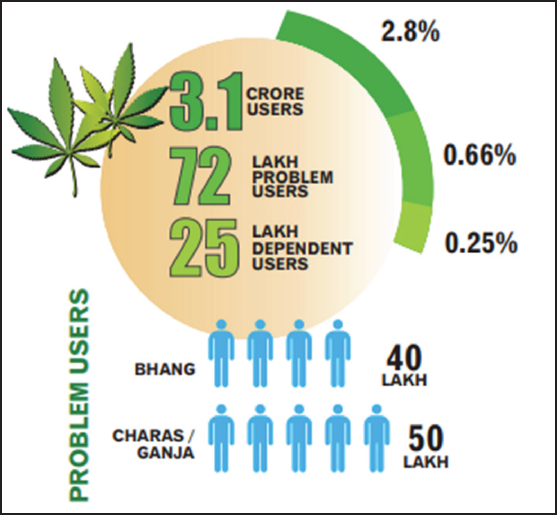
- Cannabis use in India.
Opioids were the next common substance of use. About 2.26 crore individuals, translating to about 2.1% of the country’s population, consume opioids. Heroin (1.14%), followed by pharmaceutical opioids (0.96%) and raw opium (0.52%), were the commonest opioids being used in India. The states with the highest prevalence of opioid use were Sikkim, Arunachal Pradesh, Nagaland, Manipur, and Mizoram (the prevalence of use in the general population was more than 10%). It was estimated that there were 77 lakh problem users of opioids, and about 28 lakh dependent users [Figure 5].
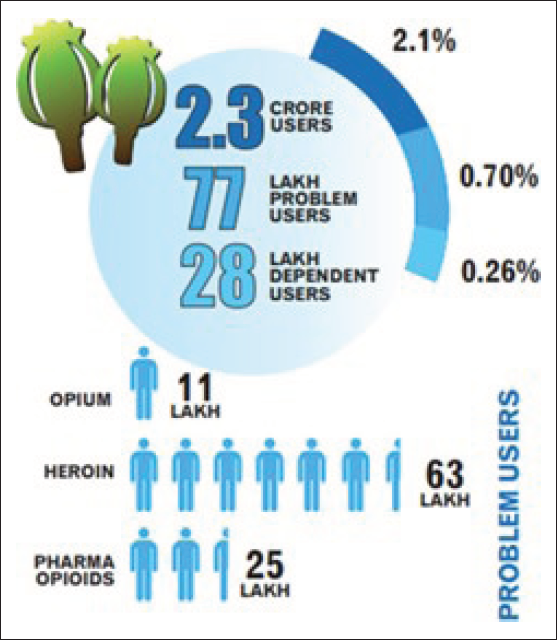
- Opioid use in India.
The survey estimated 1.08% of the population (translating to about 1.18 crore people) as current users of nonmedical and nonprescription sedatives. Sikkim, Nagaland, Manipur, and Mizoram have the highest prevalence of such sedative usage. Inhalant use was more common among children and adolescents (1.17%) than adults (0.58%). Other categories of drugs, such as cocaine (0.10%), amphetamine-type stimulants (0.18%), and hallucinogens (0.12%), were reported to be used by a smaller proportion of the population.
The National Mental Health Survey of India conducted in the years 2015–2016 has also presented the data on harmful and dependent use of alcohol and other substances.4 The prevalence of alcohol use disorders was found to be 4.7%, and the prevalence of other substance use disorders (apart from tobacco) was found to be 0.6%. The prevalence of tobacco use disorders was 20.9%. These findings also suggest a high prevalence of substance use disorders in the country.
The rates of tobacco use according to National Family Health Survey - 5 was found to be 38.0% among men and 8.9% among women, though this survey did not present the prevalence of tobacco use disorders per se.3 Similarly, the prevalence rate of alcohol use among men and women was reported to be 18.3% and 1.3%, respectively.
Of late, behavioral addictions have emerged as an important consideration in India as well.10 Among them, Internet addiction has drawn research attention across the different states of India.6 It has been estimated that about 20% to 40% of college students in India are at risk of Internet addiction. Similarly, gambling-related problems have been studied in the Indian context and there is evidence to suggest that 7.4% of college students indulged in problem gambling.5 Thus, behavioral addictions also need to be addressed from a policy and healthcare perspective in India. However, the literature on behavioral addiction has been limited, and representative national surveys are yet to be conducted on behavioral addictions.
Substance use disorders and behavioral addictions cause adverse health consequences, which result in disability and death. Ramalingam et al. (2022)8 showed that alcoholic liver disease led to more than 8,000 deaths in the National Capital Territory of Delhi in a single year starting in March 2017.8 The health-related expenditure due to alcohol was estimated to be about two times the revenue generated due to the sale of alcohol. Similarly, the Bangalore study suggests that alcohol use was associated with several familial and social adverse consequences, and the costs incurred due to alcohol use exceeded the revenue generated from alcohol.2,11
Taken together, there seems to be a high prevalence of substance use and substance use disorders in the country.12 Problematic substance use not only affects the person from a health perspective but also causes a burden to the family and society. Substance use can cause both direct and indirect harm to individuals and communities.
Current infrastructure, facilities, technologies, policies, programs, etc., in the country in the context of the problem/health issue
Care of people with substance use disorders can be at various levels, including primary, secondary, and tertiary care [Figure 6]. Primary care has the widest approach and is most easily accessible to individuals with substance use disorders.

- Care levels for people with substance use and behavioral problems.
A larger number of individuals can be helped at a lower level of care. As the severity of problems increases, the individual may need to be referred to a higher level of care.
Brief interventions at the primary care level can be of much use to elicit problematic substance use and to use the medical/clinical encounter for suggesting behavioral change and discussing methods of reducing or ceasing substance use.13 For example, a clinical encounter in the medicine/emergency department with a medical health problem can provide an opportunity to discuss cessation of alcohol use, which has led to gastritis/accident. Screening, brief intervention, and referral to treatment (SBIRT) can be utilized to screen and refer patients with more severe substance use disorders to the secondary level of care, and patients with complex needs can be referred to the tertiary levels of care.
Provisions of care can be through various approaches and settings:14-18
Public institutions – There is a wide array of medical and mental health services at primary, secondary, and tertiary care. Generally, patients with substance use disorders and behavioral addictions would have closer access to primary care. Much of the treatment of patients with substance use disorders, especially screening and identification, can be conducted in primary care.19
There are also specialized center and psychiatry departments in medical colleges for helping people with substance use disorders and behavioral addictions. NDDTC Ghaziabad, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh; National Institute of Dr. RML Mental Health and Neurosciences (NIMHANS), Bengaluru; RML Hospital, New Delhi; AIIMS, Bhubaneswar; and Central Institute of Psychiatry (CIP), Ranchi, are among the centrally supported institutions. Apart from that, there are several drug treatment clinics (DTCs) and addiction treatment facilities (ATFs) across the country. Medical colleges (centrally supported or supported through state governments) also provide care.
Private medical facilities – Many private medical facilities (both inpatient and outpatient) provide care for patients with substance use disorders. These facilities may be dedicated mental health facilities or general medical facilities. Counseling is also provided by independent practitioners from across the country. Alcohol, tobacco, and other substance-related harms may make individuals visit general healthcare facilities, and this can be an opportune moment to discuss cessation/reduction of substance use.
Nongovernmental organization (NGO) and not-for-profit sector – This sector also aims to reach out to patients with substance use disorders and provide care for them. There are a range of models of providing care, and these services tend to provide low-threshold services in the community. NGO and not-for-profit sectors provide a wide range of services varying from outpatient counseling services to long-term residential rehabilitation services. In addition, Alcoholics Anonymous and Narcotics Anonymous also provide mutual self-help 12-step facilitation among substance users.
Traditional and alternative systems of medicine – Many patients with substance use disorders approach traditional and alternative systems of medicine as well. Several interventions, like yoga, have demonstrated efficacy for patients with substance use disorders.
Digital and tele services – In the recent past, telephone and digital platforms have expanded in India. These offer an opportunity of reducing costs and make care more easily and immediately available. mHealth-based applications can be used through smartphones and can help in the reduction of substance use. Similarly, quitlines can provide counseling for the cessation of tobacco.
Figure 7 summarizes the range of services available for substance use disorders and behavioral addictions.

- Treatment service provisions.
Apart from services, prevention forms an important component of the approach to substance use and substance use disorders at the community level.20-25 Prevention aims at both educating the younger population about harms associated with substance use and emphasizing the measures available for addressing substance use. Other approaches for prevention rely on improving prosocial behaviors in the school setting, which has been shown to reduce substance use initiation. Workplace-based interventions have also shown promise for reducing substance use. Prevention measures can be universal, selective, or indicated, though universal approaches may have a wider reach and show greater impact. Prevention approaches that have shown a reduction in substance use among adolescents and young adults include increasing taxes on alcohol, brief alcohol screening, and intervention for college students, and workplace interventions.
Supply control measures may also have an impact on the use of substances like alcohol. Restrictions on the sale below a certain age, prohibition of the sale of alcohol in a particular area, control on the number of outlets, and taxation may also limit the consumption of alcohol, and hence the consequent harms.
Current policies:
National Policy on Narcotic Drugs and Psychotropic Substances
Current programs:
Drug De-Addiction Program under the Ministry of Health and Family Welfare, Government of India.
National Action Plan for Drug Demand Reduction under the Ministry of Social Justice and Empowerment, Government of India.
Nasha Mukt Bharat Abhiyaan under the Ministry of Social Justice and Empowerment, Government of India.
Current Budget
Ministry of Health & Family Welfare is running a National “Drug De-Addiction Program (DDAP)” with the objective of providing affordable, easily accessible, and evidence-based treatment for all substance use disorders through the government healthcare facilities and of building the capacities of healthcare staff in recognition and management of substance use disorders. The program is implemented through the health institutions under the Ministry of Health and Family Welfare (MoH&FW), viz., AIIMS, Dr.RML New Delhi; PGIMER, Chandigarh; NIMHANS, Bengaluru; RML Hospital, New Delhi; AIIMS, Bhubaneswar; and CIP, Ranchi. Out of these six, the center at AIIMS, New Delhi (NDDTC), is functioning as the National/Nodal center. The Ministry of Health and Family Welfare (MoHFW) has released the “Standard Treatment Guidelines for the Management of Substance Use Disorders and Behavioral Addictions”.18 The average annual budget of Rs. 45–53 crores has been allotted for DDAP Program for these above-cited DDAP Institutes in the last three years.
Ministry of Social Justice and Empowerment (MoSJE) implements the National Action Plan for Drug Demand Reduction (NAPDDR), which is an umbrella scheme under which financial assistance is provided to:
‘State governments/union territory (UT) administrations for preventive education and awareness generation, capacity building, skill development, vocational training, and livelihood support of ex-drug addicts, programs for drug demand reduction by states/UT, etc.’
“Non-Government-Organizations/Voluntary Organizations for running and maintenance of Integrated Rehabilitation Centers for Addicts (IRCAs), Community-based peer Led Intervention (CPLI) for early Drug Use Prevention among Adolescents and Outreach and Drop In Centers (ODIC) and Addiction treatment facilities (ATFs) in Government Hospitals”.
RECOMMENDATIONS
Key issues/gaps identified in the current situation in the country in the context of the problem/health issue
Despite having a considerable substance-using population, there is a large unmet treatment need pertaining to substance-use disorders in India. The National Survey on Magnitude of Substance Use in India suggests that only one in four persons with dependence on illicit substances receive treatment. For alcohol dependence, the rates were even abysmal, with only one in 38 individuals with alcohol dependence ever receiving treatment. The National Mental Health Survey of India found the treatment gap to be 86.3% for alcohol use disorders, 91.8% for tobacco use disorders, and about 73% for other drug use disorders (overall 90%). This emphasizes the fact that there is a much larger number of individuals with substance use disorders than those who seek treatment.
In addition, among those who seek treatment, many drop out of treatment due to various reasons. There could be many causes of drop-out from treatment, including inaccessibility of treatment, lack of motivation, logistical difficulties, peer pressure for discontinuation, and other reasons. Drop-out from treatment may be associated with relapse to substance use and recurrence of the problems associated with substance use. Thus, unplanned treatment cessations need to be focused upon so that the duration of abstinence from substances can be prolonged.
Treatment facilities for substance use disorders need to be expanded. Treatment for substance use disorders is provided through dedicated services through various channels. There is a need to expand the services so that it is accessible to individuals who need it. Providing such treatment at subsidized costs or free of cost or bringing it under the ambit of insurance coverage may make the care affordable to the patients.
There is also a need to expand the training and teaching in addiction psychiatry among medical graduates. Since alcohol dependence and substance use disorders are a common presentation in the clinical medical setting, clinicians need to be empowered to deal with these disorders. However, as of present, the attention to substance use disorders in the medical curriculum is limited. This forces medical graduates to “learn on the go” when they practice. Greater training of the medical graduates about substance use disorders and behavioral addictions is warranted.
There is a need to empower primary care physicians and other health professionals through training to enable them to screen substance use disorders and treat them. This might be done by providing clinical experience through case discussions and handholding in the initial period so that they become more attuned to the care of patients with substance use disorders in a routine manner.
Apart from training medical graduates, there is a need to train specialists in the field of addiction to provide care for patients with complex needs. Specialized training is also needed to develop a workforce of those who are able to train personnel for the treatment of addictive disorders.
Services of clinical psychologists, professionals from psychiatric social work, and professionals from psychiatric nursing can be utilized for the purpose of awareness, identification, and counseling of persons with substance use disorders.
Short-term courses (for example, under the Indira Gandhi National Open University-IGNOU) can be designed to increase human resources for counseling services and work at the community level. This would enable services to be provided at a larger scale to those who use substances or have issues related to behavioral addiction.
Furthermore, there needs to be efforts to enhance knowledge about substance use disorders in the general population. More awareness about these disorders, putting in the context of harms associated with them and the help available for treatment, would be helpful. Coupled with this, stigma reduction measures would help to de-stigmatize substance use disorders and enable greater acceptability of treatment.
While drawing and implementing policies, one has to consider the social needs and expectations. The perceptions of the community and their expectations should be factored while framing programs and implementation. Social marketing and social engagement need to be implemented to improve the outcomes of policies. The experience from previous programs has suggested that corrective measures may be required to improve community engagement and delivery of services.
Key issues/gaps identified in the current infrastructure, facilities, technologies, policies, programs, etc., in the country in the context of the problem/health issue
Key gaps in the current infrastructure, facilities, technologies, policies, and programs include:
Lack of adequate facilities and evidence-based treatment available to provide treatment for substance use disorder.
Lack of knowledge and skills in medical personnel to address substance use disorder
Different agencies to deal with different aspects of substance use disorders
Non uniform policies on alcohol
Lack of awareness regarding available treatment for substance use disorders and behavioral addiction
Lack of community support for treatment, support, and aftercare for people with substance use disorders
Lack of regulation of some centers that cater to people with substance use disorders resulting in the mistreatment of people with substance use disorders
Lack of due emphasis/focus on substance use disorders at the state level (which is responsible for health) in the midst of competing priorities.
Key issues/gaps identified in current financial inputs, etc., in the country in the context of the problem/health issue
While financial inputs are being provided for the treatment of substance use disorders, there needs to be a greater emphasis. Some of the further measures could be:
Dedicated outlays for evidence-based preventive measures
Greater government expenditure for sustaining services in the government sector
Dedicated budget for substance use disorders through telemedicine
Financial incentive for the provision of care to patients with substance use disorder in the NGO sector
Dedicated funds for incentivizing capacity development – trained primary care physicians, medical professionals, counselors, nurses, and other health professionals.
Funds for research need to be earmarked to find contextual solutions to the problems of substance use and behavioral addictions in India
WAY FORWARD
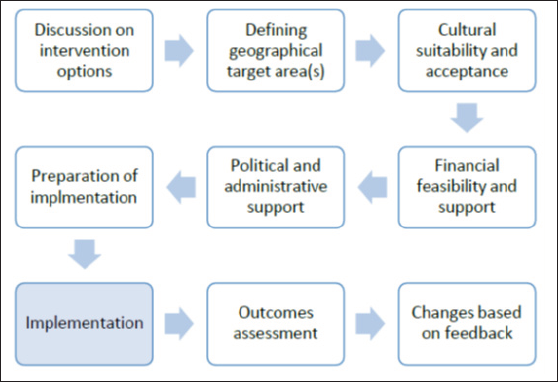
The way forward should include both preventive and curative aspects to address the problems of substance use and behavioral addictions. There is a need for clearly demonstrated efficacious measures, especially those that have been shown to be implementable in the country. Due to cultural and linguistic differences across the country, a multiple set of approaches might be useful to address the concerns of substance use disorders and behavioral addictions [Figure 8].

- Addressing substance use disorders and behavioral addictions in India.
Addressing substance use and behavioral addiction in India
Suggested policy activities and advocacy for policy makers
Working further toward a national alcohol policy in line with the WHO Global Strategy to reduce the harmful use of alcohol.
Relocation of all health-related activities for tobacco, alcohol, drugs, and behavioral addictions within the Ministry of Health and Family Welfare.
Framing policies to divert patients with substance use disorders with small quantities of recovered substances toward medical care in lieu of criminal proceedings and incarceration.
Sensitizing important stakeholders, including law enforcement authorities, and judiciary, on the need to distinguish drug users from drug dealers.
Telemedicine rules and guidelines should also facilitate the treatment of substance use disorders.
Enabling provisions to ensure the physical safety of healthcare providers at the workplace.
Advocating with policymakers on the need to ease the availability of medicines that are otherwise regulated under the Narcotic Drugs and Psychotropic Substances (NDPS) Act of 1985 and the need to protect the medical fraternity from inadvertent lapses in following processes/procedures in prescribing and dispensing medicines. This includes benzodiazepines that are needed for patients with mental illnesses.
Fund policy-related research activities on existing policies on substance use disorders and behavioral addiction, for example, the impact of banning alcohol in some regions/states, whether criminalization/decriminalization of some substances is the way forward, etc.
Recommendations for health/medical professionals
Training medical professionals and other healthcare providers about substance use disorders to enable screening and detection of substance use disorders and behavioral addictions at the primary/emergency care level.
Every patient who visits any health center or tertiary care center and has any of the above listed addiction habits should be counseled by the doctor at first instance and necessary referral should be provided by a psychiatrist in case a need arises.
Greater utilization of brief intervention and referral to the treatment of patients encountered in the medical setting who have problematic substance use at the primary level of care.
Optimum utilization of online training mechanisms for the training of medical professionals about substance use disorders and behavioral addictions. As a long-term goal, incorporate the Ministry of Health and Family Welfare-approved addiction psychiatry curriculum at the MBBS level.
Enable provision of basic treatment of substance use disorders and behavioral addictions at the primary care level.
Making a basket of services available to cater to the different needs of the population.
Greater access to treatment services like opioid substitution treatment for those who need such treatment.
Integrate psychosocial rehabilitation with medical treatment of patients with substance use disorders.
Training about addictive disorders at postgraduate levels in mental health and allied disciplines.
Suggestions to create awareness among general public, NGOs, and community stakeholders
Enhancing the awareness about substance use and the harms associated with it at the school and college levels. This includes not only medical harms and health deterioration but also mental health concerns and social consequences of substance use disorders.
Strengthening, implementation and monitoring of “Nasha Mukt Bharat Abhiyaan” could hold promise in preventive aspects.
Initiate workplace interventions for substance use problems in the workforce.
Sensitizing teachers in educational institutions about substance use for early identification and referral.
Target school and college students toward enhancing prosocial behaviors, to reduce substance use experimentation.
The key thrusts at policy, professional, and awareness levels are given in Figure 9.
- Key thrusts at policy, professional, and awareness levels.
The implementation plan would need more thorough deliberations with not only medical experts but also a multi-stakeholder approach, including individuals with substance use disorders, those with programmatic and administrative experience, financial experts, and others. The choice of strategies to be prioritized should be based on the evidence base and also the unique cultural, social, economic, and political landscape of the country. Social marketing should be considered while planning and implementing programs that address substance-related problems and behavioral addictions (Tiwari, 1998). The strategies selected should be linked to measurable outcomes evaluated on a suitable time frame basis. The objectives being defined by being specific, measurable, achievable, reliable, and time-bound would help to know whether the strategies have the intended effects. This would be beneficial in directing resources and better utilization of the inputs.
Further implementation plan is given in Figure 10.

- Further implementation plan.
ACKNOWLEDGMENT
We are grateful for the contributions from various domain experts in the field of substance use disorders and behavioral addictions and the Ministry of Health and Family Welfare. We are also thankful for the support from the National Academy of Medical Sciences (India). Our sincere thanks are also due to the various stakeholders working in the field of substance use disorders and behavioral addictions in India.
OPERATIONAL DEFINITIONS OF THE TERMS USED IN THE REPORT
Behavioral addiction – Syndromes related to repetitive rewarding behaviors that cause distress or interference with functioning.
Demand Reduction – Demand reduction means trying to prevent people from wanting to and taking illicit drugs.
Harm reduction – An approach to reduce the harmful consequences of drug use without necessarily reducing drug consumption.
Prevention (in the context of substance use disorder) – Process that attempts to prevent the onset of substance use or limit the development of problems associated with using psychoactive substances.
Substance use disorder – Involves patterns of symptoms caused by using a substance that an individual continues taking despite its negative effects.
Supply reduction – Supply reduction means using various strategies to disrupt the production and supply of illicit drugs.
LIST OF ABBREVIATIONS
AIIMS: All India Institute of Medical Sciences
ATF: Addiction Treatment Facility
CIP: Central Institute of Psychiatry
DTC: Drug Treatment Clinic
GOI: Government of India
IRCA: Integrated Rehabilitation Centers for Addicts
MoHFW: Ministry of Health and Family Welfare
MoSJE: Ministry of Social Justice and Empowerment
NAPDDR: National Action Plan for Drug Demand Reduction
NGO: Nongovernmental Organization
NIMHANS: National Institute of Mental Health and Neurosciences
ODIC: Outreach and Drop in Centers
PGIMER: Postgraduate Institute of Medical Education and Research
SUD: Substance Use Disorder
IMPORTANT DATA, STATISTICS RELATED TO THE ISSUE
Relevant data available from:
Ambekar A, Agrawal A, Rao R, Mishra AK, Khandelwal SK, Chadda RK. Magnitude of substance use in India. New Delhi: Ministry of Social Justice and Empowerment, Government of India. 2019. Murthy P, Manjunatha N, Subodh BN, Chand PK, Benegal V. Substance use and addiction research in India. Indian J Psychiatry. 2010;52(Suppl1):S189. National Family Health Survey – 5. 2019–21. India Fact Sheet. International Institute for Population Sciences. 2022. Available at http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf
REFERENCES
- Magnitude of substance use in India. New Delhi: Ministry of Social Justice and Empowerment, Government of India; 2019.
- Alcohol related harm: Implications for public health and policy in India, Publication No. 73. Bangalore, India: NIMHANS; 2011.
- 2022. 2019-21. India Fact Sheet. International Institute for Population Sciences. [accessed 2021 Jan 19]. Available from: http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf
- The National Mental Health Survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry. 2020;66:361-72.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-sectional study of problem gambling and its correlates among college students in South India. BJPsych Open. 2016;2:199-203.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of internet addiction among college students in the Indian setting: A systematic review and meta-analysis. Gen Psychiatr. 2021;34:e100496.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Changing pattern of substance abuse in patients attending a de-addiction centre in north India (1978-2008) Indian J Med Res. 2012;135:830-36.
- [PubMed] [PubMed Central] [Google Scholar]
- Health and economic burden due to alcohol-associated liver diseases in the Union Territory of Delhi: A Markov probabilistic model approach. Indian J Gastroenterol. 2022;41:84-95.
- [CrossRef] [PubMed] [Google Scholar]
- Self-reported medical co-morbidity among 400 substance using patients at an addiction unit in India. Journal of Substance Use. 2016;21:41-7.
- [Google Scholar]
- Service development for behavioural addictions: AIIMS experience. Ann Natl Acad Med Sci (India). 2017;53:130-38.
- [Google Scholar]
- Burden and Socio-Economic Impact of Alcohol — The Bangalore study. World Health Organization: Regional Office for South-East Asia; 2006.
- Substance use and addiction research in India. Indian J Psychiatry. 2010;52:S189.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Brief interventions for substance use disorders. Indian J Psychiatry. 2020;62:S290-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Substance use disorders: Need for public health initiatives. Indian J Soc Psychiatry. 2019;35:13.
- [Google Scholar]
- Need for psychosocial interventions: From resistance to therapeutic alliance. Indian J Psychiatry. 2018;60:S440.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Social marketing: A new approach in mental health research. Indian J Psychiatry. 1998;40:311-21.
- [PubMed] [PubMed Central] [Google Scholar]
- Standard Treatment Guidelines. Management of Alcohol Dependence. New Delhi: Ministry of Health & Family Welfare Government of India; 2017.
- [Google Scholar]
- New Delhi: Tobacco Control & Drug De-Addiction Programme Ministry of Health and Family Welfare, Government of India; 2020.
- Treatment of substance use disorders through the government health facilities: Developments in the “Drug De-addiction Programme” of Ministry of Health and Family Welfare, Government of India. Indian J Psychiatry. 2017;59:380.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tobacco control policies in India: Implementation and challenges. Indian J Public Health. 2011;55:220.
- [CrossRef] [PubMed] [Google Scholar]
- 2012 [accessed 2021 Jan 19]. Available from: http://dor.gov.in/sites/uploadfiles/revenue/files/NationalPolicyonNDPS.pdf
- Publication No. PEP19-PL-Guide-1 Rockville, MD: National Mental Health and Substance Use Policy Laboratory. Substance Abuse and Mental Health Services Administration; 2019.
- Global strategy to reduce the harmful use of alcohol. World Health Organisation: Geneva; 2010.
- 2021. Regional Office for the Eastern Mediterranean. Summary report on the regional technical consultation on the working document for development of the action plan (2022–2030) to effectively implement the global strategy to reduce the harmful use of alcohol as a public health priority, virtual meeting, 23 February 2021. World Health Organization. Regional Office for the Eastern Mediterranean. [accessed 2021 Jan 19]. Available from: https://apps.who.int/iris/handle/10665/351532
- International Standards for the Treatment of Drug Use Disorders: Revised edition incorporating results of field-testing. 2020.




