Translate this page into:
Quality of life outcomes in patients of genitourinary tuberculosis undergoing major surgical procedures: A single center experience
*Corresponding author: Dr. Aditya Prakash Sharma, Department of Urology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. Email: aditya.p.sharma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mandal S, Sharma AP, Chaudhary K, Aggarwal D, Devana SK, Mavuduru RS, et al. Quality of life outcomes in patients of genitourinary tuberculosis undergoing major surgical procedures: A single center experience. Ann Natl Acad Med Sci (India). 2024;60:151–6. doi: 10.25259/ANAMS-2023-3-10-(868)
Abstract
Objectives
In India, an estimated 18% of patients suffering from tuberculosis (TB), have Genitourinary tuberculosis (GUTB). Understanding the effect of GUTB on overall health and QoL is essential for providing better patient care and modifying health programs. The present study was designed to provide insight into the change in QoL in GUTB patients following surgical management using the World Health Organisation Quality of Life Brief Version (WHOQOL-BREF) questionnaire.
Material and Methods
A total of 35 patients, who underwent extirpative or reconstructive surgery at our center from January 2016 to December 2021 were included. Demographic profiles, clinical details, laboratory data, radiological imaging findings, and microbiological data were recorded from our database. To assess the impact of the disease and the subsequent surgical treatment, patients themselves completed the WHOQOL-BREF Hindi questionnaires twice, based on the recall method.
Results
The mean age of the study cohort was 36.89±12.64 years. Lower urinary tract symptoms (LUTS) were the most common (68.6%) presenting symptoms. Kidney alone or in combination with other organs was involved in all but six cases, amongst them three cases each exclusively involved the ureter and bladder only. Isolated kidney was involved in 7/35 (20%) patients. Preoperative diversion of the upper tract was needed in 27 patients. Nephrectomy was the most commonly performed surgery (48.6%) overall. Ileal conduit with cystectomy was the most frequently performed reconstructive surgery (14.3%). Amongst all the domains, preoperative mean physical and environmental domain scores improved from 51.08 ± 12.39 to 57.71 ± 14.53 and 55.37 ± 13.41 to 64.02 ± 16.59 after surgery, respectively.
Conclusion
GUTB significantly affects all domains, psychological and physical being the worst affected facets. With surgical treatment, improvement in overall QoL and its domains could be achieved.
Keywords
Genito-urinary Tuberculosis
Nephrectomy
Quality of Life
Tuberculosis
WHOQOL-BREF Questionnaire
INTRODUCTION
India has one of the highest burdens of tuberculosis (TB) worldwide. As per the Global World Health Organization-Tuberculosis (WHO TB) Report 2020, the incidence is 193 per 100,000 population.1 At present, a microbiological cure remains the litmus indicator for successful TB control services all over the world. Even though a gradually declining trend was noted, still around 10 million people were suffering from symptomatic TB globally in 2019.1 In India, of all the patients suffering from TB, an estimated 18% of patients have genitourinary tuberculosis (GUTB).2 GUTB causes significant morbidity as it causes multi-organ involvement. The disease and the treatment both cause considerable morbidity and consequently affect the Quality of Life (QoL) of these patients. Patient perceptions about the disease, sequelae of the disease, and its subsequent effect on QoL remained largely undetermined. It is important to understand the effect of GUTB on health and QoL to improve patient care and formulate health policies related to extrapulmonary tuberculosis.
Assessment of QoL in TB survivors is uniquely tricky as there is a lack of a validated TB-specific QoL calculator. There is difficulty in choosing pertinent control populations and a lack of descriptive and analytical data on the health status of the general population in many TB endemic areas. Therefore, self-reported health-related QoL is an important adjunct measure to understand and subsequently quantify the actual impact of GUTB on affected individuals.
The WHOQOL-BREF is a person-focused, multilingual tool for the subjective assessment of QoL. Its unique multi-dimensional profile enables it to be used in a wide range of diseases. It has four domains: physical, psychological, social, and environmental. The Hindi version of WHO QoL has been validated in the Indian healthcare setting, making it a valuable tool for assessing QoL in GUTB.3–5 The present study was designed to look into the changes in QoL in GUTB patients who have undergone major surgical procedures using the WHOQOL-BREF questionnaire.
MATERIAL AND METHODS
In this ambispective study, the electronic database was accessed for details of GUTB patients. Institutional ethics committee approval was obtained (IEC). Patients diagnosed with GUTB and undergoing extirpative or reconstructive surgery from January 2016 to December 2021 were included. Informed written consent was obtained from all the patients. All patients were diagnosed with GUTB based on one or more of the following criteria: microbiological, radiological, or clinical.
Clinical details, demographic details, laboratory parameters, radiological imaging findings, and microbiological data were recorded from our computer database. Any of the positive suggestive findings for GUTB from imaging such as intravenous pyelogram (IVP), micturating cystourethrogram (MCU), nephrostogram, non-contrast computerized tomogram (NCCT), or contrast-enhanced computerized tomogram of kidney ureter and bladder (CECT KUB) were noted. For microbiological diagnosis, acid-fast bacillus (AFB) smear positivity, Cartridge-based nucleic acid amplification test (CB-NAAT), TB- polymerase chain reaction (TB-PCR), or culture positivity in voided urine or urine from percutaneous nephrostomy (PCN) along with typical constellations of symptoms were considered. In the absence of any radiological or microbiological criteria, a history of symptom complex of GUTB was sought and further confirmation with histopathological evidence was done.
Quality of life was evaluated using the WHOQOL-BREF (Hindi variant) questionnaire (Annexure I). It is a truncated 26-item adaptation of WHOQOL-100, which initially had 100 questions. The Likert-type scale was used for scoring in the following four domains:
Domain 1: Physical health
Domain 2: Psychological health
Domain 3: Social relationships
Domain 4: Environment
Patients were called and given all necessary instructions. The change in QoL was assessed by administering the WHOQOL-BREF ( Supplementary File 1) questionnaire to the patients on two occasions based on the recall method. The raw scores obtained from the patients on the questionnaire were changed to the transformed score out of 100 in each domain as per the equations for computing domain scores provided by WHO ( Supplementary File 2). The first entry corresponding with the QoL before undergoing the surgical treatment, and the second one corresponding to the post-surgery period were noted. The median time to administration of the questionnaire was six months (range 3 months–12 months). Patients with missing values of more than 20% were excluded from the analysis according to the standard rule of the WHOQOL Group (the WHOQOL Group, 1995; World Health Organization, 1996).
Measures of central tendency like mean and median were used with measures of dispersion like standard deviation and interquartile range for continuous data. For qualitative data, frequency and percentage were analyzed. The normality of data was checked with Kolmogorov–Smirnov test and Shapiro–Wilk test. We then compared pre-treatment and post-treatment scores of all questionnaires with Student’s paired t-test and compared two means. All the data were analyzed by SPSS version 23 (SPSS Inc, Chicago, IL, USA). The raw scores were converted to transformed domain scores by using SPSS syntax (the scores are converted on a scale from 0 to 100 to enable comparisons between domains composed of unequal numbers of items). P-value ≤0.05 was considered significant.
RESULTS
Thirty-nine GUTB patients who met the inclusion criteria were screened, and four patients were excluded from the study because of the unavailability of adequate data. The pre-surgery questionnaire was filled prospectively in 21 patients, whereas 14 patients filled it using the recall method. Of the 35 patients interviewed, six (17.1%) patients had a history of pulmonary TB in the past and none had any evidence of active pulmonary Koch’s at the time of seeking treatment for GUTB. The mean age of the study cohort was 36.89 ± 12.64 years. More than 50% 18/35 (51.4%) of the patients were females. Lower urinary tract symptoms (LUTS) were the most common (68.6%) presenting symptom, followed by flank pain and hematuria [Table 1].
| Sl. No. | Parameter | Value (n = 35) |
|---|---|---|
| 1. | Age (years) (Mean ± SD) | 36.89 ± 12.64 |
| 2. | Sex | Male 17(48.6%), Female 18 (51.4%) |
| 3. | Weight (kg) (Mean ± SD) | 55.17 ± 13.13 |
| 4. | Height (cm) (Mean ± SD) | 159.74 ± 9.91 |
| 5. | Fever | 7 (20%) |
| 6. | Flank pain | 17 (48.6%) |
| 7. | Hematuria | 12 (34.3%) |
| 8. | Lower urinary tract symptoms | 24 (68.6%) |
| 9. | History of pulmonary tuberculosis | 6 (17.1%) |
| 10. | Comorbidity | DM - 2 (5.8%), HTN - 1 (2.9%), CKD - 1 (2.9%) |
SD: Standard deviation, DM: diabetes mellitus, CKD: chronic kidney disease, HTN: Hypertension, GUTB: Genitourinary tuberculosis.
Sterile Pyuria was present in 17 (48.5%) patients. Simple microscopy of voided urine identified AFB in 37.1% of patients. Simple microscopy, along with TB-PCR of voided urine, successfully diagnosed 62.8% of GUTB patients. PCN urine was exclusively positive for AFB in 11 (31.4%) patients. Eight (22.8%) patients had concomitant positive bacterial urine culture at the time of presentation. Escherichia coli is the most common (11.4%) organism responsible for concurrent urinary tract infection, followed by Enterococcus, Klebsiella, and Pseudomonas sp.
Isolated kidney was involved in 7/35 (20%) patients. The rest of the involved organ patterns are depicted in Table 2. A diuretic renogram revealed 18 of 35 patients having unilateral non-functioning kidneys (NFK) (non-visualized on a radionuclide scan) and another eight having poorly functioning kidneys (<10%).
| Sl. No. | Imaging | Finding with number (n = 35) |
|---|---|---|
| 1. | Organ involved |
Kidney only - 7 (20%) Kidney + Ureter - 10 (28.6%) Kidney + Ureter + Bladder - 11 (31.4%) Ureter only - 3 (8.6%) Urinary Bladder only - 3 (8.6%) Kidney + Bladder - 1 (2.9%) |
Preoperative diversion of the upper tract was needed in 27 patients. PCN was the most commonly performed procedure (62.8%). Double J Stent was placed in 5/35 patients. Various surgical procedures performed are depicted in Figure 1. Nephrectomy with excision of the affected ureter was the most commonly performed surgery (48.6%). Ileal conduit with simple cystectomy was the most frequently performed reconstructive surgery (14.3%). Clavien-Dindo grade 3 and 4 complications were not seen in any of the patients, whereas grades 1 and 2 were seen in three (5.7%) and four (11.4%) patients.
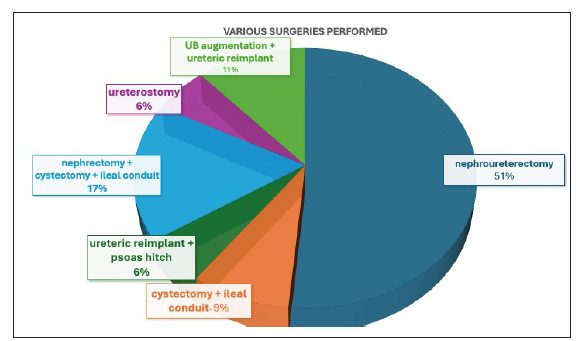
- Various surgeries performed in genitourinary tuberculosis patients.
All the domains in the WHOQOL-BREF score showed improvement following surgery. Physical and environmental domain scores significantly improved from 51.08 to 57.71 and 55.37 to 64.02 after surgery, respectively. Psychological and social domains also showed improvement in the postoperative period, but the changes were not statistically significant [Table 3]. The change of QoL scoring following surgery was analyzed with respect to organ involvement. Patients with bladder involvement showed statistically significant improvement in physical domain scores (p = 0.012) following surgery compared to patients with other genitourinary organ involvement. Change of score following surgery in psychological (p = 0.55), social (0.078), and environmental (0.414) domains did not show any significant difference with respect to organ involvement.
| Sl. No. | Questionnaire | Pre-treatment value (mean ± SD) | Post-treatment value (mean ±SD) | P-value |
|---|---|---|---|---|
| 1. | Physical domain score | 51.08 ± 12.39 | 57.71 ± 14.53 | 0.021 |
| 2. | Psychological domain score | 49.34 ± 15.68 | 54.31 ± 15.25 | 0.057 |
| 3. | Social domain score | 54.42 ± 18.54 | 61.08 ± 18.34 | 0.051 |
| 4. | Environmental domain score | 55.37 ± 13.41 | 64.02 ± 16.59 | 0.001 |
SD: Standard deviation
Surgery-wise distribution of QoL scores is provided in Table 4. Nine patients underwent cystectomy and urinary diversion (seven patients ileal conduit, one patient continent cutaneous diversion, and one orthotopic neobladder). The mean scores for all the domains pre- and post-operatively, respectively, are as follows: physical (45.6 vs. 73.7), psychological (48 vs. 56.2), social (52.8 vs. 75), and environmental (54.3 vs. 66). There was a statistically significant difference between the pre-and post-surgical scores for all the domains. On the contrary, the patients who underwent nephrectomy alone did not show a significant difference in pre-and post-surgical scores: physical (54.8 vs. 53.3), psychological (52.2 vs. 53), social (53.2 vs. 53.7), and environmental (57.9 vs. 64.8). Similar scores were observed for patients undergoing ureteric reimplantation [Table 4]. It is to be noted that many patients underwent more than one surgical procedure.
| Surgery | Physical (Pre vs. Post) | Psychological (Pre vs. Post) | Social (Pre vs. Post) | Environmental (Pre vs. Post) |
|---|---|---|---|---|
| Nephrectomy | 54.8 vs. 53.3 | 52.2 vs. 53 | 53.2 vs. 53.7 | 57.9 vs. 64.8 |
| Ureteric reimplantation/Ureteroureterostomy | 49.17 vs. 49 | 42.83 vs. 49 | 59.5 vs. 60.33 | 51.33 vs. 59/5 |
| Cystecomy + Urinary diversion | 45.6 vs. 73.7 | 48 vs. 56.2 | 52.8 vs. 75 | 54.3 vs. 66 |
| Augmentation cystoplasty | 47.25 vs. 53.25 | 45.25 vs. 51.5 | 48.25 vs. 68.75 | 48.75 vs. 67.25 |
Pre: pre-surgery scores, post: post-surgery scores
DISCUSSION
The focus of TB management in individuals with multi-organ involvement is targeted at giving a better QoL. Individuals afflicted with GUTB undergo significant changes in QoL due to the disease itself, treatment-related adverse effects and sequelae of the disease. Long-duration treatment schedules for months with multiple drugs, the need for urinary diversion, and reconstructive and extirpative surgical procedures affect patients in all domains of health and carry a lasting impact on the individual. Health-related quality of life (HRQoL) measures the repercussions of a disease on a patient’s day-to-day activities, functional state, behavior, and perceived health. HRQoL recently became more relevant in widening the concept of measuring health status beyond conventional indicators such as mortality and morbidity.6, 7
In this context, our findings highlight the improvement in post-treatment HRQoL of GUTB patients as measured by the WHOQOL-BREF questionnaire. In this study, we tried to find the effect of surgical intervention for GUTB on QoL. In two separate studies from Asian countries, it was seen that females were more affected in social domains,8 but in our study, patients of both genders were affected equally and improvement in QoL scores post-surgical intervention was comparable in both the sexes.
All the domains in the WHO-QoL BREF questionnaire revealed a set of low baseline scores. This could be attributed to the affliction by the disease itself and the delay in seeking treatment in our part of the world. End organ damage requiring nephrectomy in 51% of the patients reflects the delayed presentation on the part of the patients. This could be attributed to the poor socioeconomic status of the patients and lack of education. Extirpative and reconstructive surgeries were almost equally performed, simple nephrectomy being the most common surgery among all. The surgery was performed by Urology Consultants along with the senior residents with good experience in handling these cases. Most of the nephrectomy and nephroureterectomy were performed laparoscopically, while ureteric reimplantation, cystectomies with urinary diversion, and augmentation procedures were performed by an open approach. PCN was a more commonly used method of diversion as compared to Double J stent. This probably stems from the fact that these patients presented to emergency with infected hydronephrosis and PCN drainage was thought to be a better mode of diversion. Double J stenting was attempted in the majority of these patients. However, these patients had either obliterative strictures, renal pelvic scarring, or small capacity bladder, which precluded the retrograde or antegrade stent placement. Three of these patients had more than one PCN. Removal of these tubes itself is contributory to the improvement in QoL scores.
Even though the kidney was the most commonly involved organ, the QoL improvement following surgery was better seen with patients with bladder involvement. On further analysis, cystectomy and urinary diversion were found to be the surgery with the most profound effect. The same effect was observed in patients undergoing augmentation cystoplasty. Our findings imply that LUTS, the presence of catheters interferes with the QoL aspects of life significantly more than the symptoms arising from upper tract involvement. Rushing to the bathroom and the inability to travel and work due to LUTS or small capacity bladder leads to a significant impact on the QoL of these patients. The same is reflected in Table 4. Patients who underwent cystectomies or augmentation showed significant improvement in all the domains of QoL as compared to other surgical procedures. Although it is perceived that the application of a Conduit bag may lead to body dysmorphism, it was not noted in our cohort, as seen in Table 4. Also, it is notable that for surgeries such as nephrectomy and ureteric reimplantation, not much difference was found between the pre-surgery and post-surgery scores. Gender-wise, no difference was seen in terms of sexual function between males and females after cystectomy (73.8 vs. 76.5).
We found that the worst affected domain was the psychological domain. A wide arena of psychological reactions has been observed in patients with TB. Denial, worry about the diagnosis, depression, reduced sexual desire, tiredness, sleep cycle abnormalities, and anorexia are pretty common following diagnosis, and they mostly stem from fear of social retreat.9–12 More significantly, hospitalization and isolation of patients have been seen to have substantial emotional and psychological offshoots.11,13 Early identification and adequate treatment can dampen these psychological issues.
A study from South Africa on patients with pulmonary Koch’s used the Hospital Anxiety and Depression Scale (HADS) and showed that there was an improvement by +95% in both anxiety and depression domains, which led to a change from “moderate problems” to a state of “no problems”.14 Also, in our study there was an improvement of QoL in the psychological domain, but it did not reach statistical significance. Good empathetic communication and attention to minor details should be an inherent part of management, especially during diagnosis and treatment initiation. Adequate social and psychological support from family, friends, and community has been seen to give a better QoL to these patients.15 This social support and out-of-hospital care, which is usually lacking in our part of the world, needs to be strengthened further.
Physical functioning is a state which describes an individual’s capability to carry out daily activities self-care, and to fulfill the entitled and pre-desired roles at home, work, and in society. The diagnosis of tuberculosis in the family increases the workload on the family, especially on first-degree relatives, which further diminishes the caregiver’s capability.16 Physical domain scores in the preoperative period were also low in our study population, as mentioned previously, which subsequently improved in the postoperative period.
The environmental domain, which relates to the sense of safety, home environment, transport, and financial security, also showed significant improvement following treatment. Particular attention should be paid to culturally relevant and targeted interventions for TB-affected persons, especially in the early months of treatment, to integrate patients back into their communities as quickly and effectively as possible.
One of the essential dimensions affecting QoL in TB patients is secondary to the social blemish, which comes from family and the community.11,17 This stigma is even more prevalent in third-world countries. In one of the studies from urban Zambia, 82% of TB patients reported the fear of social seclusion at some point of the disease.18 Even though a lesser number was seen in a study from southern India, about 51% of patients felt the repercussions.19 In our study, we saw that the mean social domain score was affected, and even though it showed improvement in the postoperative period, it could not reach statistical significance. The appointed health personnel should be categorically trained to the special needs of these patients so that they can identify specific mental and physical health components and offer help. Primordial prevention can only come from promoting awareness, which can bring down the severity of social stigma. There is an urgent need to understand the origins of misbeliefs about TB and its curability with early interventions.
Patient-reported outcomes (PROMS) are the outcome of interest in most disease conditions. One such outcome is QoL, besides the physical health of an individual. Our study is the first of its kind that explored the QoL in a systematic way in patients suffering from GUTB. The limitation of our study is a component of recall bias in patients reporting pre-surgical QoL scores. Nevertheless, the study highlights the importance of patient-reported outcomes, especially of QoL, in patients suffering from GUTB as this is a prevalent disease in our part of the world and taking a step forward for out-of-hospital care for these patients.
Disease eradication is the latest goal of the National Tuberculosis Elimination Program (NTEP), but the disease and its treatment leave sequelae far outreaching inpatient care. Only bacteriological cure should not be the goal, but the ongoing programs should follow the participants till they fully recover health in all dimensions, allowing their complete return to society. At a higher level, policy strengthening, environmental protection, and livelihood interventions should be made.20 Outreach programs to educate and support TB patients, at-risk community members, and healthcare providers may prove useful.
CONCLUSION
Genitourinary tuberculosis significantly affects the QoL of the patients in all the domains with psychological and physical being the worst affected facets. The surgical management of GUTB improves both domain-wise and overall QoL. Bladder involvement causes the maximum deterioration of QoL and surgical procedures for the same have a maximum impact on QoL.
Ethical approval
Institutional ethics committee approval was obtained From Ethics Committee at PGIMER, Chandigarh. INT/IEC/2021/SPL-1194 dated 12/08/21.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Global Tuberculosis Report 2020. 2020.
- Current status of genitourinary tuberculosis: Presentation, diagnostic approach and management-single centre experience at IGIMS (Ptana, Bihar, India) Indian J Surg. 2020;82:1-7.
- [Google Scholar]
- WHOQOL-BREF Hindi questionnaire: Quality of life assessment in acetabular fracture patients. Indian J Orthop. 2015;49:323-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An assessment of the quality of life in hemodialysis patients using the WHOQOL-BREF questionnaire. Indian J Nephrol. 2008;18:141-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHOQOL-Hindi: A questionnaire for assessing quality of life in health care settings in India. World health organization quality of life. Natl Med J India. 1998;11:160-5.
- [PubMed] [Google Scholar]
- The WHOQOL-BREF: Translation and validation of the odia version in a sample of patients with mental illness. Indian J Soc Psychiatry. 2017;33:269.
- [Google Scholar]
- Validation of WHO QOL-BREF instrument in Indian adolescents. Indian J Pediatr. 2010;77:381-6.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of post-treatment health-related quality of life (HRQoL) among tuberculosis patients. Int J Tuberc Lung Dis. 2007;11:887-92.
- [PubMed] [Google Scholar]
- Perception and social consequences of tuberculosis: A focus group study of tuberculosis patients in Sialkot, Pakistan. Soc Sci Med (1982). 1995;41:1685-92.
- [Google Scholar]
- Psychosocial trauma of diagnosis: A qualitative study on rural TB patients’ experiences in Nalgonda district, Andhra Pradesh. Indian J Tuberc. 2013;60:162-7.
- [PubMed] [Google Scholar]
- Quality of life in tuberculosis: Patient and provider perspectives. Qual Life Res. 2004;13:639-52.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of tuberculosis patients about their physical, mental and social well-being: A field report from south India. Soc Sci Med (1982). 2005;60:1845-53.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing quality of life in patients with active tuberculosis. Health Qual Life Outcomes. 2004;2:58.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS one. 2017;12:e0174605.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The impact of social support on the health-related quality of life of adult patients with tuberculosis in Harare, Zimbabwe: A cross-sectional survey. BMC Res Notes. 2018;11:795.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Economic impact of tuberculosis at the household level. Int J Tuberc Lung Dis. 1999;3:596-602.
- [PubMed] [Google Scholar]
- Isolation and stigma: The experience of patients with active tuberculosis. J Community Health Nurs. 1999;16:233-41.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing the consequences of stigma for tuberculosis patients in urban Zambia. PLoS one. 2015;10:e0119861.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A cross-sectional study to assess the stigma associated with tuberculosis among tuberculosis patients in Udupi district, Karnataka. Indian J Tuberc. 2017;64:323-6.
- [CrossRef] [PubMed] [Google Scholar]
- The social determinants of tuberculosis: From evidence to action. Am J Public Health. 2011;101:654-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





